The human gut, often referred to as the “second brain,” plays a far greater role in emotional and cognitive health than many people realize. It’s no coincidence that stress and anxiety can manifest physically in the digestive system, producing symptoms that range from stomach cramps and bloating to an urgent need for a bowel movement. One particularly common yet under-discussed phenomenon is nervous poop, a term that describes the bowel urgency many people experience during moments of high stress or anxiety. While this may seem like an awkward or even humorous topic, it reflects a serious connection between the brain and gut that is grounded in complex physiological processes. For individuals dealing with anxiety poop episodes, understanding the root causes and learning how to stop nervous poop immediately can significantly improve daily quality of life.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
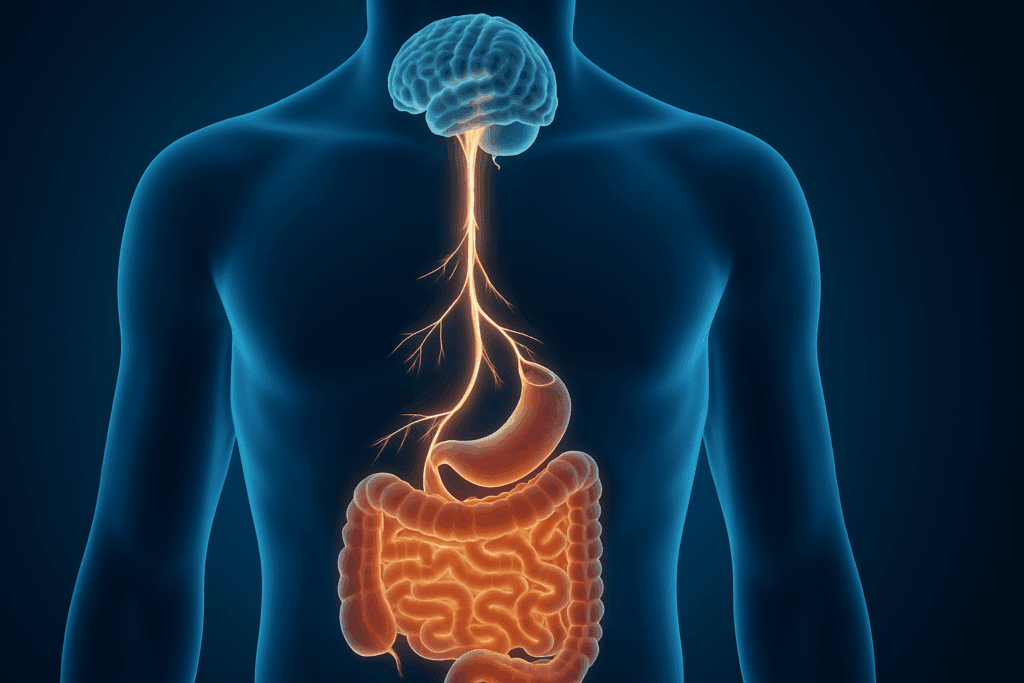
Understanding the Gut-Brain Axis: The Root of Nervous Poop
At the core of anxiety-related bowel changes is a bidirectional communication network known as the gut-brain axis. This intricate system involves neural, hormonal, and immunological signaling pathways that allow the brain and gastrointestinal (GI) tract to communicate constantly. One of the central players in this interaction is the vagus nerve, which acts as a two-way conduit, transmitting signals from the brain to the digestive system and vice versa. When a person experiences stress, the brain perceives a threat and initiates a cascade of physiological responses, including the activation of the sympathetic nervous system. This “fight or flight” response prepares the body to either confront or escape danger, and it often includes speeding up intestinal transit as a way to eliminate waste quickly in case physical exertion is required.
This mechanism explains why individuals who suffer from anxiety may also deal with nervous poop. During times of stress, neurotransmitters like norepinephrine and serotonin surge through the body. These chemicals influence gut motility, increasing the rate at which food moves through the intestines. As a result, the urge to defecate becomes more urgent, sometimes accompanied by abdominal cramping, loose stools, or diarrhea. Though this response is evolutionarily adaptive, in today’s world it more often becomes a source of social embarrassment and distress than a functional survival strategy.

