In the intricate architecture of the human brain, where trillions of neural connections orchestrate memory, language, decision-making, and personality, the concept of neurocognitive health is foundational. When these cognitive faculties begin to decline in ways that are inconsistent with normal aging, it may point to a condition known as a neurocognitive disorder. These disorders, marked by progressive or sudden impairments in mental function, are more than just a medical diagnosis—they are a deeply personal and often life-altering experience for those affected and their loved ones.
As our population ages and neurological research advances, public awareness of neurocognitive disorder has expanded. Yet for many, the term remains abstract, obscured by vague definitions and confusion with other mental health conditions. A clear understanding of the types of cognitive disorders, their underlying causes, and the early warning signs can empower individuals and families to seek timely and appropriate care. This article explores these critical issues, offering both a scientific and humanistic perspective on one of the most pressing challenges in contemporary mental health and wellness.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Defining Neurocognitive Disorder: Beyond Simple Forgetfulness
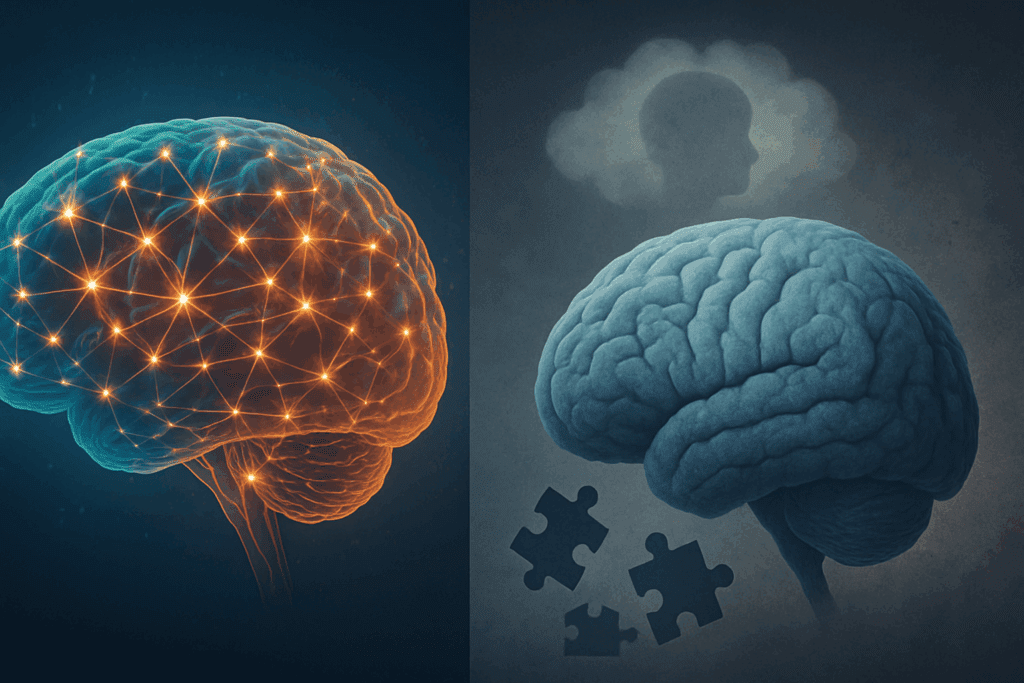
Neurocognitive disorder (NCD) is a clinical term used to describe a range of conditions characterized by a significant decline in one or more cognitive domains, such as memory, language, attention, reasoning, perception, or executive functioning. Unlike temporary lapses in focus or the mild forgetfulness that comes with aging, NCD involves persistent impairments that interfere with a person’s daily functioning and autonomy. It encompasses both mild and major forms, with major neurocognitive disorder often equated with dementia in clinical settings.
Importantly, neurocognitive disorder is not a disease itself but rather a category of disorders with diverse etiologies. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), classifies NCDs based on the presumed underlying pathology—whether neurodegenerative, vascular, traumatic, or due to other medical conditions. This classification system reflects the medical community’s shift toward a more nuanced understanding that considers both symptoms and causative mechanisms.
Many individuals are surprised to learn that neurocognitive disorder can arise at any age, though it is more prevalent in older adults. It may progress gradually, as seen in Alzheimer’s disease, or develop abruptly, as in the case of a traumatic brain injury. Regardless of onset, the impact on personal identity and daily life can be profound, underscoring the importance of early recognition and accurate diagnosis.
The Spectrum of Neurocognitive Impairment: Exploring Types of Cognitive Disorders
Understanding the different types of cognitive disorders is essential for accurate diagnosis, effective treatment planning, and compassionate caregiving. Each disorder within the neurocognitive spectrum has distinct features, although overlap often occurs.
