The human digestive system is a marvel of biological engineering, orchestrating a complex ballet of mechanical and chemical processes that sustain life. While the entire gastrointestinal (GI) tract plays an integral role in health, the upper digestive system is particularly significant, as it is the gateway through which food enters the body, is broken down, and begins the process of nutrient absorption. Comprising several vital organs and processes, the upper gastrointestinal tract forms the anatomical and functional foundation of digestion. Understanding the upper GI tract is not merely an academic exercise; it is a fundamental component of maintaining holistic wellness and preventing a wide range of health conditions. From nutrient assimilation to early immune responses and even mental health connections, the upper digestive tract influences more than most people realize.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
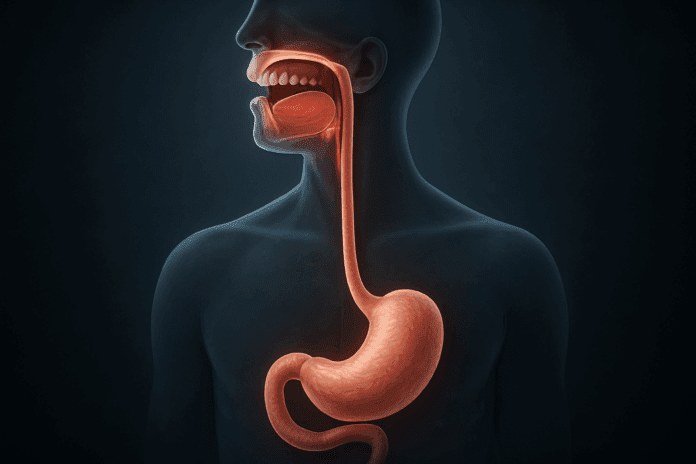
The Anatomy of the Upper Gastrointestinal Tract
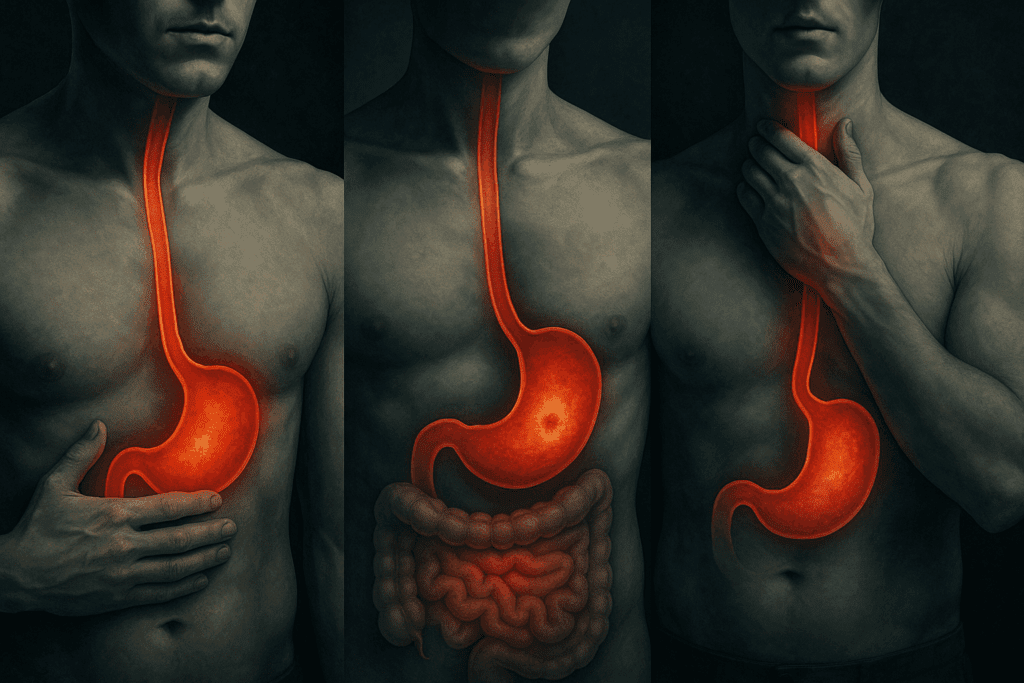
The term “upper gastrointestinal tract” refers to the anatomical section of the digestive system that includes the mouth, esophagus, stomach, and the first part of the small intestine, known as the duodenum. Each of these components plays a specific and interrelated role in digestion. The mouth initiates the process mechanically by chewing and chemically through enzymes in saliva, breaking down starches before food even reaches the stomach. The esophagus then serves as a muscular conduit, propelling food downward through coordinated muscle contractions known as peristalsis. Once food reaches the stomach, it encounters an acidic environment engineered to dismantle proteins and kill potentially harmful microbes. Finally, in the duodenum, enzymes from the pancreas and bile from the liver begin the complex task of emulsifying fats and further breaking down carbohydrates and proteins for absorption.
