Understanding the Difference Between Normal Forgetfulness and Concerning Memory Loss
Forgetfulness is a natural part of aging. Nearly everyone occasionally misplaces their keys or forgets someone’s name. However, differentiating between benign lapses in memory and early indicators of more serious cognitive decline is a crucial task—one that can be both medically and emotionally complex. While it’s common for people to experience mild forgetfulness due to stress, fatigue, or age-related changes, persistent memory issues that interfere with daily life should never be ignored. This is especially true when such issues disrupt routines, impair communication, or begin to impact safety and personal independence.
The signs that warrant concern often go beyond simple forgetfulness. Repeatedly asking the same questions, forgetting familiar routes, struggling to follow conversations, or showing poor judgment are examples that may indicate something more serious. These are red flags that suggest a need to see a doctor for memory loss, as they could point to underlying neurological conditions such as Alzheimer’s disease, vascular dementia, or other forms of cognitive impairment. The earlier these warning signs are recognized, the sooner effective interventions can be considered, which is why early evaluation is so important.
Moreover, there’s an important distinction between memory loss due to a reversible cause—such as a medication side effect, vitamin deficiency, or thyroid problem—and that stemming from progressive neurodegenerative conditions. Identifying the root cause requires clinical expertise, which reinforces the value of consulting a doctor for memory issues. What may appear as routine forgetfulness could, in fact, be a symptom of a treatable condition, but without a comprehensive medical assessment, these opportunities for intervention can be missed. Early detection and an accurate diagnosis not only support better health outcomes but also offer patients and their families a clearer understanding of what to expect moving forward.
You may also like: What to Eat to Boost Memory: Science-Backed Brain Foods That Improve Recall, Focus, and Long-Term Mental Health
What to Expect During a Medical Evaluation for Memory Concerns
Visiting a healthcare provider for memory evaluation is a proactive step, not a sign of alarm. When people decide to see a doctor for memory loss, the process typically begins with a detailed conversation about symptoms, their onset, and how they are affecting daily life. This history-taking stage is essential, as it helps the physician understand the context of the memory problems and distinguish between benign memory lapses and those linked to more serious conditions. The more detailed and specific the information provided, the more accurate the assessment.
In most cases, the evaluation will include cognitive screening tests such as the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA). These standardized tools help clinicians gauge memory, language, attention, and executive function. However, they are only one part of the picture. Depending on the initial findings, the physician may order blood tests to check for underlying medical issues like vitamin B12 deficiency or hypothyroidism, both of which can contribute to memory problems but are reversible with proper treatment. Imaging studies such as MRI or CT scans may also be used to look for structural abnormalities in the brain, such as tumors, strokes, or signs of neurodegeneration.
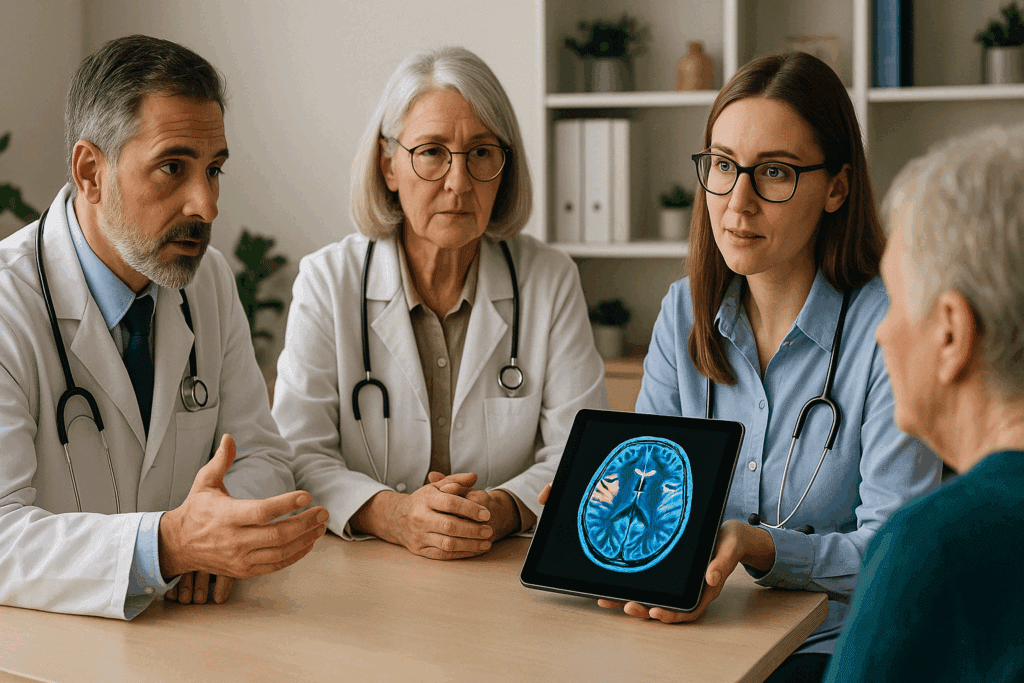
A key aspect of these evaluations is the collaborative, multidisciplinary approach often involved. Neurologists, geriatricians, psychologists, and sometimes even psychiatrists may all contribute to forming a comprehensive understanding of the patient’s cognitive health. The presence of mood disorders like depression and anxiety, which can mimic or exacerbate memory loss, is also assessed. By the end of this evaluation process, patients should have a clearer picture of whether their memory issues are normal, reversible, or indicative of a more serious condition. The entire experience underscores the benefit of seeing a doctor for memory issues rather than attempting to self-diagnose or delay care.
