Many people are familiar with the peculiar discomfort that arises just after a bowel movement. Whether it’s a dull ache, sharp cramp, or bloated unease, the experience can be unsettling, especially when it becomes a recurring issue. For some, the concern begins with a simple observation: “Why does my stomach hurt after I poop?” Others may ask, “Why am I pooping so much and my stomach hurts?” These questions, while seemingly straightforward, reveal a complex interplay between digestive function, neurological signaling, emotional health, and underlying medical conditions such as Irritable Bowel Syndrome (IBS). In this article, we’ll explore the medical, psychological, and functional reasons behind post-defecation discomfort and examine how bloating, diarrhea, nausea, and fatigue might signal a deeper gastrointestinal disturbance.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
Understanding the Gut-Brain Connection in Digestive Pain
The gastrointestinal tract is intricately linked with the brain via the gut-brain axis, a bidirectional communication system involving the enteric nervous system and central nervous system. This system helps regulate motility, secretion, immune responses, and even mood. When we ask, “Why does your stomach hurt when you have to poop?” we’re not merely describing a local physical reaction; we are observing a neurologically modulated phenomenon. For individuals with IBS, this relationship is often dysregulated, leading to heightened pain perception known as visceral hypersensitivity. This means that what might be a normal movement in the intestines for one person becomes painful for another.
Painful bowel movements, particularly those followed by lower abdominal discomfort, may also be related to muscle contractions that continue even after defecation is complete. These contractions can produce sensations similar to menstrual cramps or a sharp pain in the lower abdomen after pooping. It’s not uncommon for patients to describe abdominal cramps after defecating that seem disproportionate to the act itself. Understanding this neurogastroenterological complexity helps frame digestive pain not as an isolated issue but as a symptom of broader dysregulation.
IBS, Diarrhea, and Cramping: Unraveling the Symptom Cluster
Among the most common culprits behind post-poop discomfort is Irritable Bowel Syndrome, particularly its diarrhea-predominant subtype (IBS-D). Individuals often report bloating and diarrhea occurring together, followed by sharp or aching pain once a bowel movement has finished. This lingering discomfort can stem from intestinal inflammation, though IBS is not considered an inflammatory condition in the traditional sense. Instead, it represents a functional gastrointestinal disorder, where structure appears normal but function is impaired.
In cases of IBS-D, stool consistency is often loose, and individuals may experience a sense of incomplete evacuation. This can contribute to repeated trips to the bathroom and questions like, “Why am I pooping so much and my stomach hurts?” Lower stomach pain and mushy poop frequently appear together, which may further intensify feelings of frustration and physical fatigue. For some, symptoms escalate during or after meals, suggesting a dysregulated gastrocolic reflex. Cramping when you poop is often associated with the colon’s response to food and stress, which can exacerbate already sensitive tissues. When the belly hurts after pooping, it might reflect this exaggerated motility pattern combined with heightened visceral awareness.
The Role of Bloating, Gas, and Loose Stools
Gas and bloating are natural byproducts of digestion, but excessive gas production or impaired absorption can lead to significant discomfort. Many individuals experience what causes lots of gas and loose stools without understanding the biochemical dynamics behind them. Excess fermentation of undigested carbohydrates in the colon by gut bacteria can result in bloating and diarrhea, particularly in those with carbohydrate malabsorption issues like lactose intolerance or fructose malabsorption. These conditions may overlap with IBS, making diagnosis and treatment challenging.
A bloated, distended abdomen followed by a sudden urge to defecate is a hallmark experience for many living with irritable bowel syndrome and nausea. This can lead to confusion about whether nausea is caused by the digestive system itself or by an underlying motility issue. In either case, when the stomach hurts after pooping, it may be due to intestinal spasms continuing even after elimination. The discomfort after bowel movement might feel like sharp, transient cramps or dull, lasting aches depending on the individual’s sensitivity and the type of bowel activity preceding it.
Nausea and Vomiting in the Context of IBS
While less commonly discussed, nausea is a frequently reported symptom in IBS, especially in patients with overlapping upper gastrointestinal symptoms. This raises important clinical questions such as: Can IBS cause nausea? And does IBS cause nausea in a way that mimics gastritis or other upper GI conditions? Research suggests that in many cases, the answer is yes. The dysregulation in gut-brain signaling that characterizes IBS does not stop at the colon—it can affect the entire digestive tract.