Understanding upper GI anatomy is essential for diagnosing and treating various digestive disorders. For example, recognizing how acid reflux stems from dysfunction in the lower esophageal sphincter offers clarity on the mechanisms behind heartburn and gastroesophageal reflux disease (GERD). Additionally, the anatomical layout helps explain why ulcers form in the stomach or duodenum and how structural abnormalities like hiatal hernias or strictures can interfere with normal digestive function. A working knowledge of upper GI organs is indispensable not only for medical professionals but also for individuals seeking to make informed decisions about their health.
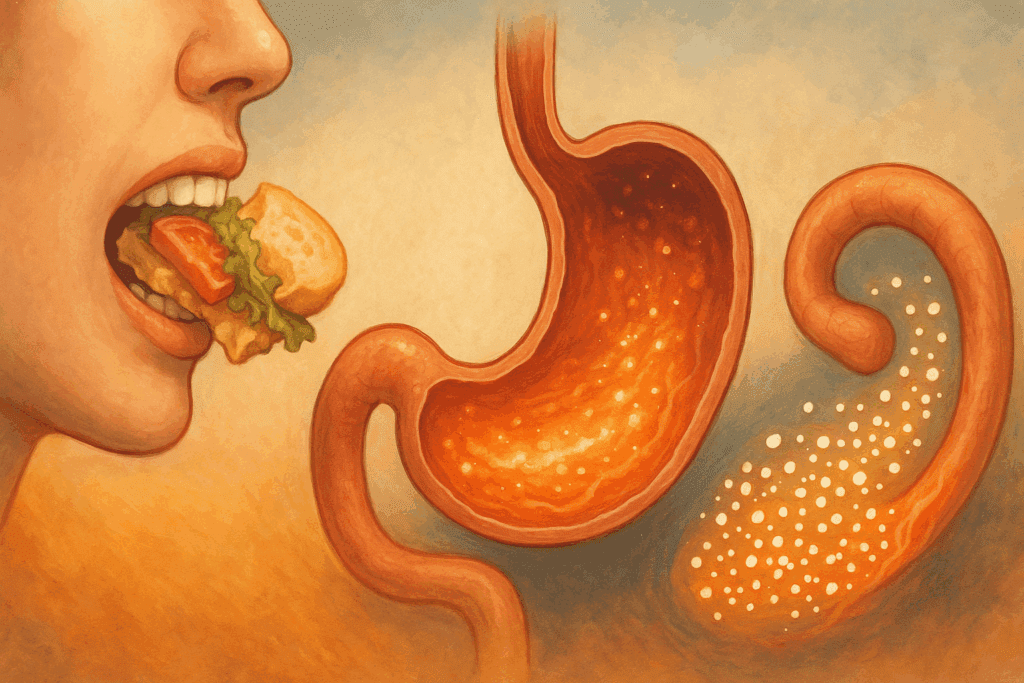
The Role of the Upper Digestive Tract in Nutrient Breakdown
The upper digestive system is not merely a passive channel but an active, dynamic environment where food undergoes essential transformations. Each organ in the upper GI tract contributes to the biochemical breakdown of nutrients, preparing them for absorption in the lower intestines. The salivary glands release amylase, an enzyme that begins the digestion of carbohydrates almost immediately upon chewing. This early intervention by the upper alimentary tract significantly reduces the workload for downstream organs, allowing for more efficient nutrient processing.
In the stomach, gastric glands secrete hydrochloric acid and the enzyme pepsin, which work synergistically to denature proteins and break them into smaller peptides. The acidic environment also facilitates the absorption of certain micronutrients such as vitamin B12, which requires intrinsic factor, a glycoprotein secreted by the stomach lining. As chyme—the semi-digested food mass—enters the duodenum, it encounters a surge of enzymes and bile that finalize the disassembly of fats, proteins, and complex carbohydrates.