The Role of Anxiety in Digestive Dysfunction
To understand why anxiety poop occurs, it’s essential to examine the broader impact of anxiety on the digestive system. Chronic anxiety disorders are associated with a range of gastrointestinal conditions, including irritable bowel syndrome (IBS), functional dyspepsia, and even inflammatory bowel diseases in more severe cases. Anxiety disrupts the normal rhythm of the enteric nervous system, often leading to irregular bowel movements and changes in stool consistency. Individuals who live with generalized anxiety disorder, social anxiety, or panic disorder frequently report digestive symptoms such as nausea, bloating, and unpredictable bowel habits.
These experiences are more than just physical inconveniences—they can create a feedback loop in which the anticipation of gastrointestinal distress triggers even more anxiety. This cyclical relationship can be particularly debilitating in social or professional settings, where the fear of an untimely bowel movement leads to increased physiological arousal, compounding the likelihood of experiencing poop anxiety disorders. In this context, nervous poop becomes not just a symptom but a trigger for worsening mental health, reinforcing the importance of a holistic treatment approach that addresses both emotional and physiological factors.
Differentiating Normal Stress Responses from Poop Anxiety Disorders
While occasional nervous poop is a normal response to high-pressure situations—like public speaking, exams, or first dates—it becomes problematic when it starts interfering with daily life. Poop anxiety disorders refer to a spectrum of conditions in which individuals develop an intense, sometimes irrational fear of having a bowel movement in public or inconvenient settings. This anxiety can escalate to the point where individuals avoid social events, travel, or even leaving their homes due to fear of digestive urgency.
Such conditions often overlap with psychological disorders, including agoraphobia, obsessive-compulsive disorder (OCD), and social anxiety. In many cases, the individual may not recognize the severity of their avoidance behaviors, attributing them to a “sensitive stomach” rather than an underlying anxiety condition. However, the pattern of preemptively using the restroom multiple times before leaving the house, obsessively mapping out bathroom locations, or carrying emergency supplies like extra underwear or medications can indicate a deeper issue.
Medical professionals often differentiate poop anxiety disorders by assessing both the frequency and intensity of symptoms, along with their impact on quality of life. Treatment usually involves a combination of cognitive behavioral therapy (CBT), gut-directed hypnotherapy, and sometimes pharmacological interventions such as selective serotonin reuptake inhibitors (SSRIs) that help regulate both mood and gastrointestinal function.
The Physiology Behind Urgency: What Happens in the Body During Nervous Poop
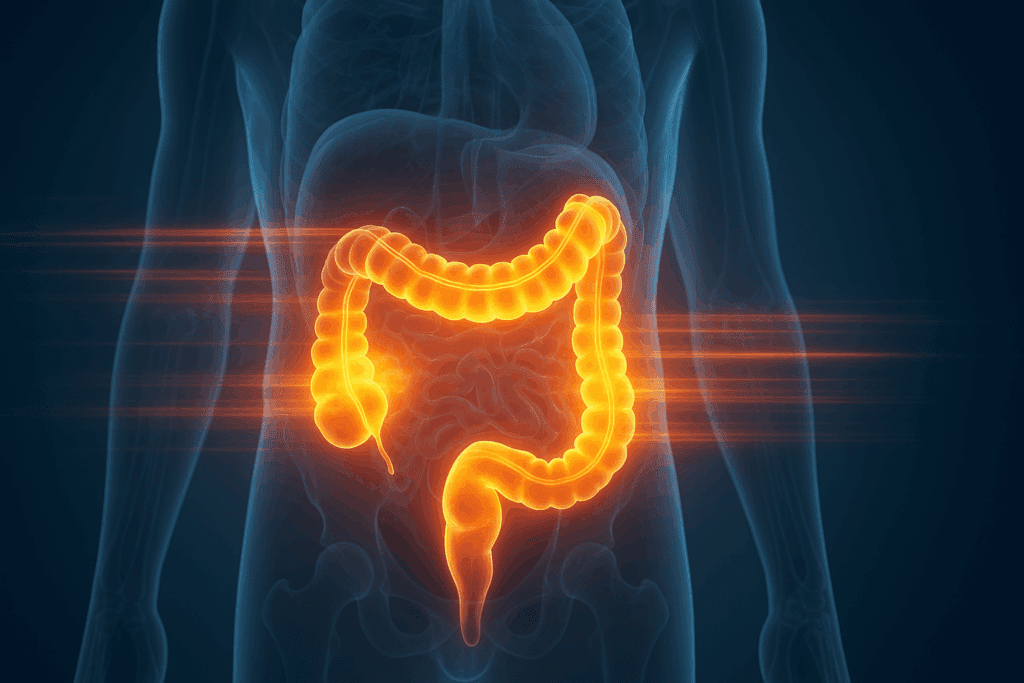
To fully grasp how to stop nervous poop immediately, it’s important to look closely at the physiological events that lead to urgency. When anxiety hits, the hypothalamic-pituitary-adrenal (HPA) axis springs into action, releasing cortisol and adrenaline into the bloodstream. These hormones are designed to increase alertness, raise heart rate, and mobilize energy stores. However, they also have secondary effects on the digestive system, including the inhibition of gastric emptying and the acceleration of colonic motility.
