Leaky gut syndrome has become one of the most talked-about yet scientifically debated topics in modern digestive and mental health conversations. Its very name stirs up both skepticism and curiosity. Is leaky gut real, or is it a catch-all term used to describe a constellation of symptoms that medicine has yet to fully understand? The answer is complex, shaped by emerging research, anecdotal experience, and the evolving relationship between the gut and overall health. As awareness of gut health grows, especially within integrative and functional medicine, so too does the demand for clear, evidence-based guidance on what leaky gut syndrome actually entails, what causes leaky gut, and how to treat it in a way that is both safe and effective. This article explores the physiological basis of what is commonly called leaky gut, the symptoms of leaky gut syndrome, and the science behind how to fix leaky gut in ways that align with both traditional and complementary medical approaches.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
Understanding the Concept of Leaky Gut
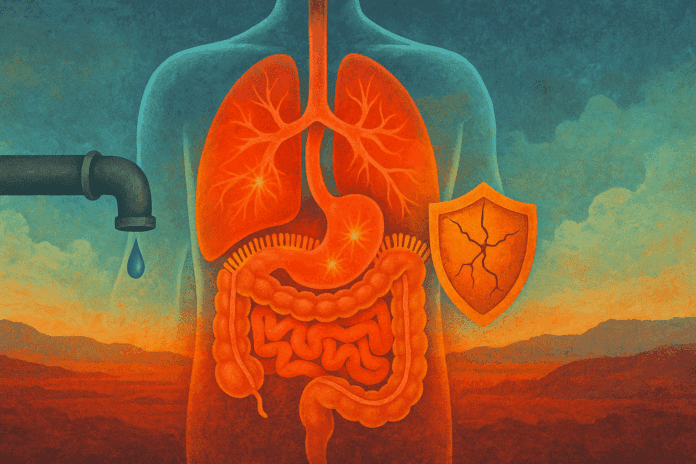
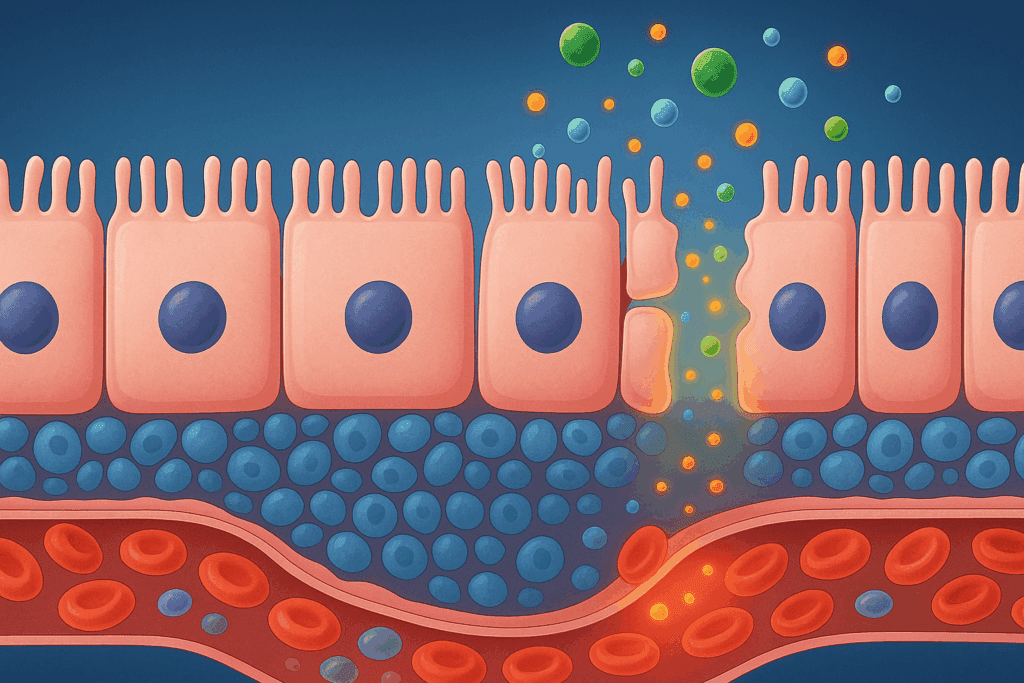
At its core, leaky gut syndrome refers to increased intestinal permeability, a condition in which the lining of the small intestine becomes compromised. Normally, the intestinal barrier functions like a finely tuned sieve, allowing nutrients to pass through while keeping harmful substances—such as toxins, pathogens, and undigested food particles—out of the bloodstream. In the case of a leaking intestine, this barrier becomes porous, allowing these substances to enter systemic circulation and potentially trigger inflammation and immune reactions.