The upper gastrointestinal system thus plays a critical preparatory role, ensuring that nutrients are in their simplest absorbable forms by the time they reach the lower intestines. Any disruption in this process—whether due to enzymatic deficiencies, reduced gastric acid, or anatomical issues—can lead to malabsorption, nutrient deficiencies, and related systemic problems. This makes the health of the upper GI tract central to the body’s nutritional economy.
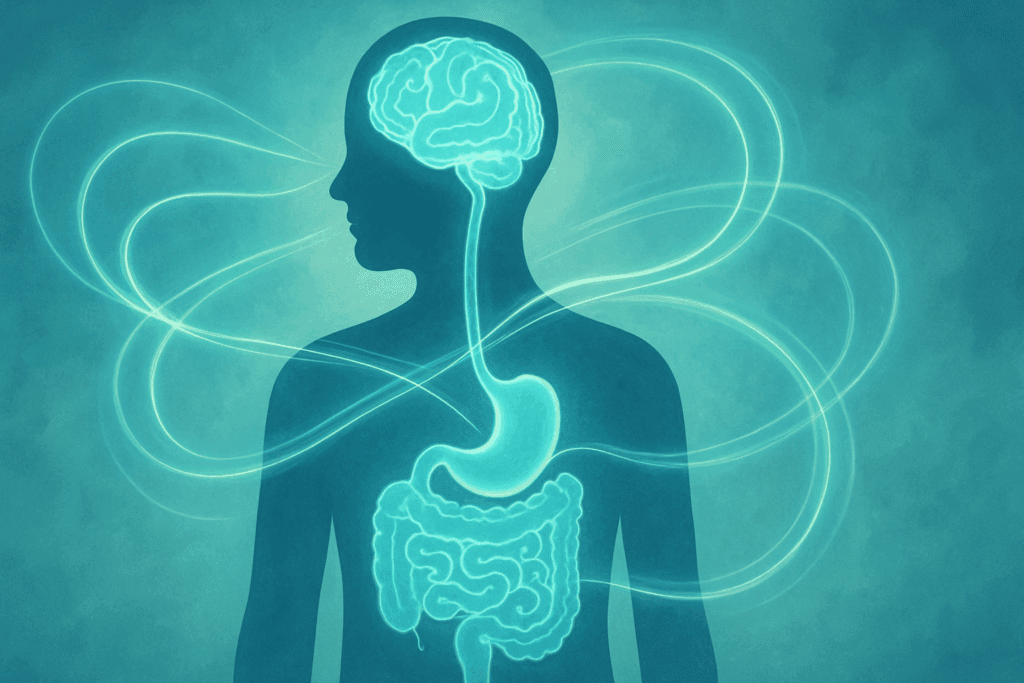
Upper GI Health and Its Impact on Mental Well-Being
Emerging research in the field of psychogastroenterology is shedding light on the intricate connections between the upper digestive system and mental health. The gut-brain axis, a bidirectional communication network linking the gastrointestinal tract with the central nervous system, begins its physiological messaging in the upper GI organs. Conditions like functional dyspepsia, which involves chronic discomfort in the upper digestive tract, often occur alongside anxiety and depression. The reciprocal nature of this relationship suggests that disruptions in upper GI function can both result from and contribute to psychological distress.
Furthermore, the upper gastrointestinal tract plays a role in regulating the production of neurotransmitters. For instance, the amino acid tryptophan—an essential precursor for serotonin synthesis—is first processed in the stomach and duodenum. If upper GI dysfunction impairs tryptophan absorption, it may compromise serotonin levels and contribute to mood imbalances. Stress and emotional distress, in turn, can alter gastric acid secretion, delay gastric emptying, and exacerbate symptoms like nausea or bloating.
Understanding this gut-brain interplay underscores the need for a holistic approach to mental health treatment that includes an assessment of upper GI health. Interventions like dietary adjustments, stress management techniques, and in some cases, targeted probiotic or enzymatic therapies can offer dual benefits for digestive and psychological well-being.