Nausea associated with IBS is often episodic and occurs in tandem with changes in bowel habits. In more severe cases, individuals may also report IBS vomiting during acute flare-ups, often accompanied by dizziness or anxiety. For those who experience stomach cramps before a bowel movement, the subsequent pain and discomfort can trigger a stress response that makes nausea worse. When asking, “Can IBS cause vomiting?” it’s important to differentiate between functional vomiting due to gut hypersensitivity and vomiting related to other gastrointestinal diseases like gastroparesis or ulcers.
Fatigue, Mental Health, and Digestive Pain
Digestive discomfort is rarely isolated to the gut. It can reverberate across the body, contributing to fatigue, emotional exhaustion, and even mood disturbances. Many patients with IBS ask, “Can IBS cause fatigue?” And increasingly, research supports that it can. The physical act of digestion, especially when complicated by pain and urgency, demands significant energy. Chronic activation of the body’s stress response—common during periods of heightened abdominal pain when defecating—can lead to systemic fatigue.
Moreover, mental health plays a pivotal role in the experience of gastrointestinal symptoms. Anxiety and depression are both more prevalent among those with functional gut disorders, and these conditions can intensify the perception of pain. When patients notice that their GI symptoms keep getting worse, they may be experiencing a feedback loop in which stress exacerbates symptoms, and worsening symptoms intensify stress. In this context, even a mild cramp when pooping can become an emotionally charged and physically draining event.
Recurring Discomfort After Defecation: Seeking Patterns
Patterns are key to understanding chronic digestive complaints. If someone frequently asks, “Why does my stomach hurt before I poop?” or “Why does my stomach hurt when I need to poop?” they may be experiencing anticipatory gastrointestinal pain, which often occurs in IBS. The gut becomes hypersensitive to distension, and the brain becomes hyper-aware of upcoming digestive activity. This leads to symptoms that occur even before the bowel has moved, including bloating, nausea, and anxiety.
In these situations, it’s not uncommon to experience abdominal pain when defecating that doesn’t entirely resolve post-elimination. This lingering discomfort after bowel movement might feel like internal bruising or a pulling sensation in the lower abdomen. For some, this is accompanied by sharp pain in the lower abdomen after pooping that lasts several minutes to hours. The cyclical nature of these symptoms may result in individuals fearing meals, skipping social engagements, or avoiding public bathrooms, all of which can contribute to worsening physical and emotional symptoms.
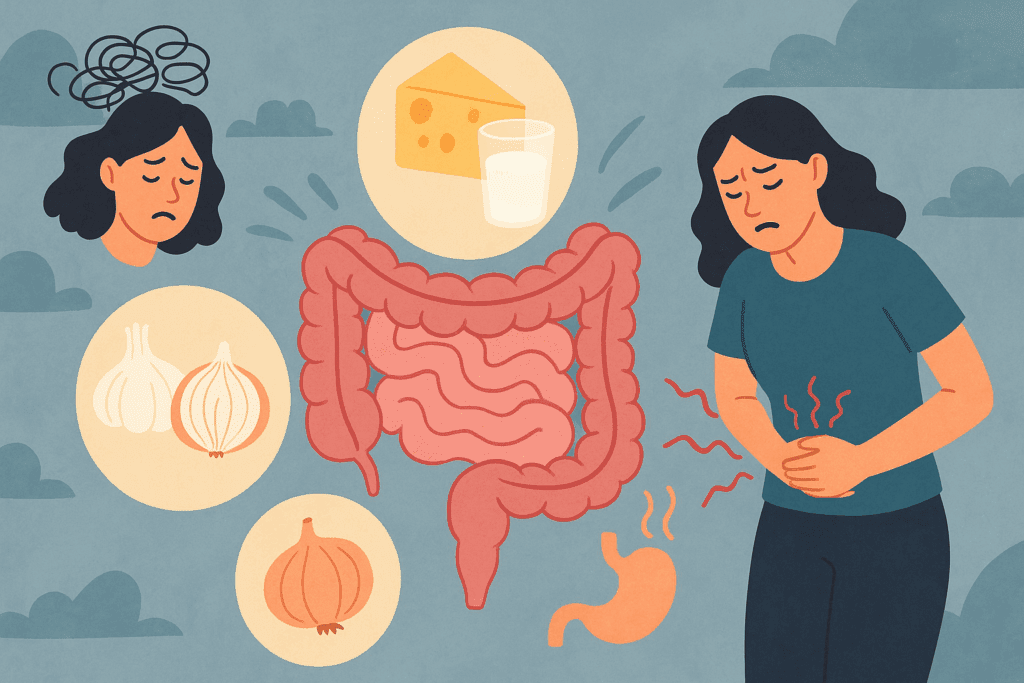
Triggers and Flare-Ups: What Makes IBS Worse?