While the concept of a leaky intestine syndrome may sound speculative, it is based on measurable changes in intestinal tight junctions—proteins that seal the spaces between epithelial cells in the gut lining. Disruption of these tight junctions has been observed in conditions like celiac disease, inflammatory bowel disease (IBD), and irritable bowel syndrome (IBS), giving rise to the notion that increased permeability may also underlie a broader array of symptoms even when those disorders are not formally diagnosed. This physiological basis is part of what supports the idea that leaky gut disease, while still controversial, warrants careful clinical consideration.
Recognizing the Symptoms of Leaky Gut Syndrome
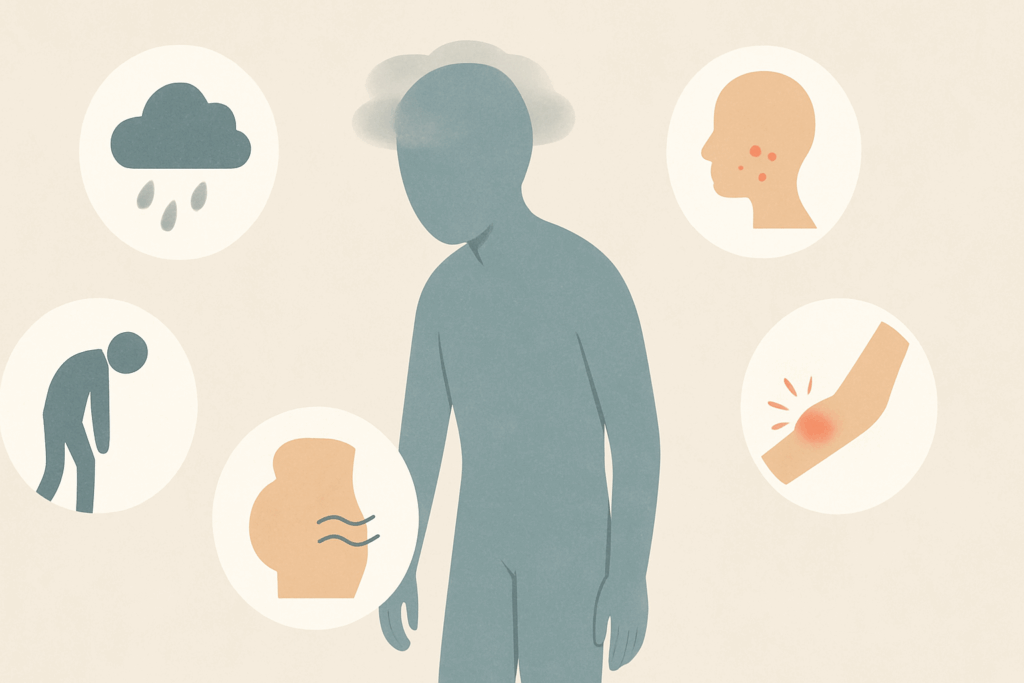
Identifying leaky gut symptoms can be challenging, as they often mimic or overlap with those of other chronic conditions. Some individuals report digestive disturbances such as bloating, gas, diarrhea, or constipation, while others may experience systemic issues including fatigue, joint pain, brain fog, headaches, and skin conditions like eczema or acne. These symptoms of leaky gut syndrome are nonspecific, making diagnosis difficult and sometimes controversial.
However, mounting evidence suggests that symptoms of a leaky stomach or compromised intestinal barrier may contribute to or exacerbate these experiences. For example, some researchers have proposed that a leaky gut disorder may allow pro-inflammatory molecules to reach the brain, influencing mood and cognitive function—a theory that supports the gut-brain axis model. This could help explain why patients with conditions such as depression, anxiety, or even autism spectrum disorders sometimes exhibit signs of gastrointestinal dysfunction alongside neurological symptoms.