Common Disorders of the Upper Digestive System
A number of disorders affect the upper gastrointestinal tract, ranging from transient discomfort to chronic and debilitating diseases. Gastroesophageal reflux disease (GERD) is one of the most prevalent, characterized by the backward flow of stomach acid into the esophagus, leading to symptoms like heartburn, regurgitation, and chest pain. While GERD is often manageable with lifestyle modifications and medications, untreated cases can result in complications such as esophagitis, strictures, or Barrett’s esophagus, a precancerous condition.
Peptic ulcers represent another major concern, particularly when linked to Helicobacter pylori infection or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). These lesions form in the lining of the stomach or duodenum, leading to pain, bleeding, and potential perforation if left untreated. Functional dyspepsia, although not linked to structural abnormalities, involves persistent upper abdominal discomfort, early satiety, and nausea, and remains a diagnostic challenge due to its elusive etiology.
Other notable disorders include esophageal motility disorders such as achalasia, where the esophagus loses its ability to move food toward the stomach effectively. Conditions like gastritis, gastroparesis, and hiatal hernias also fall under the umbrella of upper GI disorders. The diversity and complexity of these conditions highlight the importance of recognizing symptoms early and seeking appropriate medical evaluation.
Diagnostic Tools for Evaluating Upper GI Function
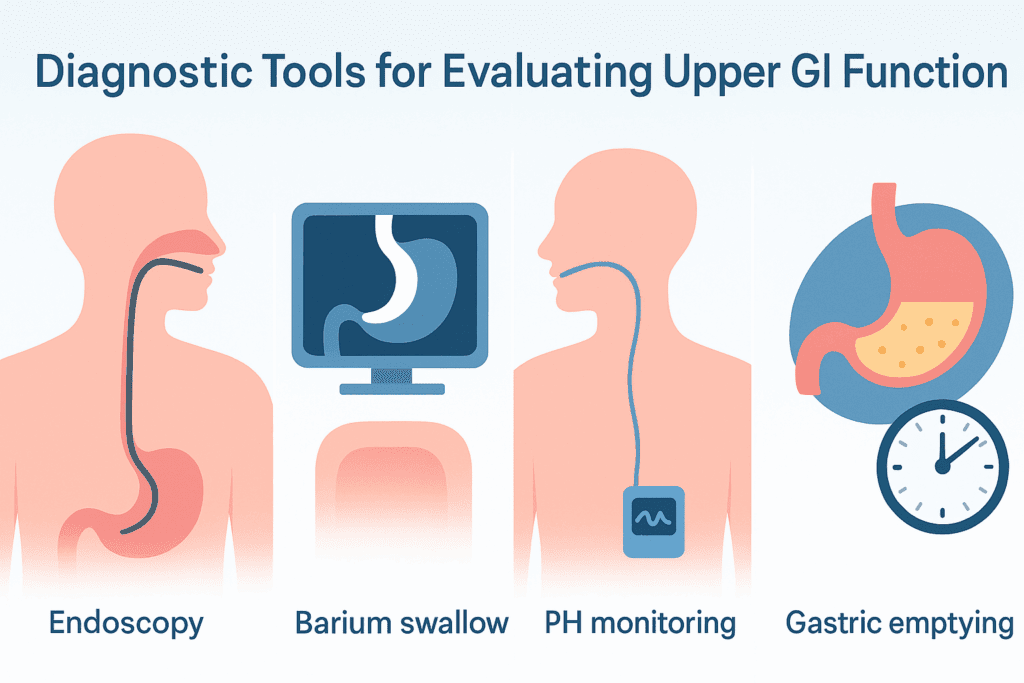
Modern medicine offers a wide array of diagnostic tools for evaluating the health and function of the upper digestive system. Endoscopy remains the gold standard, allowing direct visualization of the esophagus, stomach, and duodenum. This procedure not only aids in the diagnosis of conditions like ulcers, tumors, and esophagitis but also permits tissue biopsy for histopathological examination.
Another critical tool is the barium swallow or upper GI series, which involves swallowing a contrast dye to illuminate the structure and motility of the upper GI tract via X-ray imaging. This method is particularly useful for identifying strictures, hiatal hernias, or abnormal peristalsis. Gastric emptying studies assess how quickly food leaves the stomach, helping diagnose conditions like gastroparesis.
