Dementia is not a specific disease but rather a general term encompassing a range of cognitive impairments that interfere with daily life. Alzheimer’s disease is the most common form, but other types include vascular dementia, Lewy body dementia, and frontotemporal disorders. These conditions differ in pathology and progression, yet they often share early warning signs that can be subtle and easy to dismiss. Knowing what to do if you suspect someone has dementia can be the turning point in ensuring that your loved one receives appropriate care, support, and medical intervention.
Early recognition is essential for several reasons. First, certain causes of dementia-like symptoms are reversible, such as vitamin deficiencies, thyroid dysfunction, or medication interactions. If addressed promptly, cognitive decline in these cases may be halted or even reversed. Second, early diagnosis allows for better planning—both practically and emotionally. Families can make informed decisions about finances, legal matters, and care preferences before cognitive impairment progresses. Lastly, timely intervention can connect individuals with community resources and therapies that may slow progression or improve quality of life.
In clinical settings, physicians often rely on a combination of medical history, neurological exams, cognitive assessments, imaging, and laboratory tests to identify cognitive disorders. But long before a formal diagnosis is reached, it is often family, friends, or colleagues who first notice the subtle shifts: missed appointments, forgotten names, repetitive questions, or increased confusion in familiar environments. When such signs emerge, understanding what to do if you think someone has dementia becomes a vital component of health literacy and caregiving advocacy.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Identifying Cognitive Changes: From Normal Aging to Concerning Signs
Distinguishing between normal cognitive aging and early dementia symptoms can be challenging, particularly because memory lapses occur naturally as people grow older. Forgetting a name momentarily or misplacing keys occasionally does not necessarily indicate a problem. However, consistent or escalating difficulties with memory, communication, reasoning, and judgment warrant closer examination.
One of the first red flags often noticed is short-term memory loss that disrupts daily activities. This might manifest as forgetting important dates or events and repeatedly asking the same questions. Other common signs include trouble managing finances, navigating once-familiar routes, or following multi-step tasks. Some individuals begin to struggle with language, finding it hard to follow conversations or retrieve common words. Emotional changes may also surface, such as increased irritability, anxiety, or withdrawal from hobbies and social interactions.
A particularly concerning indicator is when a person becomes suspicious, paranoid, or delusional—behavior not typical of aging alone. For instance, accusing loved ones of stealing or expressing fear that strangers are plotting against them can signify neurological disruption. These behavioral shifts, coupled with declining executive function, suggest that the cognitive impairment is not simply age-related forgetfulness.
If you find yourself wondering what to do if you suspect someone has dementia in light of these behaviors, the answer lies in early engagement, compassionate communication, and seeking professional evaluation. The earlier these signs are contextualized and validated, the greater the opportunity for supportive interventions.

Initiating the Conversation: Approaching the Subject with Sensitivity
Initiating a conversation with someone about your concerns regarding their cognitive health can be daunting. Emotions like fear, denial, embarrassment, and confusion often arise, both in the person potentially experiencing symptoms and the concerned loved one. Despite this emotional terrain, it is important to express your observations and concerns with empathy, respect, and patience.
Begin by choosing a quiet, private setting where distractions are minimal. Start with open-ended questions or gently share specific examples of behaviors you’ve observed. Framing the conversation around care and support—rather than confrontation or correction—can foster trust. For example, you might say, “I’ve noticed you’ve had a hard time remembering names lately, and I’m wondering how you’re feeling about it.”
Listening is equally important as speaking. Allow the individual to respond without interruption and validate their feelings. If they express frustration or confusion, reassure them that your intention is to help and not to criticize. Avoid making assumptions or diagnosing them yourself; instead, express your willingness to accompany them to a doctor for a thorough evaluation.
For many families, this first conversation marks the beginning of a long journey. Knowing what to do if you think someone has dementia includes not only observing symptoms but also learning to navigate sensitive dialogue with compassion. These early discussions often determine how open someone may be to seeking help.