One of the most common and widely recognized types of cognitive disorders is Alzheimer’s disease. This neurodegenerative condition is characterized by the gradual accumulation of amyloid plaques and tau tangles in the brain, leading to progressive memory loss, language difficulties, disorientation, and changes in behavior. It represents a major neurocognitive disorder and accounts for approximately 60 to 80 percent of dementia cases.
Another significant subtype is vascular neurocognitive disorder, which results from reduced blood flow to the brain due to stroke, atherosclerosis, or other cardiovascular conditions. Unlike the steady decline seen in Alzheimer’s, vascular NCD may present in a stepwise fashion, with periods of stability interrupted by sudden cognitive deterioration. Symptoms often include impaired judgment, slowed thinking, and difficulties with attention rather than memory alone.
Lewy body dementia, another neurodegenerative form, is marked by visual hallucinations, fluctuating cognition, and movement symptoms similar to Parkinson’s disease. Meanwhile, frontotemporal neurocognitive disorder tends to affect individuals at a younger age and involves early personality changes, emotional instability, and deficits in language or social cognition.
Beyond these major forms, mild neurocognitive disorder represents an intermediate stage in which cognitive impairments are noticeable but not severe enough to significantly hinder daily independence. This stage is often a precursor to more serious decline and provides a critical window for intervention.
Other types of cognitive disorders include those caused by infections (such as HIV-related NCD), substance use, traumatic brain injuries, or rare genetic conditions. As the understanding of neurobiology grows, researchers are increasingly identifying overlapping mechanisms and shared risk factors among these seemingly distinct conditions.
Root Causes and Contributing Factors: Why Neurocognitive Disorders Develop
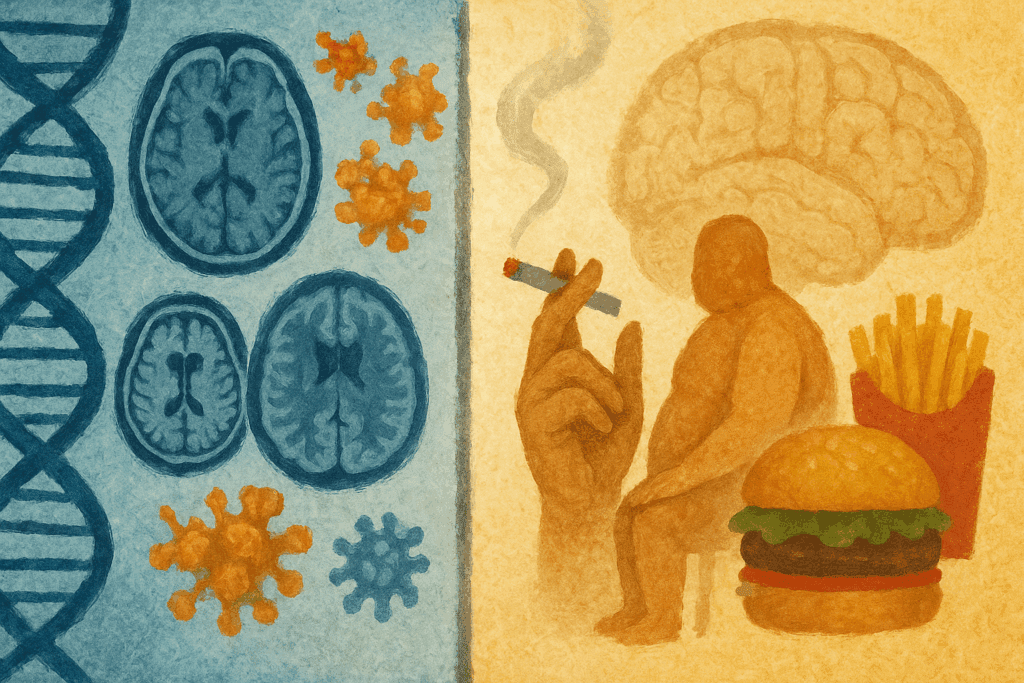
The origins of neurocognitive disorder are as varied as the human brain itself, shaped by a complex interplay of genetics, lifestyle, environment, and underlying health conditions. While age remains the most significant risk factor, it is by no means the only determinant.
In the case of Alzheimer’s disease, genetic mutations in genes such as APP, PSEN1, and PSEN2 can cause early-onset forms, though these are rare. More commonly, variants in the APOE gene, particularly APOE4, increase the likelihood of developing late-onset Alzheimer’s, though they do not guarantee it. Environmental factors—such as exposure to toxins, head trauma, and cardiovascular disease—can also heighten risk by damaging brain structures or impeding neurovascular health.