Clinical awareness is also growing regarding the indirect signs that may suggest a leaky bowel syndrome, including food sensitivities, unexplained weight fluctuations, autoimmune flare-ups, and persistent fatigue despite adequate rest. While not definitive on their own, these indicators, especially when present alongside known digestive issues, may prompt further investigation into the possibility of a leaky bowel disease or related condition.
What Causes Leaky Gut Syndrome?
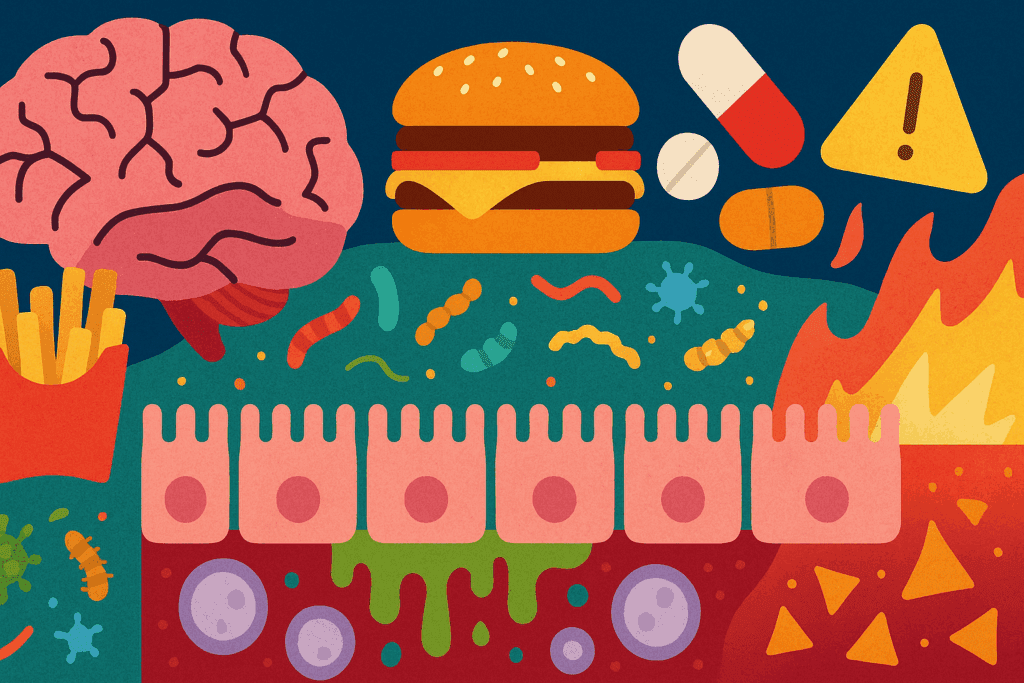
The causes of leaky gut are multifactorial, often involving a combination of genetic, environmental, and lifestyle elements. Chronic stress, poor diet, environmental toxins, and the overuse of certain medications—particularly nonsteroidal anti-inflammatory drugs (NSAIDs) and antibiotics—have all been implicated in the development of intestinal permeability. Emerging research suggests that dysbiosis, or an imbalance in gut microbiota, may also play a significant role in compromising the gut barrier.
For example, diets high in processed foods, refined sugars, and artificial additives can disrupt the delicate microbial ecosystem in the gut, weakening mucosal defenses and contributing to inflammation. Simultaneously, deficiencies in key nutrients such as zinc, vitamin D, and omega-3 fatty acids may impair the body’s ability to repair and maintain the intestinal lining. As such, understanding what causes leaky gut syndrome involves a holistic look at both internal and external stressors that influence gastrointestinal health.
Other potential triggers include chronic infections, alcohol overuse, and hormonal imbalances, each of which may compromise gut integrity through various mechanisms. For individuals predisposed to autoimmune conditions, a leaky gut may serve as a “priming” factor that increases susceptibility to more serious diseases. This theory, while still under investigation, is supported by observational studies noting a correlation between intestinal permeability and autoimmune diseases such as type 1 diabetes, rheumatoid arthritis, and Hashimoto’s thyroiditis.
Is Leaky Gut Syndrome Real?