Encouraging a Professional Evaluation: The Importance of Medical Diagnosis
Once initial concerns have been discussed, the next step involves encouraging a professional evaluation. Only a licensed healthcare provider can perform the necessary assessments to determine whether dementia is present and identify its type and stage. Understanding what to do if you suspect someone has dementia includes advocating for this crucial step, even if the individual is reluctant or fearful.
The diagnostic process typically involves multiple components: a thorough review of medical history, cognitive and neuropsychological tests, physical examinations, blood tests, and imaging studies such as MRI or CT scans. These evaluations help differentiate dementia from other potential causes of cognitive impairment, such as depression, sleep disorders, or medication side effects.
Some families may face resistance when suggesting a medical appointment. In such cases, emphasizing health maintenance rather than focusing solely on memory problems can reduce defensiveness. Phrasing the appointment as a general checkup or wellness evaluation can be helpful, especially if the person is anxious or suspicious. It is also beneficial to include a healthcare provider the individual trusts, such as a long-standing primary care physician.
Early diagnosis opens the door to a wide range of interventions, including cognitive therapies, medications, and support services. Furthermore, it enables individuals to participate in their own care planning while they are still cognitively able to do so. By making a diagnosis a collaborative goal rather than a punitive judgment, families and caregivers lay a foundation for resilience and preparedness.
Building a Support Network: Caregiving with Compassion and Collaboration
Dementia affects not only the individual but also their family, friends, and caregivers. As cognitive decline progresses, everyday tasks can become overwhelming or unsafe, necessitating external support. Knowing what to do if you think someone has dementia includes assembling a network of care that spans emotional, practical, and professional domains.
Family members often take on primary caregiving roles, especially in the early and middle stages of the disease. While this can foster closeness and continuity, it can also lead to burnout, stress, and emotional strain. Caregivers must be mindful of their own well-being and recognize the value of respite care, support groups, and counseling. Organizations such as the Alzheimer’s Association and local Area Agencies on Aging can provide invaluable resources, including caregiver education, support networks, and respite services.
Professional caregivers and home health aides may become necessary as needs intensify. Their training allows them to manage behaviors, assist with personal care, and ensure safety, especially for individuals prone to wandering or falls. In some cases, memory care facilities or assisted living communities with dementia units offer structured environments with 24-hour supervision.
Community support plays an integral role in dementia care. Involving neighbors, friends, clergy, or community centers can provide additional layers of companionship and security. From medication reminders to meal preparation, simple acts of help can significantly ease the burden on primary caregivers and promote a higher quality of life for the person with dementia.
Planning for the Future: Legal, Financial, and Ethical Considerations
Dementia is a progressive condition, and as it advances, decision-making becomes increasingly difficult. Planning for the future while the person can still participate in the process is not only pragmatic but ethically sound. One of the most critical components of understanding what to do if you suspect someone has dementia is initiating early discussions about legal and financial matters.
This planning should include designating a durable power of attorney for both healthcare and finances, establishing advance directives, and reviewing or updating wills and estate plans. Engaging a qualified elder law attorney can help ensure that these documents comply with state laws and reflect the individual’s preferences and values. Transparent communication about these arrangements can prevent conflicts among family members and reduce uncertainty during later stages.
Financial planning is also essential, particularly given the long-term costs of care. This includes evaluating insurance coverage, retirement benefits, Medicaid eligibility, and other funding options. Long-term care insurance, if already in place, may provide critical support. Families should also explore local and national programs that offer financial assistance or subsidized services.
Beyond practical considerations, ethical issues often emerge in dementia care. These may include questions about autonomy, driving, safety, and medical decision-making. Balancing respect for the individual’s dignity with the need to protect them from harm requires nuanced judgment and, often, the guidance of medical professionals, legal advisors, and ethics committees.
Fostering Dignity and Engagement: Maintaining Quality of Life After Diagnosis
A dementia diagnosis does not mean an immediate or complete loss of agency. Many individuals in the early stages continue to lead active, fulfilling lives with proper support and accommodations. Recognizing what to do if you think someone has dementia involves creating environments and routines that support independence, purpose, and joy.
