Cognitive Behavioral Therapy (CBT) has long been recognized as one of the most effective and widely researched forms of psychotherapy, especially for conditions such as depression, anxiety, trauma-related disorders, and obsessive-compulsive behavior. It combines the practical application of cognitive and behavioral techniques to bring about meaningful psychological change. Central to CBT’s success is its structured, stage-based approach that allows both therapists and clients to track progress, identify challenges, and set specific therapeutic goals. But understanding how CBT unfolds from the initial evaluation to long-term maintenance is essential for anyone considering this therapy or working within the field of mental health.
You may also like: How Does CBT Work to Improve Relationships and Communication? Science-Backed Techniques for Getting Along with Others
The process of CBT is not arbitrary. Rather, it is grounded in an empirically validated framework that begins with a comprehensive cognitive behavioural assessment and moves through distinct yet fluid stages, each aimed at progressively fostering insight, behavioral change, and emotional resilience. This article explores those stages in depth, examining not only what each entails but also how they interconnect to support sustainable mental health outcomes. We will also address a common question among new clients and students of psychology alike: What are the 5 steps of CBT, and how do they contribute to the therapy’s enduring effectiveness?
Laying the Groundwork: The Importance of Cognitive Behavioural Assessment
Every successful therapeutic journey begins with a thorough understanding of the client’s inner world and external circumstances. The cognitive behavioural assessment is the foundational stage of CBT, and it serves as far more than a simple intake process. During this stage, therapists gather detailed information about the client’s presenting concerns, medical and psychological history, thought patterns, emotional triggers, and behavioral responses. This assessment allows for the development of a personalized conceptualization of the client’s struggles, rooted in the core principles of CBT.
What sets cognitive behavioural assessment apart from general intake evaluations in other therapeutic modalities is its emphasis on identifying the interaction between cognition, emotion, and behavior. For example, a client presenting with social anxiety may reveal through this assessment that their avoidance of public settings is driven by distorted beliefs about how others perceive them. These distorted beliefs are not treated as static personality traits but as modifiable cognitive errors that contribute to maladaptive behaviors.
Another vital aspect of this stage is establishing therapeutic rapport and setting initial expectations. Clients often arrive at therapy feeling overwhelmed, ashamed, or uncertain. The assessment phase provides a structured yet empathetic environment to begin normalizing their experiences and instilling hope. Additionally, therapists begin identifying potential obstacles to engagement, such as motivational challenges or external stressors, and develop early strategies to address them.
By the end of this assessment, a detailed treatment plan emerges. This plan includes targeted goals, prioritized areas of intervention, and a hypothesis about the cognitive and behavioral mechanisms maintaining the client’s difficulties. It sets the stage for what is to come—a methodical and evidence-based pathway through the stages of CBT that offers not only symptom relief but also the acquisition of lifelong coping strategies.