In simple terms, your body halts or slows digestion in the stomach while speeding up activity in the colon, creating an ideal scenario for loose, frequent stools. This response, while designed to serve a purpose during a true emergency, can become maladaptive in routine stress situations like morning commutes or job interviews. Over time, this chronic overactivation can lead to sensitization of the gut, making individuals more reactive to even minor stressors. As a result, people with anxiety may find themselves trapped in a pattern of hyper-awareness of bowel signals, which reinforces the nervous poop cycle.
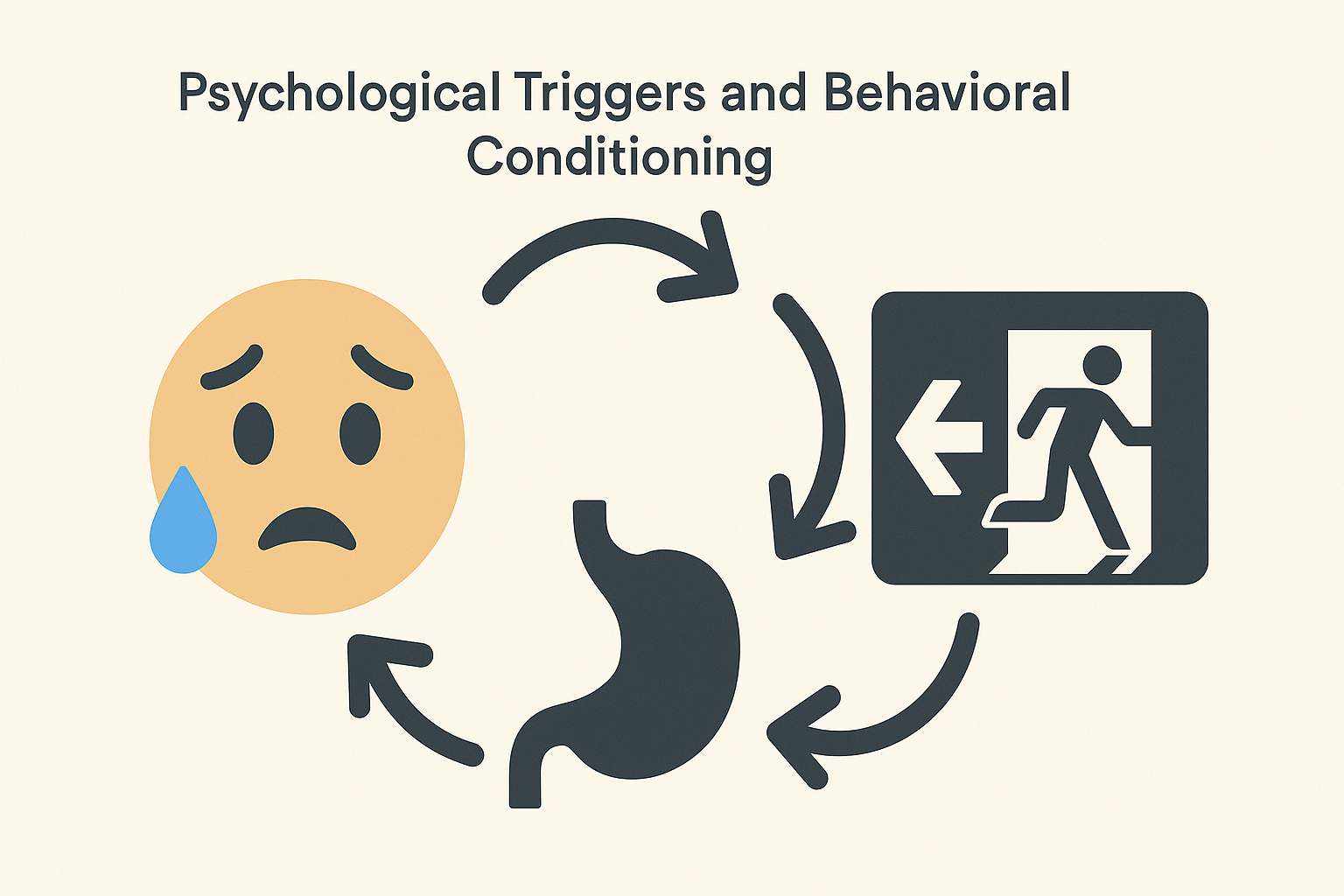
Psychological Triggers and Behavioral Conditioning
Beyond physiology, the mind plays a significant role in perpetuating poop anxiety disorders. Classical conditioning can create strong associations between specific settings—such as classrooms, elevators, or public transportation—and the sensation of needing to defecate. Even after the original stressful incident has passed, these environmental cues can trigger anticipatory anxiety and physiological arousal, mimicking the initial response.