Advances in functional testing, such as esophageal pH monitoring and manometry, provide deeper insight into esophageal reflux and motility disorders. These technologies measure acid exposure and muscle coordination in the esophagus, offering valuable information for tailoring treatment strategies. With these diagnostic capabilities, clinicians are better equipped to pinpoint underlying issues and recommend effective interventions.

How Lifestyle Affects the Upper GI Tract
Daily habits play a powerful role in determining the health and efficiency of the upper gastrointestinal tract. Diet is one of the most influential factors; high-fat, highly processed, or excessively spicy foods can trigger acid reflux, slow gastric emptying, and disrupt enzyme activity. Conversely, diets rich in fiber, lean proteins, and fermented foods support optimal function across upper GI organs by promoting healthy microbial activity and ensuring smooth digestive flow.
Physical activity also influences upper digestive health. Regular moderate exercise helps stimulate peristalsis and gastric motility, reducing the risk of bloating, constipation, and indigestion. However, intense physical exertion immediately after eating may interfere with digestion by diverting blood flow away from the GI tract. Stress management is another critical lifestyle component, as chronic stress has been shown to impair gastric acid secretion and exacerbate symptoms in individuals with functional upper GI disorders.
Other behaviors, such as smoking and alcohol consumption, significantly affect the upper GI anatomy and its function. Smoking weakens the lower esophageal sphincter and impairs mucosal healing, increasing susceptibility to GERD and ulcers. Alcohol can irritate the gastric lining and delay gastric emptying, contributing to a range of digestive complaints. By understanding how lifestyle choices interact with the upper digestive system, individuals can make proactive decisions that promote long-term gastrointestinal health.
The Upper Digestive Tract and Systemic Health
The implications of upper digestive tract health extend far beyond the boundaries of the GI system. Impaired digestion at the upper level can set off a cascade of systemic issues. For instance, poor gastric acid production—a condition known as hypochlorhydria—can lead to the malabsorption of key nutrients like iron, calcium, magnesium, and vitamin B12. These deficiencies, in turn, are associated with anemia, osteoporosis, fatigue, and cognitive dysfunction.
Furthermore, the stomach and duodenum act as initial barriers against pathogens. The acidic environment in the stomach not only aids digestion but also serves as a frontline defense mechanism, neutralizing harmful bacteria and viruses before they reach the intestines. When this defense is compromised, the risk of gastrointestinal infections and downstream dysbiosis increases.
Research has also shown that chronic inflammation in the upper gastrointestinal system may contribute to systemic inflammatory states, potentially influencing the development of conditions like cardiovascular disease and autoimmune disorders. The interconnectedness of upper GI health with other bodily systems reinforces the importance of viewing digestive care as a cornerstone of comprehensive wellness.
Preventative Strategies and Medical Interventions
Prevention is the most effective strategy for maintaining a healthy upper digestive tract. Simple measures like eating slowly, avoiding overeating, and remaining upright after meals can significantly reduce the risk of reflux and indigestion. Incorporating fermented foods such as yogurt, kefir, and kimchi may help enhance the microbial environment of the upper GI tract and support better digestion.
When medical intervention is necessary, a wide range of treatment options is available. Antacids and proton pump inhibitors are commonly used to manage acid-related conditions like GERD and peptic ulcers. However, these medications should be used judiciously, as long-term use can interfere with mineral absorption and alter gut microbiota. Antibiotic therapy is often indicated for Helicobacter pylori infections, while prokinetic agents may be prescribed for motility disorders.
Endoscopic procedures can address structural issues like strictures or bleeding ulcers, and surgical interventions such as fundoplication may be considered in severe, treatment-resistant GERD. In all cases, a multidisciplinary approach that includes dietary guidance, behavioral counseling, and regular monitoring can yield the best outcomes. Early detection and intervention are key to preventing complications and preserving the integrity of upper GI function.
Maintaining Long-Term Upper GI Health: A Lifelong Priority
Supporting the health of the upper gastrointestinal system requires a proactive and sustained commitment. Regular checkups with healthcare providers, especially for individuals with a history of digestive issues, can catch emerging problems before they escalate. Being attuned to subtle changes in digestion—such as increased bloating, early satiety, or recurrent heartburn—can offer early warning signs that warrant investigation.