The Importance of Early Detection and Diagnosis
When it comes to cognitive decline, timing is everything. Early diagnosis not only opens the door to more treatment options but also allows patients and families to plan for the future with greater clarity and control. In the early stages of many neurodegenerative diseases, including Alzheimer’s, interventions can slow progression and improve quality of life. Medications like cholinesterase inhibitors and memantine are most effective when used in the earlier phases of dementia, before significant brain damage has occurred. This is another compelling reason to consult a doctor for memory loss at the first signs of trouble.
In addition to pharmacologic treatments, early detection enables engagement in non-drug interventions that have been shown to preserve function and independence. Cognitive stimulation therapies, memory training exercises, physical activity, and dietary modifications can all contribute to better outcomes. However, for these strategies to be effective, the condition must be identified early. Waiting until symptoms are advanced often limits the potential for meaningful improvement, both medically and functionally.
Families also benefit greatly from early diagnosis. It allows them to become educated about the nature of the illness, make necessary legal and financial arrangements, and ensure that the person with memory issues is involved in their own care planning while they are still capable of making informed decisions. These preparations become far more difficult once cognitive decline is severe. Seeing a doctor for memory issues before they escalate is a step toward empowerment—not just for the individual but for their entire support system. Understanding the prognosis, managing expectations, and accessing support resources all begin with a timely and accurate diagnosis.
Reversible Causes of Memory Loss: Why Early Evaluation Matters
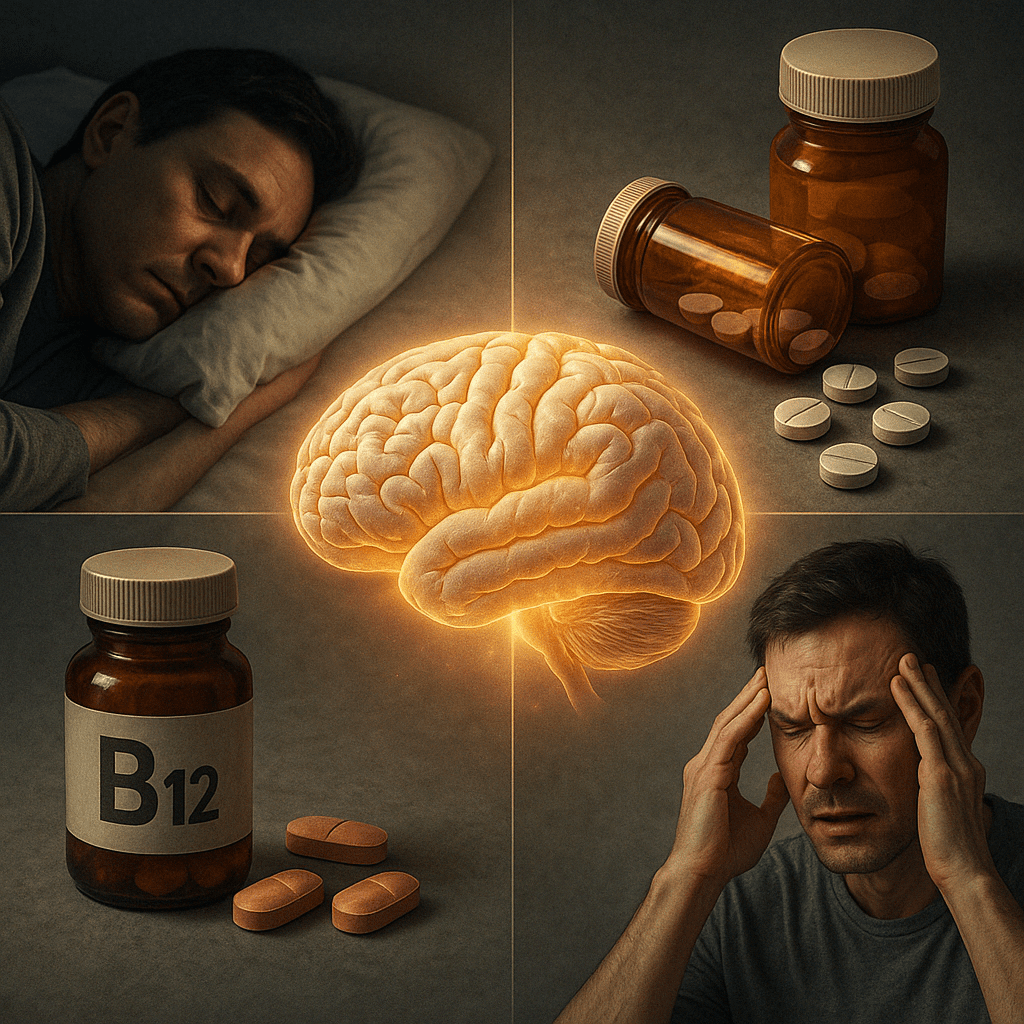
While many people associate memory loss with irreversible conditions like dementia, it’s important to recognize that some causes are completely treatable. Identifying and addressing these underlying factors can lead to full or significant recovery of cognitive function. Common reversible causes include medication side effects, especially from sedatives, antihistamines, and certain painkillers, which may impair memory and concentration. Discontinuing or adjusting these medications under medical supervision can often restore mental clarity.
Nutritional deficiencies, particularly of vitamin B12, folate, and thiamine, can also contribute to cognitive symptoms. These nutrients play a vital role in brain function, and their deficiency can lead to confusion, forgetfulness, and even mood changes. Supplementation can reverse these effects when the deficiency is caught early, highlighting the need to see a doctor for memory loss rather than making assumptions or resorting to over-the-counter solutions. Hormonal imbalances, such as those caused by hypothyroidism, are another example. Because the thyroid regulates metabolism, low hormone levels can result in sluggish thinking, depression, and memory difficulties—all of which are reversible with the right treatment.