The debate over whether leaky gut syndrome is real reflects larger tensions between conventional and integrative medicine. Critics argue that leaky gut remains a vague and non-diagnostic label, lacking standardized criteria or universally accepted diagnostic tools. Indeed, the term “leaky gut syndrome” is not recognized as an official medical diagnosis by major health authorities such as the World Health Organization or the American Medical Association.
Nevertheless, the underlying condition of increased intestinal permeability is well-documented in peer-reviewed research. The question is not whether a leaky gut exists in physiological terms, but whether it should be treated as an independent clinical disorder or a secondary phenomenon of other health issues. Integrative practitioners tend to view leaky gut as a central feature of chronic illness, advocating for protocols aimed at restoring gut health to improve systemic symptoms. From this perspective, asking “is leaky gut syndrome real” may miss the more relevant clinical question: how can we best address gut barrier dysfunction when it appears to be contributing to patient distress?
How Is Leaky Gut Diagnosed?
Diagnosing leaky gut remains a challenge in clinical practice, primarily because there is no single, universally endorsed leaky gut syndrome test. However, several research-based tools exist to assess intestinal permeability. The most common is the lactulose-mannitol test, which measures the absorption of two non-metabolized sugars through the intestinal lining. Elevated ratios suggest increased permeability.
Other investigative methods include blood tests for zonulin, a protein that regulates tight junctions and has been found in elevated levels in individuals with celiac disease and other autoimmune disorders. However, the utility of zonulin testing remains debated, as normal reference ranges are not standardized. Stool analyses may also offer indirect insights into gut health by measuring markers of inflammation, microbial diversity, and digestive function. In some cases, clinicians may infer a leaky gut diagnosis based on a patient’s symptoms, history, and response to therapeutic interventions.
Because no single test offers a definitive answer, diagnosing a leaky gut often requires clinical judgment, patient input, and a willingness to treat based on symptom patterns rather than rigid criteria. The lack of a gold standard does not invalidate the patient experience but rather highlights the need for more research into how leaky gut can be diagnosed and treated effectively.

How to Treat Leaky Gut Syndrome: Evidence-Based Approaches
Treating leaky gut involves a multi-pronged strategy aimed at removing irritants, repairing the gut lining, and restoring microbial balance. The first step in how to treat leaky gut syndrome often involves dietary intervention. Many practitioners recommend an elimination diet that removes common allergens and inflammatory foods such as gluten, dairy, processed sugar, and alcohol. This approach helps reduce the immune load on the gut and allows the intestinal lining an opportunity to recover.
In addition to removing triggers, nutritional support is critical. Key supplements often used in leaky gut recovery include L-glutamine, an amino acid that supports intestinal cell repair; zinc carnosine, which promotes mucosal healing; and omega-3 fatty acids, which reduce inflammation. Herbal remedies such as slippery elm, marshmallow root, and licorice extract have also been used to soothe the gut lining, though more robust clinical trials are needed to confirm their efficacy.
Probiotics and prebiotics play an important role in restoring microbial diversity and function. A well-balanced microbiome helps maintain barrier integrity and prevents colonization by pathogenic bacteria. Fermented foods such as sauerkraut, kefir, and kimchi can also support this process naturally. When chosen carefully, targeted supplementation may complement lifestyle interventions and provide a comprehensive approach for those seeking a leaky gut cure.