Understanding what causes IBS flare-ups is central to managing post-poop discomfort. Flare-ups can be triggered by dietary changes, stress, hormonal fluctuations, or even alterations in routine. High-FODMAP foods—those that are fermentable and poorly absorbed—are often culprits, contributing to what causes lots of gas and loose stools. During these flare-ups, patients frequently report that their belly hurts after pooping more than usual and that their fatigue and nausea have also intensified.
Additionally, gut flora imbalances and post-infectious changes can set the stage for chronic flare patterns. This helps explain why some people report that their GI symptoms keep getting worse even after attempting various treatments. Medications like antibiotics, painkillers, or even antidepressants can alter gut motility and microbial composition, exacerbating symptoms. In these cases, abdominal cramps after defecating might be part of a broader physiological shift that extends beyond digestion.
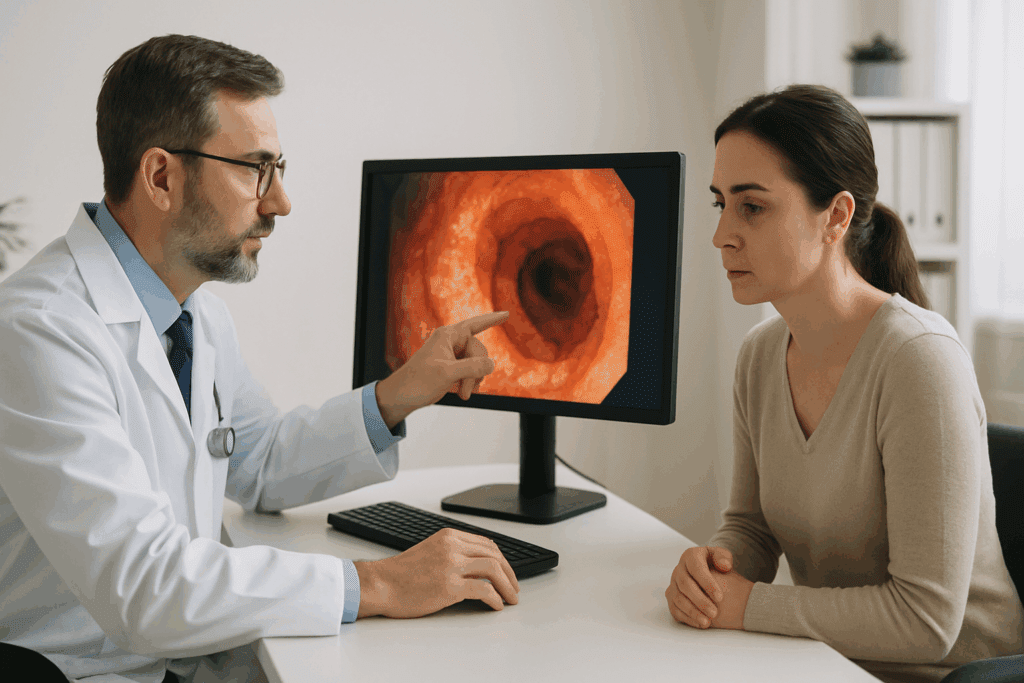
Diagnosing Digestive Pain: Ruling Out Other Causes
Although IBS is a common cause of post-defecation pain, it’s not the only one. It’s crucial to rule out other conditions, particularly when symptoms persist or worsen. Inflammatory Bowel Disease (IBD), including Crohn’s disease and ulcerative colitis, can also present with painful bowel movements and lower abdominal pain. While these conditions involve overt inflammation that can be seen during endoscopy, IBS does not. This distinction is vital when considering treatment.
Other conditions that may mimic IBS include endometriosis, which can cause pelvic and abdominal pain when defecating, and celiac disease, which involves an autoimmune response to gluten. In some cases, structural issues such as rectal prolapse or internal hemorrhoids may contribute to post-poop discomfort. If a patient reports symptoms like cramp when pooping or consistent pain that doesn’t improve with standard IBS management, further evaluation may be warranted to explore these alternatives.