Psychoeducation and Goal Setting: Building Awareness and Direction
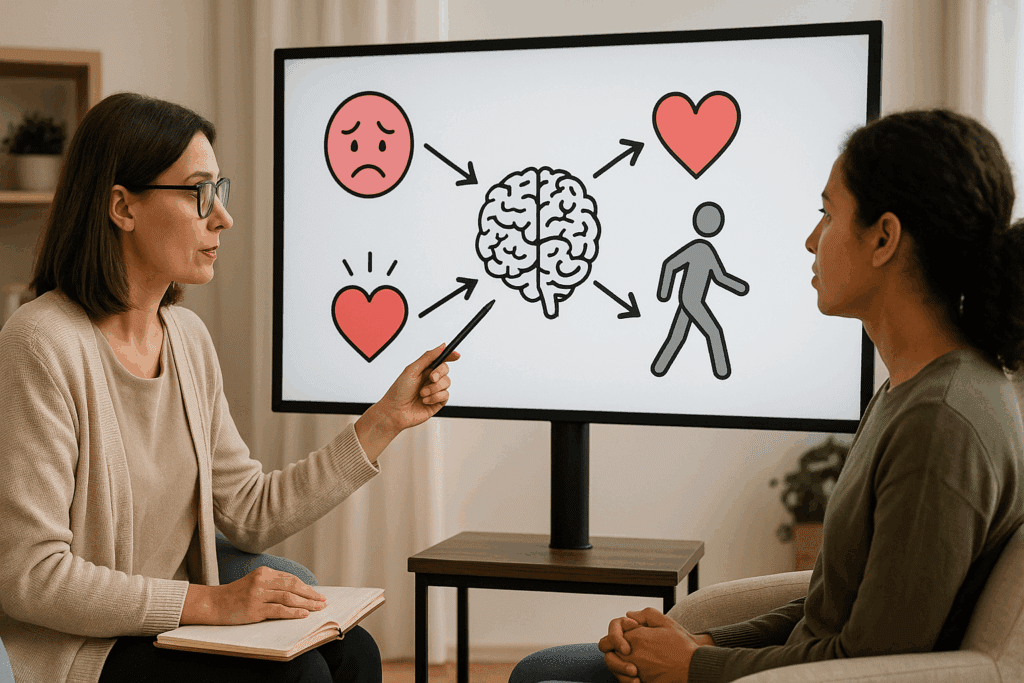
Following assessment, the next crucial stage in CBT involves psychoeducation and goal setting. While some might view psychoeducation as merely informational, in the context of CBT it is an empowering tool that facilitates insight, engagement, and long-term adherence. Clients are introduced to the core CBT model—the interrelationship between thoughts, feelings, and behaviors—and begin to understand how this model applies to their own lives.
In this phase, therapists explain the rationale behind CBT interventions and clarify what clients can expect from the process. Clients are often surprised to discover how significantly automatic thoughts can shape emotional and behavioral reactions. A woman experiencing panic attacks, for instance, might learn that her intense fear is not only physiological but also driven by catastrophic interpretations of bodily sensations. With this new understanding, clients start to become more observant and curious about their internal experiences rather than fearful or avoidant.
Goal setting is another cornerstone of this stage. Goals in CBT are not vague aspirations like “feel better” or “be happy,” but specific, measurable, and time-bound objectives. Effective CBT treatment goals might include reducing the frequency of panic attacks, increasing participation in social activities, or improving sleep hygiene. These goals provide structure and allow both therapist and client to evaluate progress objectively.
Importantly, goal setting in CBT is a collaborative process. Clients are encouraged to articulate their values and priorities, ensuring that the therapy remains aligned with what matters most to them. Therapists guide the refinement of these goals into actionable targets, often using tools like behavioral activation schedules or thought records to monitor outcomes. Through this mutual effort, the therapeutic alliance is strengthened, and motivation is enhanced.
Understanding what are the 5 steps of CBT often begins in this goal-setting phase, where clients become acquainted with the structured, stepwise approach that defines the therapy. These five steps typically include: identifying troubling situations, becoming aware of automatic thoughts, recognizing cognitive distortions, challenging those distortions, and replacing them with more balanced thinking. This cycle becomes the engine that drives the subsequent stages of change.
Cognitive Restructuring: Identifying and Challenging Distorted Thinking
One of the most transformative stages of CBT is cognitive restructuring, which involves the systematic identification and correction of distorted thinking patterns. Clients are taught to become mindful of their automatic thoughts—those quick, reflexive interpretations of events that often go unexamined but powerfully influence mood and behavior. These thoughts are typically rooted in cognitive distortions such as catastrophizing, black-and-white thinking, personalization, or overgeneralization.
The goal here is not to impose positive thinking but to cultivate more accurate and balanced perspectives. For example, a client who constantly thinks, “I always mess things up,” is encouraged to examine the evidence for and against this belief. Through Socratic questioning, behavioral experiments, and guided discovery, clients learn to test their assumptions and develop alternative interpretations that are both realistic and constructive.