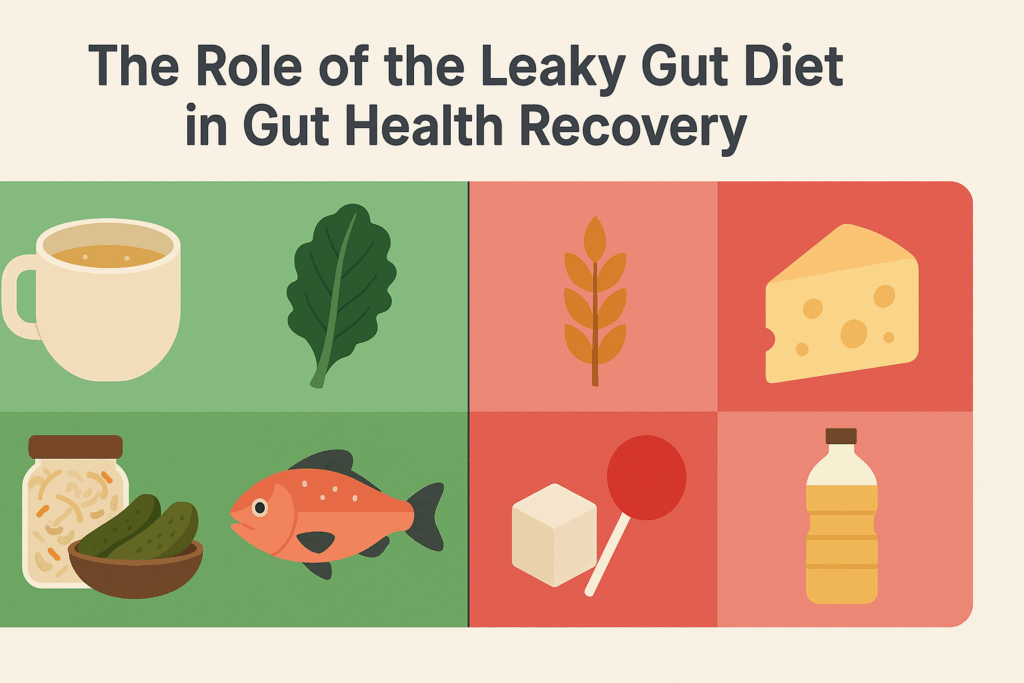
The Role of the Leaky Gut Diet in Gut Health Recovery
A leaky gut diet is often central to any recovery plan, as nutrition directly influences both intestinal permeability and systemic inflammation. While there is no one-size-fits-all leaky gut diet, common elements include whole, unprocessed foods, anti-inflammatory fats, and fiber-rich vegetables. Bone broth is frequently cited as a healing food due to its content of collagen and amino acids like proline and glycine, which may support mucosal repair.
Equally important is the removal of potentially irritating substances. Gluten, dairy, refined carbohydrates, and industrial seed oils are commonly avoided during the initial phases of gut healing. Some protocols also eliminate legumes and nightshades, although evidence for these restrictions remains largely anecdotal. Gradual reintroduction under professional guidance can help identify personal triggers.
Functional medicine practitioners often personalize dietary recommendations based on symptom presentation, lab results, and comorbid conditions. By tailoring a plan that emphasizes nutrient density and minimizes inflammation, patients may experience meaningful symptom relief and begin to understand how to heal leaky gut in a sustainable, non-restrictive way.

Long-Term Leaky Gut Recovery and Maintenance
Healing the gut is not a quick fix. True leaky gut recovery involves sustained effort and often requires lifestyle changes beyond diet alone. Managing stress through mindfulness practices, improving sleep quality, and engaging in regular physical activity are all foundational to long-term gut health. Chronic stress, in particular, has been shown to impair gut barrier function by increasing cortisol and disrupting microbial balance.
Environmental exposures also matter. Reducing contact with pesticides, heavy metals, and endocrine-disrupting chemicals can lessen the toxic burden on the body and support the detoxification systems that work in tandem with gut integrity. Identifying and treating underlying infections or imbalances—whether bacterial, parasitic, or fungal—may be essential for those with persistent symptoms.
Because the gut is a dynamic system, even after initial healing, maintenance is crucial. Periodic reassessment and adjustments to diet, supplementation, and lifestyle can help ensure continued progress. This approach not only addresses how to repair leaky gut but also how to prevent recurrence and maintain optimal health over the long term.
How to Know If You Have Leaky Gut: Awareness and Self-Advocacy
Many people wonder, “how do you know if you have leaky gut?” The answer isn’t always straightforward. Given the wide range of symptoms and lack of standardized diagnostic tools, identifying leaky gut disorder often involves a process of exclusion and pattern recognition. Individuals with unexplained fatigue, brain fog, skin eruptions, and digestive complaints may find that their experiences align with symptoms of a leaky stomach.
Self-advocacy is important in these cases. Keeping a symptom journal, exploring elimination diets, and seeking out healthcare providers who are knowledgeable about gut health can make a significant difference. While not every case of bloating or fatigue points to a leaky gut, persistent or unexplained symptoms deserve attention. Asking the right questions and pursuing appropriate testing—where available—can lead to more personalized care and improved outcomes.