When to Seek Help and What to Expect from Treatment
Recurring digestive pain should never be dismissed, particularly when it affects daily functioning or quality of life. A thorough medical evaluation often begins with a detailed history, stool testing, and possibly imaging studies to rule out organic disease. If IBS is suspected, treatment often involves dietary modifications, stress reduction techniques, and targeted medications such as antispasmodics or low-dose antidepressants that modulate gut-brain signaling.
Behavioral therapies such as gut-directed hypnotherapy or cognitive behavioral therapy can also be helpful, particularly for individuals who experience intense stomach cramps before bowel movements or feel their GI symptoms keep getting worse despite medical treatment. Addressing underlying anxiety and depression may reduce both the frequency and severity of symptoms, including bloating and diarrhea or irritable bowel syndrome and nausea. When pain is severe, options like pelvic floor physical therapy or neuromodulation therapies may also be considered.
Frequently Asked Questions: Post-Bowel Movement Pain, IBS, and Digestive Discomfort
1. Why does my stomach hurt after I poop even when my bowel movements seem normal?
Stomach pain after a seemingly normal bowel movement can stem from hypersensitivity in the gut, particularly among those with functional bowel disorders. While the stool may appear healthy in form, the intestines might still be undergoing subtle spasms or overactive contractions that continue post-defecation. This phenomenon often relates to increased neural reactivity in the gut lining—a characteristic seen in many IBS patients. Even mild or transient abdominal cramps after defecating can reflect nervous system overactivation in the digestive tract. When your stomach hurts after pooping without obvious gastrointestinal changes, it may suggest an underlying sensitivity or neurogastroenterological imbalance rather than a structural issue.
2. What could explain why I’m pooping so much and my stomach hurts afterward?
When you find yourself wondering, “Why am I pooping so much and my stomach hurts?” it’s often due to abnormal gut motility. Excessive or frequent pooping combined with pain may indicate that your intestines are overreacting to food, stress, or internal triggers. Diarrhea-predominant IBS (IBS-D) is a primary cause, but infections, dietary intolerances, and gut flora imbalances can also accelerate transit time and contribute to painful bowel movements. A key sign to watch for is whether this pattern is episodic or chronic; frequent loose stools paired with discomfort after bowel movement can sometimes signal a persistent functional gastrointestinal disorder that needs clinical attention.
3. Can IBS cause nausea and vomiting even if I don’t have diarrhea?
Yes, IBS can cause nausea even in the absence of diarrhea or classic lower GI symptoms. The stomach and upper intestines share many nerve pathways with the colon, and IBS-related hypersensitivity may extend upward. Nausea without vomiting is more common, but during severe IBS flare-ups—especially when bloating and diarrhea are also present—vomiting may occur as a stress or sensory response. It’s important to note that IBS vomiting is typically not persistent or severe enough to cause dehydration, unlike that caused by infections or obstruction. If nausea and vomiting accompany changes in bowel habits or abdominal pain when defecating, a broader evaluation is warranted to rule out overlapping conditions.
4. Why does my lower stomach hurt and my poop look mushy or loose?
Lower stomach pain and mushy poop are frequently linked by fast colonic transit, which limits water absorption and leaves stool soft or unformed. This may happen due to a range of causes including stress, dietary triggers, or inflammatory signals in the gut. People often associate this with irritable bowel syndrome and nausea, especially when these symptoms cluster around emotional distress. It’s not uncommon for people with IBS-D to feel abdominal cramps before bowel movement and then pass loose stool accompanied by pain. Over time, recognizing the foods or stressors that worsen these patterns can help tailor treatment.
5. Why does your stomach hurt when you have to poop, and what does that mean about your gut health?
When your stomach hurts before or during the need to defecate, it usually points to visceral hypersensitivity—a heightened pain response to bowel distention or movement. This is a key trait of IBS, particularly in those who experience poop pains regularly. The gut in these individuals is more reactive, meaning normal peristalsis (intestinal contractions) may feel like sharp pain in the lower abdomen after pooping or just before. This type of discomfort does not necessarily indicate damage but may reflect a nervous system that is too tuned in to the digestive process. Learning to manage gut sensitivity through diet, mindfulness, or medication may reduce the perception of pain.