Cognitive stimulation is beneficial and can include puzzles, music therapy, reading, art, and reminiscing activities. These engagements tap into preserved abilities and promote self-expression. Physical activity also plays a vital role, supporting cardiovascular health, reducing agitation, and preserving mobility. Walks, gentle exercises, and balance training contribute to both mental and physical well-being.
Diet and sleep hygiene should not be overlooked. Balanced nutrition supports overall brain health, while establishing calming bedtime routines can improve sleep patterns disrupted by sundowning or restlessness. In some cases, occupational therapy may be useful for adapting the home environment to ensure safety while preserving autonomy.
It is also essential to nurture emotional and spiritual well-being. Supportive relationships, participation in faith communities, or engaging in meaningful rituals help sustain identity and reduce feelings of isolation. By focusing on the whole person—not just the diagnosis—caregivers and loved ones affirm the humanity and worth of those living with dementia.
When and Where to Seek Help: Leveraging Resources for Comprehensive Care
As dementia progresses, care needs often become more complex. Knowing when to seek additional help and where to find it is a key aspect of what to do if you suspect someone has dementia. Resources span medical, social, legal, and psychological domains, and accessing them early can make a meaningful difference.
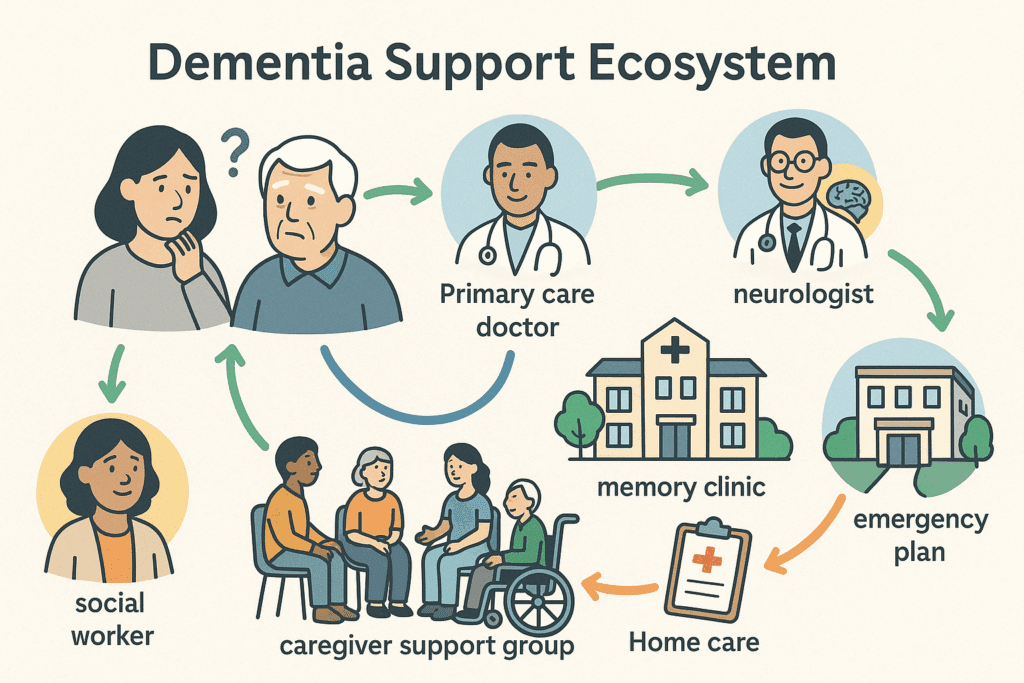
Primary care physicians and neurologists are usually the first point of medical contact. However, geriatricians, neuropsychologists, and dementia care specialists may offer more targeted evaluations and treatment strategies. Memory clinics and Alzheimer’s research centers may provide access to clinical trials and cutting-edge therapies. Social workers and case managers can coordinate services and connect families with relevant support systems.