Mindful eating practices, such as chewing thoroughly and eating in a relaxed environment, can enhance enzymatic activity and improve digestive efficiency. Nutritional adequacy is another essential aspect; ensuring that the diet provides sufficient levels of vitamins and minerals helps prevent the cascading effects of malabsorption. Hydration also plays a critical role, as adequate water intake supports mucosal health and digestive flow.
In the modern health landscape, where fast-paced lifestyles often interfere with digestive rhythms, taking time to care for the upper alimentary tract is both a medical and psychological investment. Integrating digestive health into overall wellness strategies can help prevent disease, boost mental resilience, and enhance quality of life.
Frequently Asked Questions About the Upper Digestive System and Upper GI Tract
1. How can poor posture affect the upper digestive system?
Surprisingly, poor posture—especially slouching while eating or sitting for long periods—can significantly impact the upper digestive system. When you hunch over, it compresses the abdominal cavity and alters the natural alignment of the upper gastrointestinal tract, which can contribute to acid reflux, delayed gastric emptying, and even impaired esophageal motility. These mechanical changes may reduce the efficiency of food transit through the upper digestive tract and increase intra-abdominal pressure. Over time, such posture-related issues can compromise the function of key upper GI organs like the stomach and esophagus. Simple changes like sitting upright during meals and avoiding lying down immediately after eating can support healthier digestion across the entire upper alimentary tract.
2. What is the relationship between the upper GI tract and immune function?
The upper gastrointestinal system serves as a vital frontline in the body’s immune defense. The stomach’s acidic environment neutralizes many pathogens before they can reach the lower digestive system. Furthermore, the mucosal lining of the upper GI tract houses immune cells that participate in pathogen recognition and response. Conditions that alter gastric pH, such as chronic use of acid-suppressing drugs, may inadvertently increase susceptibility to infections like Clostridium difficile and small intestinal bacterial overgrowth. Supporting the immune aspects of the upper GI anatomy includes maintaining the balance of stomach acid and preserving mucosal integrity, both of which help ensure that the upper digestive system can fulfill its immunological role effectively.
3. Can upper GI health influence nutrient timing and energy levels?
Yes, the health of the upper digestive tract can influence how quickly and effectively nutrients are made available to the body. If the upper GI organs, particularly the stomach and duodenum, are not functioning optimally, nutrient breakdown is delayed, which can affect blood sugar regulation, satiety signals, and postprandial energy levels. For athletes or individuals with active lifestyles, a sluggish upper gastrointestinal tract can lead to poor nutrient timing, impacting performance and recovery. Optimizing upper GI anatomy through dietary practices, such as choosing easily digestible meals around physical activity, can enhance metabolic efficiency. Therefore, ensuring the smooth operation of the upper gastrointestinal system is crucial for sustained energy and metabolic balance.
4. How does aging affect the upper digestive system?
Aging introduces physiological changes that often impact the upper digestive system, including reduced saliva production, slower esophageal motility, and decreased gastric acid secretion. These changes can lead to difficulties in swallowing, altered taste perception, and increased risk of malabsorption—especially of key nutrients like calcium, B12, and iron. The muscular tone of the esophagus and stomach may also decline, affecting the peristaltic movements that help move food efficiently through the upper GI tract. Preventive strategies such as mindful eating, targeted supplementation, and regular medical evaluations can help mitigate these effects. Preserving the structural and functional health of the upper GI organs is essential for maintaining vitality and resilience in later life.
5. Are there gender-specific considerations in upper GI health?
Emerging research suggests that gender may influence both the presentation and prevalence of upper gastrointestinal conditions. For instance, functional dyspepsia and gastroparesis appear to be more common in women, possibly due to hormonal fluctuations affecting upper GI motility. Men, on the other hand, are more frequently diagnosed with GERD and Barrett’s esophagus. Differences in symptom reporting, stress responses, and pain perception may further complicate diagnosis and treatment. These patterns highlight the importance of considering gender as a factor when evaluating upper digestive tract symptoms, and tailoring interventions to align with hormonal, behavioral, and anatomical differences in upper GI system function.