Vascular neurocognitive disorder, in contrast, is more directly linked to modifiable factors like hypertension, diabetes, smoking, high cholesterol, and obesity. These conditions compromise blood flow and promote the formation of small clots or infarcts that disrupt brain function. Controlling these risk factors through lifestyle and medical management can significantly reduce the likelihood of cognitive impairment.
Neurocognitive disorders associated with Lewy bodies or frontotemporal lobar degeneration often arise from abnormal protein accumulation, though the exact triggers remain under investigation. Infections, autoimmune conditions, and chronic inflammation may also contribute to the pathological cascade that disrupts neural connectivity and neurotransmitter balance.
Mental health conditions such as depression, anxiety, and post-traumatic stress disorder (PTSD) can further complicate the clinical picture. While these do not constitute neurocognitive disorders themselves, they can mimic or exacerbate symptoms, leading to diagnostic uncertainty. Substance misuse, particularly of alcohol, benzodiazepines, or illicit drugs, can also produce cognitive deficits that persist even after withdrawal, especially if neurotoxicity or nutritional deficiencies are involved.
Given this wide range of contributing factors, the assessment of a suspected neurocognitive disorder must be thorough and multidimensional. Brain imaging, neuropsychological testing, blood work, and detailed medical history are often necessary to identify the underlying cause and determine the best course of action.
Recognizing Early Signs: When Cognitive Changes May Indicate a Problem
It is often difficult to distinguish between benign age-related changes and the early manifestations of a neurocognitive disorder. Forgetting names or misplacing items may be normal from time to time, especially under stress. However, when memory lapses become frequent, interfere with work or social life, or are accompanied by other cognitive or behavioral changes, it may be time to consider a deeper evaluation.
Among the most common early warning signs is difficulty remembering recently learned information, especially if reminders or cues do not help. Individuals may repeatedly ask the same questions, struggle to follow conversations, or lose track of dates and locations. These memory deficits often coexist with trouble planning or organizing tasks, leading to frustration and a decline in confidence.
In other cases, changes in language may be more prominent. This could include difficulty finding the right words, substituting inappropriate terms, or abandoning conversations midway due to confusion. Impaired judgment and decision-making, especially in financial or safety-related matters, can be early indicators of more significant decline.
Personality changes are also common, particularly in frontotemporal disorders. A previously sociable person may become apathetic, impulsive, or uncharacteristically inappropriate. Loved ones may notice increased irritability, withdrawal, or resistance to change, all of which can signal cognitive and emotional dysregulation.
Importantly, these symptoms should not be viewed in isolation. The pattern, progression, and impact on daily function provide essential context. A neurocognitive disorder is more than a single symptom—it is a syndrome that unfolds over time and affects multiple domains of life.
Seeking Help: When and How to Begin the Diagnostic Journey
Deciding when to seek medical evaluation for cognitive concerns can be daunting. Many individuals fear the implications of a diagnosis or worry about being dismissed as simply aging. Yet early assessment is crucial—not only for identifying the presence and type of cognitive disorder but also for ruling out reversible causes and initiating appropriate support.
Primary care providers are often the first point of contact and can conduct preliminary screenings, such as the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA). These tools provide a snapshot of cognitive function and help determine whether further evaluation by a neurologist, psychiatrist, or neuropsychologist is warranted.
In cases where a neurocognitive disorder is suspected, a comprehensive evaluation may include brain imaging (MRI, CT, or PET scans), laboratory tests to exclude metabolic or infectious causes, and formal neuropsychological testing. These assessments are essential for differentiating between the types of cognitive disorders and determining the underlying pathology.
Equally important is the involvement of family members or close caregivers in the diagnostic process. Their observations can provide valuable insights into functional changes, daily challenges, and personality shifts that the individual may be unaware of or reluctant to report.
Timely diagnosis allows for the implementation of interventions that may slow progression, enhance quality of life, or address coexisting conditions. It also gives individuals and families the opportunity to plan for the future, access resources, and make informed decisions about care and support.
Living with a Neurocognitive Disorder: Strategies for Maintaining Dignity and Function
A diagnosis of neurocognitive disorder can feel overwhelming, but it does not signify the end of a meaningful life. Many individuals continue to lead fulfilling, productive lives with proper management, community support, and adaptive strategies. Understanding the specific type of cognitive disorder involved enables tailored interventions that respect the person’s strengths, preferences, and values.
Cognitive rehabilitation therapies, for example, can help maintain or improve certain functions through structured exercises and compensatory techniques. These programs may target memory, attention, or problem-solving and are often delivered by occupational therapists or neuropsychologists in clinical settings.