Mental health professionals can assist both individuals and caregivers in managing anxiety, depression, grief, and role transitions. Therapy can be instrumental in processing emotions and developing coping strategies. Group therapy or caregiver support groups provide opportunities to share experiences and gain practical advice.
In emergencies or crisis situations—such as severe agitation, hallucinations, or wandering—it is crucial to have a plan in place. This might involve contacting emergency services, visiting urgent care centers, or arranging temporary respite stays. Having critical information readily available, such as a list of medications and emergency contacts, can expedite responses and minimize harm.
Empowering families with knowledge and resources ultimately strengthens the care experience and reduces the sense of isolation and overwhelm. Proactive engagement with these services reinforces the message that no one has to navigate dementia alone.
Frequently Asked Questions: What to Do If You Suspect Someone Has Dementia
1. Can changes in sleep patterns be an early indicator of dementia, and how should families respond?
Yes, disrupted sleep-wake cycles, such as excessive daytime napping or restlessness at night, can be among the earliest behavioral changes in dementia. Families who observe such patterns often wonder what to do if they suspect someone has dementia, especially when sleep issues begin interfering with daily functioning. In these cases, it’s important to document sleep habits and discuss them with a healthcare provider, as changes in circadian rhythm may indicate underlying neurological issues. Improving sleep hygiene—including establishing consistent routines, reducing evening screen time, and limiting caffeine—may help, but professional evaluation is essential. A sleep study or neurological assessment may uncover connections between sleep disturbances and cognitive changes that warrant further exploration.
2. How do social withdrawal and changes in conversation style suggest cognitive decline?
People in early stages of dementia may begin withdrawing from social settings, avoiding phone calls, or disengaging from conversations due to fear of embarrassment or confusion. Loved ones who notice someone repeating themselves frequently, losing track of topics, or becoming unusually quiet might start questioning what to do if they think someone has dementia. These communication issues are often subtle and can be mistaken for depression or fatigue. One strategy is to gently re-engage the person in conversations centered around familiar topics while observing if patterns of confusion or word-finding difficulty persist. If the individual continues to avoid interaction or expresses frustration over speaking, a cognitive screening by a professional becomes advisable.
3. What role does nutrition play in identifying and managing early dementia symptoms?
Nutrition is often overlooked in discussions about cognitive decline, but it plays a critical role in both identifying and managing symptoms. Unintentional weight loss, disinterest in food, or forgetting how to prepare meals can be early signs that raise the question of what to do if you suspect someone has dementia. Diets rich in antioxidants, omega-3 fatty acids, and B vitamins support brain health and may help delay progression. Family members should monitor pantry contents, expired items, or repeated grocery purchases as indicators of declining executive function. Engaging a registered dietitian early on can help ensure nutritional adequacy while tailoring meals to evolving needs.
4. How can technology assist when you think someone has dementia but they’re resistant to help?
Resistance to assistance is common, especially when a person doesn’t recognize or accept their cognitive changes. For those wondering what to do if they think someone has dementia but face pushback, discreetly implemented technology can provide safety and peace of mind. GPS-enabled watches, medication reminder apps, and voice assistants can support independence while quietly offering monitoring features. Smart home devices that control lighting and appliances can reduce hazards without appearing intrusive. These tools allow caregivers to honor autonomy while maintaining a protective oversight, especially during the early phases when overt supervision might be resented.
5. Are there community-based programs that help evaluate and support those with suspected dementia?
Yes, numerous community-based resources are available to those unsure of what to do if they suspect someone has dementia but are not ready for a clinical evaluation. Many local senior centers, Area Agencies on Aging, and nonprofit organizations offer memory screening events, caregiver education, and access to social workers. Some public libraries and health departments now partner with dementia-friendly initiatives to host workshops and support groups. These programs can provide a low-pressure entry point for concerned families to begin the conversation without jumping immediately into formal diagnostics. Accessing these community services also helps build a network of support from the outset.