It’s also vital to approach this process with a critical eye. As interest in gut health has grown, so too has the market for unverified supplements and miracle cures. Understanding the difference between marketing hype and scientifically grounded interventions is a key part of the journey toward healing. Ultimately, how you treat leaky gut syndrome depends on both the severity of symptoms and the level of support available.
Frequently Asked Questions: Leaky Gut Syndrome
1. How do you know if you have leaky gut if your symptoms are vague or inconsistent?
Determining whether you have a leaky gut disorder can be challenging, especially since symptoms often overlap with those of other conditions. However, paying attention to patterns—such as recurring food sensitivities, persistent fatigue, skin flare-ups, or mood disturbances—can offer important clues. People frequently report subtle changes like seasonal worsening of symptoms, heightened anxiety after certain meals, or increased brain fog following antibiotic use. While these signs may not confirm a leaky intestine syndrome, they warrant deeper investigation. Keeping a detailed health journal and working with a practitioner trained in gastrointestinal disorders can help determine whether further testing for leaky gut syndrome is appropriate.
2. What is the difference between leaky gut syndrome and other digestive disorders like IBS or celiac disease?
While leaky gut syndrome is associated with increased intestinal permeability, conditions like IBS and celiac disease have defined diagnostic criteria and are generally more widely recognized in mainstream medicine. Leaky gut disorder is often viewed as a functional imbalance, not a formal diagnosis. However, leaky bowel disease may occur alongside these conditions and worsen their progression by allowing inflammatory triggers into the bloodstream. Unlike IBS or celiac, where damage occurs primarily due to specific triggers (like gluten in celiac), leaky gut symptoms stem from a broader compromise of the gut barrier, often caused by diet, medications, or chronic stress. Identifying and treating co-occurring issues can significantly improve outcomes in individuals with suspected leaky gut disease.
3. Are leaky stomach symptoms more common in people with chronic mental health conditions?
Emerging research indicates a link between intestinal permeability and mental health, supporting the gut-brain axis theory. People with depression, anxiety, and ADHD often exhibit increased inflammatory markers and altered gut microbiomes. This suggests that leaky gut symptoms may play a role in perpetuating psychiatric symptoms, particularly when coupled with nutrient malabsorption or food-triggered inflammation. Chronic psychological stress itself is also a factor in what causes leaky gut, as stress hormones like cortisol can degrade gut lining integrity. Treating both the psychological and digestive dimensions may offer a more comprehensive path to wellness for those struggling with both mental and gut health concerns.
4. Can a leaky gut diet help even if you don’t have a confirmed diagnosis?
Yes, adopting a leaky gut diet can benefit individuals even without a formal diagnosis. Anti-inflammatory and whole-food diets help reduce overall immune activation, support microbiome diversity, and encourage tissue healing. Many people with autoimmune conditions or chronic fatigue report improvements when eliminating common gut irritants like gluten, dairy, and processed foods. A diet designed to heal leaky gut does not need to be restrictive forever; rather, it can be a short-term intervention to support leaky gut recovery while identifying individual food triggers. Over time, a more sustainable dietary pattern can be created that supports long-term gut integrity without excessive restriction.
5. How do you treat leaky gut syndrome without relying heavily on supplements?
While supplements like L-glutamine and probiotics are frequently recommended, it is possible to focus on whole-food strategies and lifestyle changes. Key interventions include prioritizing sleep, practicing mindfulness-based stress reduction, and consuming gut-friendly foods like bone broth, fermented vegetables, and high-fiber produce. These approaches support how to repair leaky gut naturally without the need for complex supplement regimens. Furthermore, mindful eating practices—such as chewing thoroughly and avoiding overeating—can also reduce mechanical and inflammatory stress on the gut. These simple, daily habits may be especially helpful for individuals seeking low-cost, sustainable options to support how to heal leaky gut.
6. How to fix leaky gut syndrome when symptoms fluctuate or relapse occurs?
Managing fluctuating symptoms requires a flexible approach. During symptom flare-ups, returning to the foundational principles of a leaky gut diet—removing irritants, reducing stress, and prioritizing rest—can help stabilize gut function. It’s also helpful to revisit your supplement plan and adjust as needed; for example, some people benefit from temporarily increasing probiotic intake or reintroducing anti-inflammatory herbs. Recognizing emotional stressors is just as important, as they can directly affect gut permeability. Long-term, building stress resilience and maintaining consistent eating patterns can make a significant difference in how to fix leaky gut when relapses happen.