This process is deeply empowering. As clients learn to challenge maladaptive thought patterns, they often report feeling a sense of control and agency that had previously felt inaccessible. Their emotional responses begin to shift accordingly. Instead of spiraling into despair after receiving critical feedback, a client may come to see it as an opportunity for growth or a reflection of high standards rather than a condemnation of their worth.
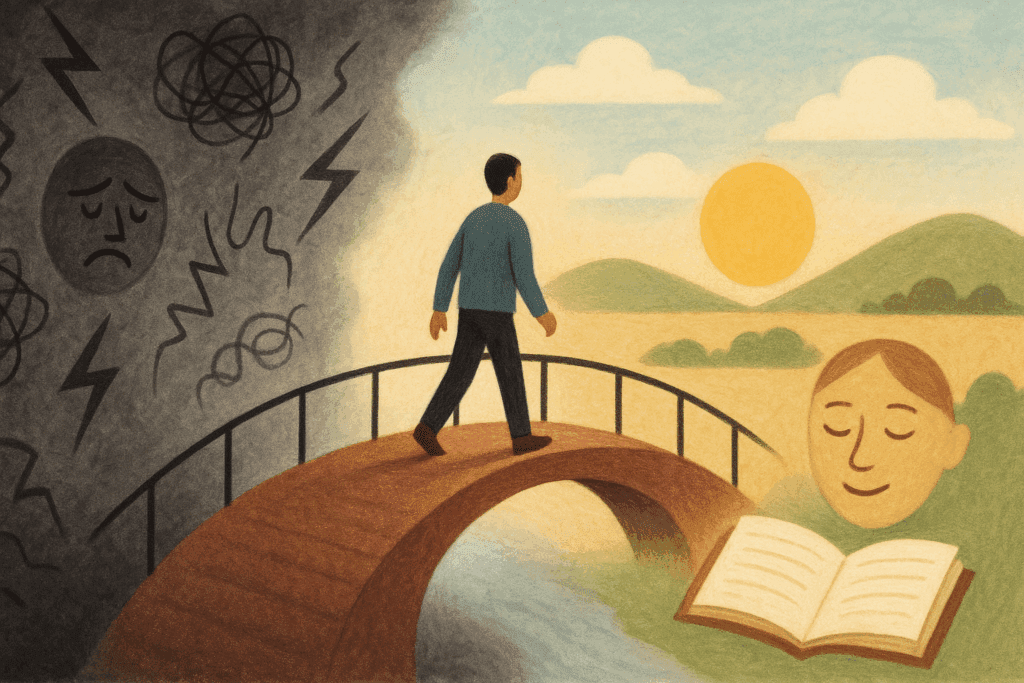
Cognitive restructuring also lays the groundwork for behavioral change by reducing the emotional obstacles that interfere with action. When clients are no longer paralyzed by fear of failure or rejection, they are more willing to experiment with new behaviors. This stage thus serves as a vital bridge between insight and action, making it one of the most dynamic elements in the stages of CBT.

Behavioral Activation and Skill Building: Taking Action Toward Change
The transition from insight to action occurs most tangibly in the behavioral activation phase of CBT. This stage involves systematically reintroducing clients to activities that align with their values, interests, and life goals, particularly those they have been avoiding due to depression, anxiety, or other emotional difficulties. Behavioral activation is not about keeping busy for its own sake; it is about reestablishing patterns of engagement that counteract negative emotional states and promote psychological well-being.
For example, a client with major depressive disorder may have withdrawn from hobbies, social connections, and exercise routines. The therapist helps the client identify and schedule specific activities that can gradually restore a sense of accomplishment and pleasure. These might include walking the dog every morning, attending a weekly art class, or calling a friend once a week. Each of these actions serves as a building block in the recovery process.
In addition to behavioral activation, this stage often includes direct skills training. Clients may learn stress management techniques, problem-solving strategies, assertiveness skills, or mindfulness practices, depending on their individualized needs. These practical tools enhance resilience and provide alternatives to maladaptive coping mechanisms such as avoidance, rumination, or substance use.