6. What are some underrecognized signs of upper digestive tract dysfunction?
While heartburn and nausea are well-known symptoms, other subtle signs may point to upper digestive tract issues. These include chronic bad breath, frequent hiccups, unexplained anemia, and early satiety—feeling full after eating small amounts. Such symptoms often stem from underlying issues in the upper gastrointestinal system, such as delayed gastric emptying or silent reflux. These signs may be overlooked because they don’t always present alongside more obvious GI complaints. Being alert to these underrecognized symptoms can lead to earlier diagnosis and better outcomes for conditions affecting the upper alimentary tract.
7. How can travel and changes in routine impact the upper GI tract?
Travel often involves shifts in diet, sleep patterns, and stress levels—all of which can affect the upper digestive system. Jet lag and altered circadian rhythms may disrupt gastric emptying and acid secretion, while unfamiliar foods can challenge the adaptability of the upper gastrointestinal tract. Air travel in particular can cause gastric bloating due to cabin pressure, impacting comfort and digestion. To support upper GI organs during travel, it’s helpful to stay hydrated, eat light meals, and maintain regular movement. Understanding the vulnerability of the upper GI anatomy to lifestyle disruptions enables travelers to plan proactively and protect digestive function.
8. Are there connections between dental health and the upper GI system?
Yes, dental health and upper gastrointestinal function are more interconnected than they might appear. Poor oral hygiene or dental infections can introduce harmful bacteria into the upper digestive system via swallowed saliva. This can disturb the microbial balance and increase the risk of infections or inflammation in the upper GI tract. Additionally, compromised chewing efficiency due to missing teeth or jaw issues can strain the upper alimentary tract by increasing the burden on the esophagus and stomach to break down inadequately chewed food. Maintaining oral health is, therefore, a critical and often overlooked component of supporting a well-functioning upper gastrointestinal system.
9. How do emotional eating patterns affect upper GI health?
Emotional eating often involves consuming food rapidly, in large quantities, or during times of stress—all of which can negatively influence the upper digestive tract. These behaviors can trigger excessive acid production, increase the risk of reflux, and slow gastric emptying. Emotional distress also affects the enteric nervous system, which directly communicates with upper GI organs through the gut-brain axis. Repeated episodes of emotional eating can dysregulate normal digestive rhythms, causing persistent discomfort in the upper gastrointestinal system. Incorporating mindful eating practices and addressing underlying emotional triggers can significantly improve upper GI tract function over time.
10. What future technologies are emerging for upper GI diagnosis and care?
Several cutting-edge technologies are poised to transform how we evaluate and manage the upper digestive system. Capsule endoscopy now allows for non-invasive imaging of upper GI anatomy without the discomfort of traditional scopes. High-resolution manometry and impedance-pH monitoring offer detailed insights into esophageal motility and reflux episodes, even in atypical cases. Artificial intelligence is being integrated into diagnostic imaging to enhance early detection of abnormalities in the upper gastrointestinal tract. Moreover, wearable devices that monitor swallowing patterns and gastric activity are under development, potentially enabling real-time assessment of upper GI function. These innovations promise a more precise, patient-friendly future in upper GI care, aligning technological progress with the evolving needs of upper alimentary tract health.
A Final Word on the Significance of Upper GI Health in Total Wellness
Understanding the health and function of the upper digestive system is essential not only for addressing specific gastrointestinal concerns but for promoting broader physical and mental well-being. The upper GI tract serves as the entry point for nutrition, the initial battleground against pathogens, and an influential component in the gut-brain axis. When upper GI organs are functioning optimally, they enable efficient digestion, robust nutrient absorption, and a balanced internal environment that supports systemic health.
Conversely, when dysfunction occurs—whether due to lifestyle factors, infections, structural abnormalities, or stress—the effects can ripple outward, influencing immunity, cognition, and overall vitality. A comprehensive understanding of the upper gastrointestinal tract empowers individuals and clinicians alike to recognize early signs of imbalance, implement evidence-based interventions, and foster lasting wellness.
As science continues to unravel the interconnectedness of digestive and systemic health, the importance of maintaining a well-functioning upper GI system becomes ever more evident. By valuing and nurturing this foundational part of the body, we make an investment not just in digestion, but in the full spectrum of human health.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out
Further Reading:
Digestive System: Function, Organs & Anatomy
Your Digestive System & How it Works
Digestive Health – Digestive Tract, Accessory Organs, Motility