Environmental modifications also play a crucial role. Simplifying routines, using visual cues, and creating structured daily schedules can reduce confusion and promote independence. Technologies such as medication reminders, GPS tracking, and voice-assisted devices are increasingly used to support autonomy and safety.
Emotional and social support remain foundational. Many people with neurocognitive disorder experience depression, anxiety, or isolation, especially in the early stages. Regular engagement with family, friends, support groups, or faith communities can enhance emotional resilience and provide a sense of belonging.
Caregiver education and respite are equally essential. Caring for someone with cognitive impairment is rewarding but often emotionally and physically taxing. Providing caregivers with resources, counseling, and practical guidance improves not only patient outcomes but also caregiver well-being and longevity.
Future Horizons: Advances in Research and Hope for Prevention
Scientific understanding of neurocognitive disorders continues to evolve at an unprecedented pace. Researchers are exploring new biomarkers, imaging techniques, and genetic risk profiles that may one day enable earlier and more accurate diagnosis—even before symptoms emerge.
Pharmacological research is also making strides, particularly in Alzheimer’s disease. While current medications such as donepezil, memantine, and rivastigmine offer symptomatic relief, newer agents targeting amyloid and tau pathology hold promise for disease modification. However, these treatments require careful consideration of risks, costs, and eligibility, and they are not curative.
Non-pharmacological interventions remain a vibrant area of inquiry. Studies increasingly support the role of lifestyle factors in delaying or mitigating the risk of neurocognitive disorders. Physical activity, cognitive stimulation, social engagement, and adherence to diets such as the Mediterranean or DASH diet have all shown neuroprotective potential. These findings reinforce the concept of brain health as a lifelong endeavor—one influenced by daily choices and cumulative habits.
Preventive strategies are gaining traction among public health professionals. Initiatives aimed at cardiovascular health, educational attainment, and early childhood development may have long-term cognitive benefits. Likewise, reducing exposure to environmental toxins and addressing health disparities may help narrow the risk gap among vulnerable populations.
Frequently Asked Questions (FAQ): Understanding Neurocognitive Disorder and Cognitive Health
1. How can lifestyle changes influence the progression of a neurocognitive disorder?
Emerging research suggests that lifestyle interventions can significantly impact the trajectory of a neurocognitive disorder, especially in its early stages. While these changes cannot reverse established brain damage, they may help slow progression and preserve function for a longer period. Regular aerobic exercise has been linked to increased hippocampal volume, a brain region critical for memory, and may counteract the brain shrinkage seen in many types of cognitive disorders. Nutritional choices, such as adherence to the MIND or Mediterranean diet, have also shown promise in reducing neuroinflammation and supporting vascular health. Sleep hygiene, social engagement, and cognitive stimulation complete the trifecta of lifestyle strategies recommended by neurologists and geriatricians alike.
2. Are certain occupations more prone to developing a neurocognitive disorder later in life?
While the exact relationship between occupation and neurocognitive disorder risk is complex, evidence suggests that cognitively demanding careers may offer a protective buffer. Professions involving strategic thinking, problem-solving, and social interaction—such as teaching, law, and engineering—appear to build cognitive reserve. This concept refers to the brain’s ability to improvise and find alternate ways of completing tasks despite damage. Conversely, some industrial or combat-related occupations involving repeated head trauma or exposure to neurotoxins may increase the risk for certain types of cognitive disorders. The balance between mental stimulation and environmental safety plays a pivotal role in long-term cognitive resilience.
3. How do neurocognitive disorders differ in rural versus urban populations?
Access to diagnostic resources, specialist care, and rehabilitative services often shapes the trajectory of neurocognitive disorders in different populations. Individuals in rural areas may face delays in diagnosis due to limited availability of neurologists or neuropsychological testing, leading to later-stage presentation and reduced treatment options. Additionally, health literacy and cultural perceptions of aging can influence when—and if—families seek help. In contrast, urban populations typically have better access to multidisciplinary care teams but may contend with greater stress, social isolation, or pollution, which can also impact brain health. These disparities highlight the importance of public health initiatives tailored to community-specific needs.
4. What is the role of inflammation in the development of neurocognitive disorders?
Chronic inflammation is increasingly recognized as a contributor to various types of cognitive disorders, including Alzheimer’s and vascular dementia. Systemic inflammation can disrupt the blood-brain barrier, allowing immune molecules and pathogens to infiltrate sensitive neural tissues. Over time, this leads to oxidative stress, neuronal loss, and impaired synaptic function—hallmarks of neurocognitive disorder pathology. Conditions such as diabetes, obesity, and autoimmune diseases elevate inflammatory markers and may increase susceptibility. Anti-inflammatory strategies, including the use of omega-3 fatty acids, dietary antioxidants, and exercise, are currently under investigation for their neuroprotective potential.