This is also a point at which the framework of what are the 5 steps of CBT becomes deeply experiential. Clients begin to see how identifying problems, examining thoughts, and adjusting behaviors in real-time can lead to observable improvements in mood and functioning. The therapy becomes not just a theoretical model but a lived experience that clients internalize and apply independently.
Relapse Prevention and Maintenance: Sustaining Progress Over Time
As therapy nears completion, the focus shifts toward consolidating gains and preparing clients to maintain their progress long after sessions have ended. This stage is often referred to as relapse prevention and maintenance, but it is far more proactive than the term “relapse prevention” might suggest. Rather than simply avoiding setbacks, clients are taught to anticipate challenges and respond to them with confidence and flexibility.
During this phase, clients revisit the cognitive and behavioral strategies they have learned and explore how these can be adapted to new or unexpected situations. Therapists encourage the development of a personalized toolkit, often in the form of written plans or digital reminders, that can be drawn upon during periods of stress or emotional vulnerability. This might include a list of supportive contacts, go-to relaxation techniques, or affirmations grounded in previous therapeutic insights.
Clients are also guided through exercises that simulate future difficulties. For instance, a client who has overcome panic disorder might be asked to role-play an anxiety-inducing scenario or journal about how they would handle a recurrence of symptoms. These exercises are designed to reinforce the belief that setbacks are manageable and that old patterns need not dictate future outcomes.
Importantly, this final stage reinforces the autonomy and competence that CBT aims to cultivate. Clients are reminded that while therapy has provided a structure, the real work of transformation lies in their ongoing choices and actions. The emphasis is on living deliberately, not reactively.
In this phase, the question of what are the 5 steps of CBT becomes a personalized framework that clients can refer to whenever new challenges arise. Similarly, reflecting on the stages of CBT helps clients appreciate how far they have come—from the initial cognitive behavioural assessment through the development of insight, skill, and resilience.
Integrating the Stages: A Lifelong Framework for Mental Well-Being
While each stage of CBT has its own distinct focus, they are not isolated compartments but interconnected phases of a comprehensive therapeutic journey. The progression from cognitive behavioural assessment to maintenance is not linear in a rigid sense; rather, it is responsive to the client’s evolving needs and circumstances. For some, revisiting earlier stages may be necessary when new issues emerge. Others may continue using tools from all stages in a fluid, ongoing manner.
This integrative view reinforces the idea that CBT is not merely a treatment but a skill set—one that clients carry forward into their lives as a means of navigating complexity, building emotional resilience, and fostering meaningful change. The stages of CBT are not only a roadmap for healing but also a framework for thriving, grounded in decades of empirical research and clinical wisdom.
Understanding what are the 5 steps of CBT within this broader context allows clients and clinicians alike to appreciate their practical value. When individuals learn to identify problematic situations, examine their thoughts, challenge distortions, test alternatives, and implement balanced perspectives, they gain a repeatable strategy for managing emotional challenges across diverse settings and life transitions.
Ultimately, the power of CBT lies in its ability to adapt and endure. The core principles remain consistent, but their application evolves as the client evolves. From the very first cognitive behavioural assessment to the final moments of relapse prevention, CBT offers a dynamic, empowering, and enduring pathway to emotional wellness.
Frequently Asked Questions (FAQ) on the Stages of CBT, Cognitive Behavioural Assessment, and the Five Steps of CBT
1. How does the cognitive behavioural assessment influence the rest of CBT treatment?
The cognitive behavioural assessment doesn’t just inform the therapist’s understanding of the client’s current difficulties—it actively shapes the direction and tone of the entire therapeutic process. This phase is where individualized patterns of thought, emotion, and behavior are mapped out in context, helping clinicians tailor interventions based on a nuanced understanding of the client’s lived experience. Unlike traditional diagnostic evaluations, cognitive behavioural assessment prioritizes functional analysis over labels, which makes the treatment more precise and actionable. It also allows for the early identification of subtle cognitive distortions that may not be immediately visible but significantly influence symptoms. As a result, this assessment stage serves as a dynamic blueprint that therapists revisit and refine throughout the various stages of CBT.