7. What causes leaky gut syndrome in otherwise healthy individuals?
Leaky gut disorder isn’t limited to those with chronic illness. Even seemingly healthy individuals may develop increased permeability due to overuse of NSAIDs, high alcohol consumption, or excessive intake of ultra-processed foods. Hidden exposures to pesticides, environmental toxins, or chronic low-grade infections may also contribute to the development of leaky intestine syndrome. Additionally, intense physical training without adequate recovery and nutrition can stress the gut barrier. In such cases, focusing on prevention through conscious lifestyle choices is as important as learning how to treat leaky gut when symptoms do arise.
8. How is leaky gut diagnosed in clinical settings beyond standard testing?
Since no single test offers definitive confirmation, practitioners often rely on functional assessments and clinical intuition. In addition to the lactulose-mannitol test and zonulin markers, some functional medicine providers use intestinal permeability panels that include multiple biomarkers. Stool tests that evaluate secretory IgA levels, calprotectin, or microbial composition can offer indirect insight into the presence of a leaking intestine. Providers may also observe how symptoms respond to a structured elimination-reintroduction diet, using this as a practical tool to assess whether a leaky stomach is contributing to systemic issues. Ultimately, diagnosis is often a synthesis of test results, patient history, and therapeutic response.
9. Is leaky gut syndrome real or just a buzzword in the wellness industry?
While the term “leaky gut syndrome” has gained traction in wellness circles, it reflects a legitimate area of scientific inquiry. The condition known as increased intestinal permeability is well-documented in medical literature, particularly in autoimmune and gastrointestinal disorders. The question “is leaky gut real?” hinges more on how the term is used and understood. Overuse by non-clinicians has fueled skepticism, but it does not invalidate the physiological phenomenon itself. Ongoing research continues to explore how intestinal permeability contributes to chronic disease, with new insights likely to refine both diagnosis and treatment of leaky gut disease in the future.
10. How do you heal leaky gut syndrome while managing other chronic health conditions?
Healing leaky gut syndrome while managing coexisting health challenges—such as thyroid disease, rheumatoid arthritis, or diabetes—requires a personalized and integrative approach. It’s important to coordinate care with practitioners who understand both conventional and functional paradigms. For example, certain medications may aggravate gut permeability, so alternatives should be discussed. The inflammatory burden from leaky bowel syndrome may also compound systemic inflammation, worsening the primary condition. Addressing leaky gut symptoms through targeted diet, stress reduction, and gut support may reduce overall symptom load and improve quality of life, especially when layered into an already complex medical regimen.
Conclusion: Navigating Leaky Gut Syndrome with Science, Strategy, and Support
Understanding what is leaky gut requires more than a cursory glance at wellness trends or dietary fads. It demands a nuanced exploration of physiology, an appreciation for individual variability, and a commitment to evidence-based practice. While the debate over whether leaky gut syndrome is real continues, the lived experiences of patients and the growing body of research on intestinal permeability suggest that this condition cannot be dismissed outright. Whether one refers to it as leaky bowel syndrome, leaky gut disease, or leaky intestine syndrome, the central message is clear: gut health matters, and it affects more than just digestion.
Learning how to fix leaky gut or how to heal leaky gut involves much more than a temporary change in diet. It calls for a thoughtful, layered strategy that includes dietary refinement, lifestyle optimization, targeted supplementation, and medical insight. Recognizing the symptoms of leaky gut syndrome and understanding what causes leaky gut opens the door to more informed decisions and more compassionate care. And while no single leaky gut cure exists, the path to recovery is one that can be walked with clarity, science, and support.
In the end, the question is not merely how to repair leaky gut, but how to maintain a relationship with our bodies that honors complexity, seeks balance, and values well-being. Through careful listening—both to scientific data and personal experience—we can build a better future for digestive and mental health, one gut at a time.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out
Further Reading:
Leaky gut syndrome: What it is, symptoms, and treatments
Leaky Gut Syndrome: Symptoms, Diet, Tests & Treatment
Leaky gut: What is it, and what does it mean for you?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.