5. Can technology play a role in managing neurocognitive disorders?
Technology has become an indispensable ally in the management of neurocognitive disorders, both for individuals and caregivers. Apps that offer cognitive training, medication reminders, and behavioral tracking are now part of standard supportive care. For those with mobility or geographic limitations, telehealth provides access to neurologists, mental health professionals, and support networks that would otherwise be unavailable. Wearable devices can track sleep, physical activity, and even detect wandering in patients with advanced types of cognitive disorders. These innovations not only improve quality of life but also offer critical data to clinicians aiming for personalized care.
6. How does a neurocognitive disorder affect emotional intelligence and empathy?
While cognitive impairments often dominate the clinical picture, changes in emotional processing are also common in neurocognitive disorders. Individuals may lose the ability to recognize facial expressions or respond appropriately to social cues, particularly in frontotemporal dementia. These deficits in empathy can strain relationships, sometimes leading loved ones to mistake symptoms for intentional rudeness or coldness. Emotional blunting may also make it difficult for individuals to express distress, creating communication challenges in clinical settings. Understanding the emotional dimensions of these conditions is key to developing compassionate care strategies that preserve dignity.
7. Are there gender differences in the prevalence or progression of neurocognitive disorders?
Gender differences are notable in the epidemiology of neurocognitive disorders. Women are disproportionately affected by Alzheimer’s disease, even when accounting for their longer life expectancy. Some studies suggest that hormonal shifts during menopause may influence brain metabolism, contributing to the higher prevalence of certain types of cognitive disorders among women. Men, on the other hand, are more frequently diagnosed with frontotemporal dementia and often present with more pronounced behavioral changes. These differences underscore the importance of gender-specific research in understanding risk, progression, and response to therapy.
8. Can early-life experiences shape the risk of developing a neurocognitive disorder?
Yes, a growing body of evidence suggests that cognitive health in later life is deeply influenced by early-life factors. Adverse childhood experiences, limited access to education, and early malnutrition are associated with increased risk for several types of cognitive disorders. These factors may limit the development of cognitive reserve and expose the brain to prolonged stress, inflammation, or deprivation. Conversely, lifelong learning, bilingualism, and intellectually rich environments appear to bolster resilience against neurodegeneration. The life-course approach to brain health is becoming a central theme in prevention-oriented research.
9. What are some emerging therapies on the horizon for treating neurocognitive disorders?
Several cutting-edge therapies are currently under investigation to address both symptoms and root causes of neurocognitive disorders. Monoclonal antibodies targeting beta-amyloid and tau proteins have shown mixed but promising results in early Alzheimer’s trials. Gene therapies, though still experimental, aim to correct underlying mutations associated with inherited types of cognitive disorders. Researchers are also exploring neuromodulation techniques, such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS), for their potential to restore neural connectivity. Advances in regenerative medicine, including stem cell therapies, may one day offer avenues for neural repair.
10. When should caregivers consider transitioning someone with a neurocognitive disorder into assisted living or memory care?
Determining the right time to transition a loved one into professional care is one of the most emotionally complex decisions for caregivers. The decision should be guided by safety, quality of life, and the caregiver’s own well-being. Signs that may indicate the need for memory care include frequent wandering, falls, incontinence, or inability to manage basic hygiene or nutrition independently. As types of cognitive disorders progress, individuals may also exhibit behaviors such as aggression or paranoia that become unmanageable at home. Engaging in open dialogue with healthcare providers and considering respite care options can help families make informed and compassionate choices.
Conclusion: Embracing Holistic Awareness and Innovation in the Era of Neurocognitive Disorders
As scientific understanding deepens and social awareness expands, it is crucial to approach neurocognitive disorder not merely as a medical condition but as a complex life journey that intersects with identity, relationships, and long-term care decisions. While we have made remarkable strides in identifying the many types of cognitive disorders and their risk factors, our work is far from finished. Advances in personalized medicine, neurotechnology, and preventive strategies continue to reshape the possibilities for diagnosis, treatment, and daily management. Equally important is our collective responsibility to nurture a culture of empathy, informed caregiving, and equitable access to support services. By embracing innovation alongside compassion, we open the door to a future where individuals affected by neurocognitive disorders can thrive with dignity, resilience, and hope.
Further Reading:
Major Neurocognitive Disorder (Dementia)
Understanding neurocognitive disorders: Types, causes, symptoms and treatment