Another commonly overlooked factor is sleep. Chronic sleep deprivation or sleep disorders like sleep apnea can severely impair memory consolidation. Individuals may not even be aware that their sleep quality is compromised, yet their cognitive function suffers. Similarly, emotional factors like untreated depression and anxiety can masquerade as memory impairment. These conditions affect attention and processing speed, making it harder for the brain to encode and retrieve information. Treating the root psychological condition often resolves the cognitive symptoms as well.
In each of these cases, seeing a doctor for memory issues allows for the kind of comprehensive evaluation that can uncover and treat these reversible causes. When addressed early, these interventions can restore function and greatly improve quality of life, making medical evaluation not just beneficial but essential.
How Specialists Help Diagnose and Manage Memory Disorders
Primary care physicians are often the first point of contact for people experiencing memory problems, but in many cases, referrals to specialists are necessary for a definitive diagnosis and long-term management plan. Neurologists, for instance, specialize in diseases of the nervous system and are equipped to diagnose complex conditions like Alzheimer’s disease, Lewy body dementia, or frontotemporal dementia. Their expertise is invaluable in interpreting imaging studies, administering advanced cognitive tests, and ruling out less common causes of memory decline.
Geriatricians also play a pivotal role, especially for older adults. They consider age-specific factors that may influence cognitive health and are adept at managing multiple comorbidities, medications, and functional issues that affect memory. Their holistic approach ensures that all potential contributors to cognitive impairment are considered, including social and environmental factors. Neuropsychologists add another layer of insight by conducting in-depth evaluations that go far beyond standard screening tools. Their assessments measure specific areas of cognitive functioning and help distinguish between different types of dementia, which can influence treatment strategies.
For individuals with mood disorders or psychiatric symptoms that overlap with cognitive decline, psychiatrists may be consulted. They can evaluate whether memory issues are primarily related to a mental health condition or are indicative of an emerging neurological disorder. This multidisciplinary collaboration is one of the strongest arguments for seeking professional care. Attempting to navigate memory loss without the guidance of trained specialists can result in misdiagnosis, delayed treatment, and unnecessary anxiety.