2. Can the stages of CBT be adapted for clients with neurodiverse conditions like ADHD or autism?
Yes, the stages of CBT can and should be adapted to meet the cognitive and emotional needs of neurodiverse individuals. While the structured nature of CBT offers clarity, therapists often need to adjust the pacing, language, and delivery methods to enhance engagement and comprehension. For instance, visual aids or metaphor-based reframing might be more effective for autistic clients, while clients with ADHD may benefit from shorter sessions and increased emphasis on behavioral activation. The initial cognitive behavioural assessment is crucial here, as it helps the therapist identify executive functioning challenges, sensory sensitivities, and processing styles. By tailoring the stages of CBT in this way, therapists can maintain therapeutic fidelity while honoring neurodiverse strengths and needs.
3. What are the 5 steps of CBT and how do they apply in crisis situations?
The five steps of CBT include identifying the situation, recognizing automatic thoughts, examining cognitive distortions, challenging unhelpful beliefs, and developing balanced alternatives. In crisis scenarios, this framework serves as an emotional triage tool. Clients can quickly map their reactions using these steps to gain momentary stability, especially when experiencing panic, anger, or emotional flooding. Therapists might teach clients to use a brief version of the five-step method—for example, through a thought log app or a crisis card with prewritten reframes. What makes these steps especially helpful in emergencies is their grounding effect, bringing the client’s focus from reactive emotional states back to structured problem-solving. This application reinforces the flexibility and durability of CBT even under high-pressure conditions.
4. How do the stages of CBT account for cultural or identity-related issues in therapy?
Culturally responsive CBT incorporates identity-informed approaches at every stage, beginning with the cognitive behavioural assessment. Therapists are trained to ask questions that explore how cultural, religious, gender, and socioeconomic identities intersect with thought patterns and behavior. For example, automatic thoughts related to intergenerational expectations or discrimination may emerge that are deeply influenced by cultural values. During the later stages of CBT, particularly cognitive restructuring, therapists help clients challenge these thoughts within the context of cultural validation rather than assuming a universal standard. Adapting the stages of CBT to honor cultural nuance not only fosters inclusivity but also improves treatment adherence and emotional resonance.
5. Are there limitations to the five steps of CBT when dealing with complex trauma?
While the five steps of CBT are powerful tools, they can sometimes oversimplify the emotional landscape of individuals with complex trauma. These clients may experience fragmented memory, dissociation, or deeply embedded belief systems that are not easily accessible through surface-level cognitive interventions. In such cases, the cognitive behavioural assessment must be extended to include trauma-specific metrics and narrative-based techniques. Furthermore, therapists often integrate stabilization work before engaging in full cognitive restructuring, blending elements of DBT or somatic therapies to ensure safety. Nonetheless, the foundational logic of the five steps of CBT remains applicable—it just requires a more flexible and trauma-sensitive implementation.
6. How do clients transition between the stages of CBT, and is it always linear?
Contrary to common assumptions, the stages of CBT do not unfold in a strictly linear fashion. While there is a general sequence from assessment to intervention to maintenance, therapy often circles back to earlier stages in response to new developments or insights. For instance, a client may revisit the cognitive behavioural assessment after experiencing a major life event that reactivates dormant thought patterns. Similarly, cognitive restructuring might resurface later in therapy if new distortions emerge under stress. This fluid movement between stages reflects CBT’s adaptability and responsiveness to the client’s evolving psychological landscape. A skilled therapist will normalize these transitions and use them as growth opportunities.