Behavioral psychology explains that repeated avoidance of these triggers can actually reinforce anxiety over time. For instance, someone who once had a nervous poop episode before a job interview may begin to associate all professional events with digestive distress. The brain, seeking to protect against discomfort, activates the same neural circuits in similar contexts, even if the threat is no longer real. This makes the anxiety poop response more frequent and intense, further entrenching the behavior.
Effective treatment, therefore, must go beyond symptom management and address the underlying cognitive patterns and conditioned responses. Exposure-based therapy, mindfulness practices, and cognitive restructuring can help individuals break these associations and regain confidence in their ability to function without fear of digestive urgency.

How to Stop Nervous Poop Immediately: Evidence-Based Interventions
While long-term therapy is crucial for addressing the root causes of poop anxiety disorders, there are several immediate strategies that can help mitigate symptoms in the moment. First and foremost, breath control exercises can activate the parasympathetic nervous system, also known as the “rest and digest” system. Deep, diaphragmatic breathing reduces sympathetic arousal and helps relax the digestive tract, decreasing the sense of urgency.
Another effective approach involves progressive muscle relaxation (PMR), which reduces generalized tension and promotes bodily awareness. By systematically tensing and relaxing muscle groups, individuals can ground themselves in the present moment and redirect attention away from gastrointestinal sensations. For those seeking more discreet tools, certain over-the-counter remedies—like loperamide or simethicone—may offer temporary relief for diarrhea or gas-related symptoms, although they should not be used as a primary solution without medical supervision.
Dietary considerations also play a role in managing acute nervous poop episodes. Avoiding caffeine, spicy foods, and high-fat meals before a known stressor can minimize gastrointestinal stimulation. Similarly, staying hydrated and consuming soluble fiber can promote stool consistency and reduce urgency. These simple but effective measures offer individuals greater control over their bodily responses during high-pressure moments.

Lifestyle Strategies for Long-Term Relief
Preventing nervous poop over the long term requires more than crisis management—it calls for a sustained focus on overall mental and digestive health. Regular physical activity is one of the most effective ways to modulate stress and improve gut function. Exercise stimulates the release of endorphins, reduces cortisol levels, and enhances vagal tone, thereby improving both mood and gastrointestinal motility. Activities like yoga, walking, swimming, and strength training can all offer these benefits, especially when practiced consistently.
Equally important is sleep hygiene. Inadequate or poor-quality sleep disrupts the regulation of the HPA axis and increases sensitivity to stress, exacerbating both anxiety and digestive symptoms. Prioritizing consistent bedtimes, limiting screen exposure before sleep, and creating a restful sleep environment can have a significant impact on both mental and physical well-being. For those who struggle with insomnia, cognitive behavioral therapy for insomnia (CBT-I) offers a highly effective, evidence-based solution that improves sleep quality and reduces anxiety symptoms over time.
Nutritional strategies should not be overlooked. Probiotic-rich foods like yogurt, kefir, and fermented vegetables can support a healthy gut microbiome, which in turn modulates the gut-brain axis. Prebiotics such as oats, bananas, and garlic also nourish beneficial gut bacteria, helping to maintain microbial balance. Maintaining a regular eating schedule and avoiding skipped meals can further stabilize blood sugar and hormonal rhythms, reducing susceptibility to stress-induced gastrointestinal responses.
The Importance of Addressing the Stigma
Despite its prevalence, nervous poop remains a topic shrouded in embarrassment and social discomfort. This stigma can prevent individuals from seeking help, leading to prolonged suffering and unnecessary limitations in daily life. By normalizing the conversation and highlighting the physiological and psychological underpinnings of anxiety poop, healthcare providers and media outlets alike can play a role in destigmatizing this issue.