Ultimately, the goal of seeing a doctor for memory loss is not just to name a condition but to gain a nuanced understanding of what is happening in the brain and how best to respond. A specialist-guided plan often includes both medical treatments and supportive strategies, such as cognitive rehabilitation, caregiver support, and legal or financial counseling. This comprehensive approach provides not only clinical direction but also a pathway for individuals and families to move forward with clarity, confidence, and compassion.
What Loved Ones Should Know: Recognizing Memory Issues and Offering Support
Families and close friends often notice memory changes long before the individual experiencing them does. This can place loved ones in a challenging position, caught between concern and uncertainty about whether to speak up or wait for more obvious signs. The truth is, being proactive and compassionate can make all the difference. If you’re a family member who has observed troubling signs—such as a parent who forgets important appointments, misplaces items in unusual places, or seems confused in familiar environments—it’s crucial not to dismiss these signs as mere “senior moments.” While aging does bring some natural cognitive slowing, distinct shifts in memory, communication, or behavior should prompt a conversation, ideally one grounded in empathy and support rather than fear or accusation.
Encouraging a loved one to see a doctor for memory loss may feel daunting, especially if the individual is in denial or fears being labeled. But reframing the conversation around wellness and prevention can help. For example, suggesting a memory checkup as part of a broader health evaluation—like an annual physical—can reduce the stigma and resistance. It’s often helpful to emphasize that seeing a doctor for memory issues doesn’t automatically lead to a diagnosis of dementia. Instead, it provides an opportunity to better understand the cause and explore interventions early, when they can have the most impact.
Caregivers also need to be prepared for the emotional toll of watching someone they love struggle with memory issues. Frustration, grief, and guilt are common, especially when a once-independent person becomes increasingly reliant on others. Knowing that early intervention improves outcomes can help caregivers feel more empowered and less helpless. In addition to medical treatment, caregivers can benefit from support groups, respite care options, and mental health counseling to manage their own well-being. Navigating memory decline is not just a medical journey—it’s a deeply human one, and loved ones play a pivotal role in supporting those affected.
When and How to Talk to a Doctor About Memory Concerns
Initiating a conversation about memory issues—whether it’s for yourself or someone you care about—can feel intimidating. For many people, fears of embarrassment, stigma, or what a diagnosis might mean can delay this crucial step. However, bringing these concerns to a medical professional early can significantly improve the chances of identifying manageable causes or slowing progression if a neurodegenerative condition is present. The key is to approach the conversation with honesty, clarity, and a sense of partnership with your physician. Scheduling a dedicated appointment focused solely on cognitive concerns, rather than tacking it on to a routine visit, can ensure that there’s enough time and attention to explore the issue thoroughly.
It can be helpful to prepare ahead of time by tracking symptoms over a few weeks. Take note of specific examples of memory lapses, their frequency, and how they affect daily life. Include input from trusted family members who may have observed behaviors you’ve missed or underappreciated. This information provides valuable context that helps doctors distinguish between transient memory issues and those that may signal deeper cognitive changes. Bringing a list of medications, supplements, and any recent life changes—such as sleep disruptions, major stressors, or health issues—will also support a more accurate and holistic evaluation.
When speaking with your physician, be direct yet open-ended. You might say, “Lately I’ve been more forgetful than usual, and I’m concerned it might be more than just normal aging,” or “My family has mentioned I repeat myself a lot and seem confused at times. I’d like to understand what’s going on.” These types of statements create space for a productive and respectful dialogue. Importantly, physicians are trained to treat memory concerns seriously. They won’t dismiss your experience or rush to judgment; instead, they’ll guide you through the next steps, whether that involves initial screening or a referral to a specialist.
Recognizing the need to see a doctor for memory issues doesn’t mean surrendering control—it means reclaiming it. The sooner the conversation begins, the more empowered you are to make informed decisions about your cognitive health, access appropriate resources, and implement supportive strategies for long-term wellness. Ignoring or minimizing memory changes may offer short-term relief, but it risks delaying intervention at a time when treatment could be most effective. Facing these concerns directly, with the guidance of trusted medical professionals, is a brave and constructive step toward better brain health.