7. What role does the cognitive behavioural assessment play in identifying comorbid conditions?
A comprehensive cognitive behavioural assessment can illuminate overlapping symptoms that point toward comorbidities, such as anxiety and depression co-occurring with substance use or eating disorders. Because this assessment focuses on functional relationships between thoughts, behaviors, and emotions, it often uncovers patterns that diagnostic checklists alone may miss. For example, a client with OCD may reveal perfectionistic thinking that also drives disordered eating. Recognizing these interwoven dynamics early allows the therapist to structure the stages of CBT accordingly, perhaps alternating between symptom-specific interventions and broader cognitive strategies. This holistic approach enhances accuracy and improves long-term outcomes by addressing root causes rather than isolated symptoms.
8. How do the five steps of CBT integrate with mindfulness-based approaches?
Mindfulness techniques can enrich the five steps of CBT by enhancing present-moment awareness and cognitive flexibility. Before clients even begin identifying automatic thoughts, mindfulness can help them observe their internal states without judgment, making the process of thought recognition more precise. During the step of challenging distorted beliefs, mindfulness encourages acceptance and compassion rather than adversarial thinking, which can soften resistance. Many therapists now integrate mindfulness practices such as breathwork or body scans as preparatory tools within the stages of CBT. This fusion is especially helpful for clients with ruminative tendencies, as it promotes a balanced approach to both cognitive intervention and emotional regulation.
9. Can digital tools support progress across the stages of CBT?
Yes, technology has introduced a range of digital tools that enhance the effectiveness of CBT across all stages. During the cognitive behavioural assessment, digital intake forms with mood tracking or interactive surveys can offer deeper insights. In later stages, mobile apps that guide clients through the five steps of CBT can facilitate real-time practice and reflection outside therapy sessions. Platforms like MoodNotes or CBT Thought Record offer structured templates for identifying and challenging negative thoughts. Additionally, AI-based mental health platforms are emerging to help deliver personalized feedback, making CBT more accessible between appointments. While these tools should never replace the human therapist, they can significantly augment engagement and accountability.
10. What long-term changes can clients expect after completing all stages of CBT?
Clients who fully engage with the stages of CBT often report long-lasting changes that extend beyond symptom reduction. They develop meta-cognitive skills—the ability to think about their thinking—which leads to improved decision-making, emotional resilience, and interpersonal functioning. Even years after treatment ends, many clients continue to use elements of the five steps of CBT in daily life, especially when facing new stressors. The insights from the initial cognitive behavioural assessment also tend to remain relevant, acting as a self-awareness anchor during future challenges. Ultimately, CBT equips clients not just with therapeutic tools, but with a philosophy of psychological flexibility and proactive mental health care that endures well beyond the therapy room.
Conclusion: From Cognitive Behavioural Assessment to Empowered Living
As we have explored, the stages of CBT represent more than just a structured sequence of therapy sessions; they embody a philosophy of change rooted in self-awareness, evidence-based strategies, and personal agency. From the initial cognitive behavioural assessment, which uncovers the underlying patterns driving emotional distress, to the empowering skills of cognitive restructuring and behavioral activation, CBT equips individuals with the tools they need to transform their lives.
By understanding what are the 5 steps of CBT and how they function within this broader framework, both clients and clinicians can approach therapy with clarity, intention, and confidence. These steps are not simply theoretical constructs—they are practical, actionable tools that support long-term recovery and emotional resilience. They help bridge the gap between insight and action, between awareness and lasting change.
Moreover, the emphasis on maintenance and relapse prevention underscores CBT’s commitment to sustainable mental health. The conclusion of therapy does not signify the end of growth but rather the beginning of self-directed mastery. Clients leave CBT not only with symptom relief but with a lifelong framework for understanding and navigating the complexities of thought, emotion, and behavior.
In a world increasingly focused on quick fixes and surface-level solutions, the depth and durability of CBT offer a refreshing and hopeful alternative. Whether you are a prospective client, a mental health professional, or a curious reader, understanding the stages of CBT can provide a valuable lens through which to view emotional well-being, personal development, and psychological healing. Through assessment, insight, action, and reflection, CBT empowers individuals to reclaim their lives—one thought, one behavior, and one moment at a time.