Open discussions in therapy, medical consultations, or even among peers can pave the way for more effective treatment and greater self-compassion. When individuals understand that their symptoms are not a reflection of personal weakness but rather a well-documented bodily response to stress, they are more likely to engage in proactive self-care and evidence-based interventions. Reducing the stigma surrounding poop anxiety disorders is not just a matter of social sensitivity—it’s a public health imperative.
When to Seek Professional Help
While occasional nervous poop is a common and manageable response to stress, there are times when professional help is warranted. If digestive symptoms are frequent, intense, or interfering with daily functioning, it’s important to consult with a medical professional. Gastroenterologists, psychologists, and primary care physicians can work collaboratively to assess the severity of the condition and recommend appropriate treatments.
Warning signs that may indicate the need for intervention include unintentional weight loss, persistent abdominal pain, blood in the stool, or changes in bowel habits that last longer than a few weeks. Additionally, if fear of bowel symptoms begins to dictate personal choices—such as declining social invitations or avoiding public transportation—it may signal the presence of a poop anxiety disorder that requires therapeutic attention.
A multidisciplinary approach often yields the best outcomes, incorporating medical diagnostics, dietary guidance, psychotherapy, and stress management techniques. With the right support, individuals can regain control over their digestive health and reduce the burden that anxiety places on both body and mind.
Frequently Asked Questions: Nervous Poop, Anxiety, and Digestive Health
1. Can nervous poop be triggered even when I don’t feel consciously anxious?
Yes, nervous poop can occur even when you’re not consciously aware of feeling anxious. This is because the body can react to subconscious stress cues through the gut-brain axis, especially if your nervous system has become sensitized over time. Many people experience gastrointestinal urgency in response to hidden stressors such as unresolved tension, suppressed emotions, or overstimulation from their environment. In these cases, anxiety poop is often a physiological reaction that seems to come out of nowhere, though it’s rooted in subtle psychological or neurological stress. This highlights why poop anxiety disorders sometimes develop without a clear traumatic event or memory—they can stem from patterns of chronic low-level stress and nervous system dysregulation.
2. Why does anxiety poop seem to hit right before important events or in the morning?
Morning urgency is a classic feature of nervous poop due to the body’s natural cortisol awakening response. Cortisol levels peak in the early hours, preparing the body for daily stressors, which can inadvertently stimulate the colon. When an important event looms—like a presentation, test, or meeting—the anticipatory anxiety activates this response even further. This overlap of hormonal, emotional, and neural stimulation explains why anxiety poop often strikes right before high-pressure situations. It’s not about digestion alone, but the body’s overall readiness and reactivity to potential threats, whether real or perceived.
3. Are there gender differences in how poop anxiety disorders present?
Emerging research suggests that poop anxiety disorders may manifest differently in men and women, partly due to hormonal differences and social conditioning. Women are more likely to report digestive symptoms like nervous poop in clinical settings, possibly because they are socialized to be more in tune with bodily discomfort. Men, on the other hand, may underreport anxiety poop due to stigma or cultural norms surrounding emotional expression. Additionally, fluctuating estrogen and progesterone levels throughout the menstrual cycle can exacerbate gut sensitivity, making anxiety-related bowel changes more frequent in women. However, poop anxiety disorders affect people of all genders and should be taken seriously regardless of how symptoms are expressed.
4. Is there a link between past trauma and anxiety poop patterns?
Yes, individuals with a history of trauma—especially those involving medical procedures, bodily autonomy, or public humiliation—are at higher risk for developing poop anxiety disorders. Traumatic memories can become somatically encoded in the nervous system, meaning that future stress may trigger digestive responses associated with earlier experiences. For instance, someone who had a distressing bathroom incident in childhood may unconsciously re-experience those emotions in similar settings later in life, resulting in nervous poop without understanding why. Trauma-informed care can be essential for these individuals, as traditional GI treatments alone may not resolve the underlying psychological distress.
5. What role does technology and screen time play in nervous poop or anxiety poop?
Although not often discussed, excessive screen time can indirectly contribute to anxiety poop through several mechanisms. Constant digital stimulation can increase baseline stress levels by keeping the nervous system in a state of alertness, particularly through social media, email, or news exposure. Blue light from screens also disrupts circadian rhythms, which affects both mood and digestion. When people use their phones excessively during bathroom time or before bed, they may reinforce hypervigilance around bowel habits, intensifying poop anxiety disorders. Taking intentional digital breaks and practicing screen hygiene can reduce this sensory overload and help recalibrate the gut-brain connection.