Frequently Asked Questions (FAQ) on Memory Loss and Medical Evaluation
1. What are some subtle early signs that might suggest the need to see a doctor for memory loss?
Subtle signs of memory decline often go unnoticed until they begin to interfere with daily life. Some of the earliest indicators may include forgetting recent conversations, having trouble following complex instructions, or relying excessively on notes and reminders for tasks that once came easily. Others might include difficulty learning new things, increased confusion in unfamiliar environments, or uncharacteristic lapses in judgment. These changes can be gradual and may not be alarming at first, which is why it’s essential to consider a medical evaluation even when symptoms seem mild. Consulting a doctor for memory loss early can help distinguish normal aging from early cognitive impairment and provide a valuable head start on potential treatments.
2. How do doctors differentiate between memory loss caused by stress and more serious conditions?
Stress can significantly affect memory, particularly short-term recall and concentration. When someone visits a doctor for memory issues, the clinician will often begin by evaluating lifestyle factors, emotional health, and recent life changes. They may administer questionnaires to assess stress levels and screen for anxiety or depression. In contrast, more serious conditions like Alzheimer’s disease often involve a progressive decline across multiple areas of cognition, including language, spatial reasoning, and problem-solving. Objective cognitive testing and longitudinal observation help doctors distinguish between stress-induced forgetfulness and more concerning neurodegenerative changes. A doctor for memory loss will also consider how symptoms evolve over time, whether they fluctuate with stress levels, and whether they improve with relaxation or lifestyle changes.
3. What should you bring to your first appointment with a doctor for memory issues?
Being well-prepared for your first appointment with a doctor for memory issues can significantly enhance the diagnostic process. It’s important to bring a comprehensive list of current medications, including prescriptions, over-the-counter products, and supplements. In addition, prepare a detailed history of symptoms, noting when they began, how they’ve changed, and any associated triggers. If possible, bring a trusted family member or caregiver who can offer another perspective and share observations. Previous medical records, lab results, or imaging related to neurological or psychiatric issues should also be included. This proactive approach enables the doctor for memory loss to form a more complete picture and develop an appropriate plan for further evaluation or referral.
4. How can technology assist in identifying patterns that might prompt a visit to a doctor for memory loss?
Digital tools are increasingly being used to track cognitive performance over time. Smartphone apps, wearable devices, and digital calendars can help users monitor their forgetfulness and recognize patterns that might indicate a problem. For instance, repeated missed appointments or frequent reliance on prompts for basic tasks could signal something more than normal aging. Families may also use home-monitoring systems to detect behavioral changes, such as disrupted sleep or unusual wandering. When this data is shared with a doctor for memory loss, it can offer valuable context and supplement traditional diagnostic methods. These tools are especially helpful for individuals who are unsure whether their memory concerns warrant medical attention.
5. Can a doctor for memory issues help identify environmental contributors to cognitive problems?
Absolutely. A doctor for memory issues often evaluates lifestyle and environmental factors that may be contributing to cognitive symptoms. Poor indoor air quality, exposure to certain chemicals, or even chronic noise pollution can negatively impact brain health. Additionally, inadequate lighting or disorganized living spaces can increase cognitive load and stress, making memory issues appear worse. Doctors may ask about occupational exposures or home environments to rule out such influences. Identifying and addressing these subtle but significant environmental contributors can result in meaningful improvements, especially when combined with other interventions such as sleep optimization and nutritional support.
6. How do cultural beliefs influence the decision to see a doctor for memory issues?
Cultural attitudes toward aging, memory loss, and mental health can deeply influence whether someone seeks help. In some communities, forgetfulness may be seen as a normal and expected part of aging, leading to delays in recognizing when symptoms require medical evaluation. Others may fear stigma or worry that a diagnosis will lead to loss of independence or respect within the family. A culturally competent doctor for memory issues will consider these dynamics and strive to build trust by acknowledging cultural values and involving family members in the conversation. Tailoring education and outreach to align with community norms is essential in improving early detection and equitable access to care.
7. How does a doctor for memory loss approach cases where language barriers complicate communication?
Effective memory evaluation relies heavily on clear communication, which can be challenging when language differences exist. A doctor for memory loss who is experienced in cross-cultural care may use certified medical interpreters, translated assessment tools, or culturally adapted cognitive tests. Non-verbal cues and family input become especially important in these situations. It’s also vital to distinguish between true cognitive decline and misunderstandings that arise from language confusion. Physicians may need to assess fluency in both the primary and secondary language to accurately interpret test results. Ultimately, the goal is to create an environment where patients can express concerns freely and receive care that reflects their linguistic and cultural context.