6. How does driving behavior serve as an early barometer of cognitive change?
A decline in driving skills—such as increased fender benders, difficulty navigating familiar routes, or trouble interpreting traffic signals—can signal early-stage dementia. For those asking what to do if you think someone has dementia, paying attention to their driving habits is a prudent and revealing step. Families should ride along and observe behaviors without drawing premature conclusions, taking note of spatial awareness and reaction time. Occupational therapists specializing in driver rehabilitation can offer assessments that gauge road safety objectively. Approaching the subject of driving restrictions requires sensitivity and, when possible, presenting it as a temporary safety measure pending evaluation.
7. How do financial missteps and changes in money management signal deeper cognitive issues?
Difficulty managing finances is often one of the earliest signs that something may be wrong, and many families begin to wonder what to do if they suspect someone has dementia when bills are unpaid, suspicious purchases appear, or bank accounts are mismanaged. These issues can indicate declining executive function, impaired judgment, or vulnerability to scams. Introducing financial oversight tools such as joint accounts, spending alerts, or professional fiduciary services can help safeguard assets while preserving dignity. It’s wise to address these concerns early and tactfully, involving a trusted advisor or attorney when necessary to formalize powers of attorney.
8. Is there a benefit to starting dementia-friendly activities before a formal diagnosis is made?
Absolutely. Once you suspect someone may be showing signs of cognitive decline, integrating dementia-friendly routines can provide structure and stimulation without needing a diagnosis to justify them. For example, puzzle-solving, art projects, gentle exercise, and music therapy have demonstrated cognitive and emotional benefits. If you’re considering what to do if you suspect someone has dementia, initiating such activities can also serve as informal assessments of how the person engages, processes, and recalls information. Early participation in these engagements may ease anxiety, strengthen bonds, and help caregivers evaluate the need for further support.
9. How can emotional intelligence and body language help you communicate concerns without confrontation?
Non-verbal cues often speak louder than words, especially when discussing sensitive topics like cognitive decline. If you’re weighing what to do if you think someone has dementia, consider your tone, facial expressions, and physical posture when raising concerns. A calm, reassuring presence can help de-escalate defensiveness, while leaning in slightly and maintaining gentle eye contact conveys empathy. Avoid crossing arms or adopting accusatory tones, which may trigger resistance. By matching your verbal message with non-threatening body language, you build an emotional bridge that encourages openness and trust.
10. What proactive steps can adult children take if their parent refuses medical evaluation?
When a parent resists seeing a doctor despite clear warning signs, adult children often grapple with what to do if they suspect someone has dementia but feel powerless to intervene. In such situations, it’s crucial to prioritize relationship preservation while still advocating for safety. Framing the appointment as a routine wellness check or involving a respected third party, such as a clergy member or long-time friend, can ease resistance. Documenting incidents and patterns in writing also helps if guardianship or power of attorney eventually becomes necessary. Most importantly, maintaining a dialogue built on empathy and trust increases the likelihood that the parent will become receptive to help over time.
Conclusion: Taking Informed and Compassionate Action When You Suspect Dementia
Ultimately, understanding what to do if you suspect someone has dementia equips families, friends, and caregivers with the tools to make a meaningful difference in someone’s life. The process begins with recognizing early signs and continues through sensitive conversations, timely medical assessments, and the construction of a robust, compassionate support system. From the initial concerns to the complex demands of long-term care, each stage benefits from thoughtful planning and evidence-based action.
By taking initiative early and approaching the journey with empathy and informed advocacy, individuals can help preserve the dignity and quality of life for those affected by dementia. This proactive stance allows for the development of care strategies that are personalized, respectful, and responsive to the evolving nature of cognitive decline. Moreover, staying connected with medical professionals, legal advisors, and community resources ensures that care remains comprehensive and grounded in best practices.
As dementia continues to impact millions of individuals and families globally, the knowledge of what to do if you think someone has dementia becomes not only a personal asset but also a societal necessity. Through awareness, collaboration, and unwavering compassion, we can foster a world where individuals with dementia are not only cared for but deeply valued and understood.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Interventions for helping people recognise early signs of recurrence in bipolar disorder
The Importance Of Early Detection In Intervention Strategies
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.