6. How does travel exacerbate poop anxiety disorders?
Travel often acts as a catalyst for nervous poop due to disrupted routines, unfamiliar environments, and fear of public restrooms. People with poop anxiety disorders may experience heightened bowel urgency on flights, in hotels, or while commuting, not because their digestion is inherently weaker, but because their sense of safety is compromised. This lack of predictability makes the body hyperaware of internal cues, leading to frequent bathroom scans and avoidance behaviors. Strategies to manage travel-induced anxiety poop include pre-planning meals, packing familiar digestive aids, and practicing calming routines before departure. Repeated positive travel experiences can also help rewire anxious associations with being away from home.
7. Can diet alone cure nervous poop or anxiety-related bowel symptoms?
While a balanced diet can significantly reduce digestive discomfort, diet alone rarely resolves the root causes of anxiety poop. Many individuals focus exclusively on food triggers like caffeine, dairy, or FODMAPs, hoping to eliminate nervous poop through elimination diets. However, poop anxiety disorders are more neurologically than nutritionally driven, and dietary adjustments may only provide partial relief. In fact, hyperfixating on food can sometimes worsen symptoms by increasing fear and rigidity around meals. A more effective approach involves combining mindful nutrition with stress-reduction strategies, such as CBT or vagus nerve stimulation exercises, to address both gut and brain inputs.
8. Are there emerging treatments or research trends targeting anxiety poop specifically?
Yes, recent advances in psychogastroenterology have led to more integrated treatments for anxiety poop, including gut-directed hypnotherapy and virtual reality exposure therapy. These methods focus on recalibrating the gut-brain communication channels using cognitive and sensory retraining. Researchers are also investigating the gut microbiome’s role in modulating anxiety and poop frequency, leading to interest in psychobiotics—probiotics with targeted mental health benefits. In parallel, neurofeedback therapies that train the brain to manage stress more efficiently are showing promise in individuals with severe poop anxiety disorders. These innovations represent a shift toward multidisciplinary care, where both psychological and physiological factors are addressed in tandem.
9. How can I build more confidence in social settings despite experiencing nervous poop?
Rebuilding confidence after dealing with anxiety poop requires both mindset work and gradual exposure. Cognitive techniques such as reframing catastrophic thoughts (e.g., “What if I can’t find a bathroom?”) into more balanced statements (“I’ve handled this before, and I know my coping tools”) can reduce anticipatory dread. Practicing non-reactivity—allowing bodily sensations to arise without panicking—also diminishes the power nervous poop holds over your self-esteem. Building up your tolerance in safe social settings, such as with trusted friends, allows you to desensitize gradually to public environments. Over time, this reduces avoidance behaviors and restores trust in your body’s ability to function calmly under pressure.
10. What’s the long-term outlook for someone living with poop anxiety disorders?
The long-term outlook for people with poop anxiety disorders is optimistic, particularly with early intervention and personalized care. Many individuals experience significant symptom reduction through a combination of therapy, lifestyle modifications, and medical support. While nervous poop may never disappear entirely, its intensity and frequency can become manageable to the point that it no longer dictates daily decisions. Resilience grows with each successful navigation of challenging situations, reinforcing the nervous system’s ability to adapt. With time, people often discover that they’re not only capable of managing anxiety poop—they’re stronger, more self-aware, and more empowered because of it.
A Final Word on Managing Nervous Poop and Reclaiming Confidence
Understanding the phenomenon of nervous poop sheds light on the profound interplay between mental health and gastrointestinal function. Far from being an isolated or quirky response, anxiety-related bowel changes reflect a deeply rooted connection within the gut-brain axis. For those grappling with anxiety poop or more entrenched poop anxiety disorders, recognizing the legitimacy of these experiences is the first step toward effective management.
Fortunately, a combination of immediate relief strategies, long-term lifestyle changes, and professional interventions can offer meaningful relief. Whether it’s through breathwork, dietary adjustments, cognitive restructuring, or structured therapy, the tools exist to help individuals stop nervous poop immediately and regain a sense of control over their lives. By addressing this issue with compassion, scientific understanding, and practical solutions, we can help shift the narrative from shame to empowerment—replacing silence with support and anxiety with resilience.
Further Reading:
Nervous Poops: Here’s Why They Happen