8. What role do annual wellness visits play in prompting referrals to a doctor for memory issues?
Annual wellness visits, particularly for adults over 65, often include cognitive screenings as part of routine preventive care. These visits are a critical opportunity for primary care providers to detect early signs of cognitive change and initiate timely referrals. Even subtle declines in performance on brief cognitive assessments can prompt further testing or a visit to a specialist. By incorporating memory evaluations into these yearly check-ins, physicians can normalize the discussion and reduce the stigma around memory loss. A timely referral to a doctor for memory issues ensures that any necessary follow-up, whether medical or lifestyle-related, is addressed promptly and efficiently.
9. How can caregivers protect their own mental health when supporting someone who sees a doctor for memory loss?
Caring for someone with cognitive issues can be emotionally taxing, particularly as the demands increase over time. It’s common for caregivers to experience burnout, depression, or anxiety if they do not have adequate support. Attending counseling, joining caregiver support groups, and scheduling regular breaks are crucial steps to maintaining resilience. It’s also important for caregivers to stay informed by attending appointments or debriefing with the doctor for memory issues, as this helps them feel empowered and included in the care plan. When caregivers are mentally and emotionally supported, they are far better equipped to offer the consistent, compassionate assistance that individuals with memory loss require.
10. What innovations are emerging in how doctors assess and treat memory loss?
Recent innovations in memory care are transforming how doctors diagnose and manage cognitive decline. Artificial intelligence is being used to detect patterns in speech, writing, and behavior that may predict dementia years before traditional tools can. Genetic testing and advanced biomarkers, such as tau and amyloid scans, are increasingly available to help identify Alzheimer’s disease at its preclinical stages. Personalized medicine approaches are also evolving, with treatments tailored to an individual’s genetic profile, lifestyle, and risk factors. A forward-thinking doctor for memory loss is likely to incorporate these cutting-edge tools to refine diagnoses and improve outcomes. As research progresses, the future of memory care is expected to be more precise, personalized, and proactive than ever before.
Conclusion: Taking Action: The Critical Role of Medical Support in Protecting Brain Health
Memory loss, whether mild or severe, is more than just a personal inconvenience—it can be a signal from the brain that something important is changing. Responding to that signal with curiosity, medical attention, and a commitment to early intervention is one of the most powerful steps anyone can take to protect long-term mental function and well-being. Far too often, people delay addressing memory issues due to fear, embarrassment, or the mistaken belief that nothing can be done. Yet, science tells a different story: many causes of memory loss are treatable, and even when the condition is progressive, early detection offers a critical window for effective management, lifestyle adjustments, and improved quality of life.
Healthcare professionals are not just diagnosticians; they are partners in understanding the full picture of a person’s cognitive health. When you see a doctor for memory loss, you open the door to a multidisciplinary approach that includes medical testing, brain imaging, psychological evaluation, and even environmental assessments that consider the influence of stress, sleep, nutrition, and emotional well-being. This holistic evaluation doesn’t merely lead to a label—it leads to answers, direction, and hope. It allows individuals and families to make plans rooted in knowledge rather than speculation, to build support systems that meet real needs, and to access therapies that may slow decline or enhance day-to-day function.
It’s also important to understand that memory care is not a one-size-fits-all process. The brain is uniquely complex, and every person’s cognitive profile is shaped by their history, genetics, lifestyle, and health status. A doctor for memory issues is trained to look at all these factors in concert, not in isolation. This comprehensive view enables tailored interventions—whether that’s starting a new medication, joining a cognitive training program, exploring therapy for depression or anxiety, or making simple but impactful changes to sleep habits, diet, and physical activity. These personalized strategies can make a significant difference, especially when implemented early.
Most importantly, seeking medical attention for memory concerns sends a message: that cognitive health matters and deserves the same level of care, respect, and attention as any other aspect of physical health. Just as we don’t hesitate to see a doctor for persistent chest pain or blurry vision, we should not hesitate to consult a professional for recurring memory issues or confusion. The stigma surrounding memory loss is gradually fading, replaced by a growing understanding that brain health is a vital and manageable part of aging. The more we normalize these conversations, the better equipped we are to support individuals across the spectrum of cognitive changes—whether temporary, reversible, or chronic.
Whether you are noticing signs in yourself or a loved one, the time to act is now. Don’t wait for the symptoms to escalate or become undeniable. Make the appointment. Start the conversation. Ask the questions. Your brain deserves that level of care. Seeing a doctor for memory loss isn’t just about diagnosis—it’s about giving yourself the best possible chance at clarity, dignity, and well-being for years to come.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
When Do You Need to See a Memory Expert?
Investigating memory loss Memory lapses could be signs of aging or something else.
Memory lapses: What’s normal and when to see a doctor
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.