6. What causes lots of gas and loose stools, and how can I reduce them without medication?
Dietary carbohydrates that ferment in the gut are among the leading causes of excessive gas and loose stools. FODMAPs—found in onions, garlic, dairy, beans, and some fruits—are poorly absorbed and easily fermented, especially in individuals with IBS. This fermentation leads to bloating and diarrhea, often followed by abdominal cramps after defecating. While medications can help, many people benefit from structured elimination diets, probiotic adjustments, and mindful eating habits to lower fermentation rates. When trying to reduce discomfort after bowel movement without drugs, addressing dietary fermentables can be a noninvasive first step.
7. Why do I experience sharp pain in the lower abdomen after pooping even if I feel relief at first?
Sharp post-poop pain that emerges after initial relief may be due to residual spasms in the colon or pelvic floor muscles. Sometimes, the rectum may not fully relax during defecation, leaving behind tension that manifests as abdominal pain when defecating ends. In others, incomplete evacuation can trigger a feedback loop of continued contractions. These cramps when pooping are often misinterpreted as signs of inflammation, but in IBS, they usually indicate functional disruption rather than structural disease. Pelvic floor therapy and biofeedback techniques can help retrain the muscles involved to reduce this pain pattern.
8. What causes IBS flare-ups, and why do they seem to keep getting worse over time?
IBS flare-ups are driven by a combination of triggers including diet, emotional stress, microbiome imbalances, and hormonal changes. What causes IBS flare-ups varies from person to person, but common contributors include sleep disturbances, medication shifts, and even weather changes. Many people feel that their GI symptoms keep getting worse because of cumulative sensitivity—the more flares they experience, the more their gut becomes reactive. Chronic stress in particular lowers the threshold for what the gut considers threatening, leading to discomfort after bowel movement even under minor provocation. Long-term flare-up control often requires a combination of cognitive behavioral therapy, dietary tuning, and sometimes neuromodulators.
9. Can IBS cause fatigue, and what’s the physiological link between the gut and low energy?
Fatigue in IBS patients is multifactorial. First, poor nutrient absorption—especially during episodes of bloating and diarrhea—can lead to reduced energy levels. Second, chronic pain from abdominal cramps after defecating or persistent poop pains drains physical and mental resources. Third, the gut’s continuous activation of the immune and nervous systems may contribute to systemic fatigue, even when bloodwork appears normal. When IBS causes fatigue, it often mimics the tiredness seen in chronic fatigue syndrome or fibromyalgia, both of which frequently co-occur with functional bowel disorders. Addressing sleep hygiene, gut inflammation, and autonomic regulation is essential to rebuilding energy.
10. What practical steps can I take if my belly hurts after pooping and I’m not getting relief from standard IBS treatments?
When standard IBS therapies fail and the belly hurts after pooping continues, it may be time to explore advanced options. First, stool testing can help identify overlooked pathogens or imbalances in gut flora contributing to symptoms like stomach hurts after pooping. Second, brain-gut behavioral therapies, including gut-directed hypnotherapy, can calm the nervous system’s reactivity. Third, if structural issues like rectal prolapse or dyssynergia are suspected, a colorectal specialist may perform targeted diagnostics. Importantly, when asking, “Why does my stomach hurt after a bowel movement?” and getting few answers from conventional care, a multidisciplinary approach—integrating gastroenterology, psychology, and dietetics—often brings the greatest improvements.
Reflecting on Discomfort: What Your Digestive Pain May Be Telling You
Ultimately, asking questions like “Why does your belly hurt when you have to poop?” or “Why does your stomach hurt after a bowel movement?” reflects a need to listen more carefully to your body’s internal signals. Pain, especially recurring digestive pain, is never without context. Whether the discomfort arises from functional hypersensitivity, dietary triggers, or emotional stress, it deserves attention and compassion.
By understanding the nuances of conditions like IBS, recognizing the impact of stress and fatigue, and identifying practical ways to manage symptoms, individuals can begin to take back control of their digestive health. If your stomach hurts after pooping or you regularly experience painful bowel movements, know that you are not alone—and that help is available. The key lies in recognizing the pattern, seeking appropriate care, and remaining proactive in your pursuit of relief.
Further Reading:
Irritable bowel syndrome – Symptoms and causes