The digestive system, often overlooked until it signals distress, plays a crucial role in overall well-being. Among its many components, the colon—also known as the large intestine—is a critical player in nutrient absorption, waste elimination, and the regulation of gut flora. Yet, when colon problems arise, they can manifest subtly at first, disguising themselves as common gastrointestinal discomfort. Over time, however, untreated colon issues may progress, sometimes signaling more serious underlying conditions such as inflammatory bowel disease or even colorectal cancer. Understanding how to recognize colon problem symptoms early is essential for prevention, timely intervention, and improved long-term outcomes.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
The Link Between Digestive Health and Whole-Body Wellness
While colon health is a topic frequently confined to the gastroenterologist’s office, it should be part of the broader wellness conversation. The colon is home to trillions of bacteria that influence not only digestion but also immune system function, mood regulation, and systemic inflammation. When colon issues disrupt this delicate balance, symptoms can ripple beyond the digestive tract, affecting energy levels, mental clarity, and emotional well-being. Recognizing early symptoms and seeking medical guidance promptly helps preserve this balance, fostering both physical and mental health.
Importantly, early signs of colon problems are not always dramatic. A slight but persistent change in bowel habits, new onset bloating, or mild abdominal discomfort might not initially raise alarm. However, these subtle signals often precede more serious developments. The challenge lies in distinguishing normal fluctuations in digestion from symptoms that warrant professional evaluation. Heightened awareness, paired with evidence-based knowledge, empowers individuals to take charge of their health before conditions worsen.
Understanding Common Colon Problem Symptoms
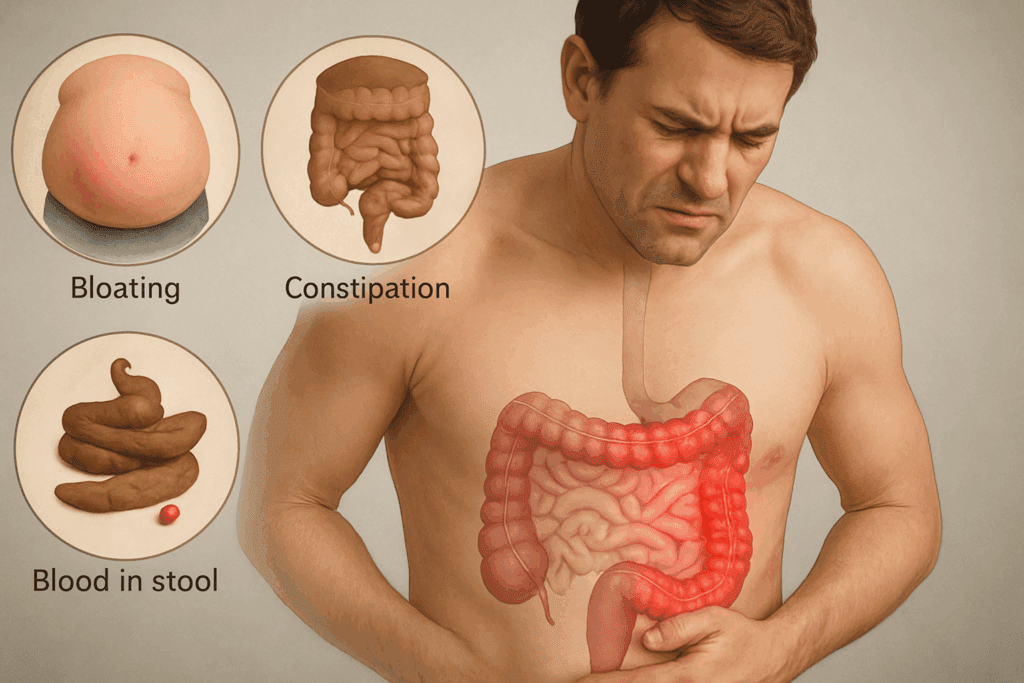
Colon problem symptoms can vary widely depending on the underlying cause, ranging from mild irritations to indicators of life-threatening disease. Constipation and diarrhea, though common and often benign, may signal deeper issues when persistent. In cases where symptoms extend beyond a few days, or recur frequently without a clear dietary or lifestyle explanation, they may point toward more significant colon issues. Chronic bloating, excessive gas, and a feeling of incomplete evacuation after a bowel movement can also suggest abnormal colon function or inflammation.
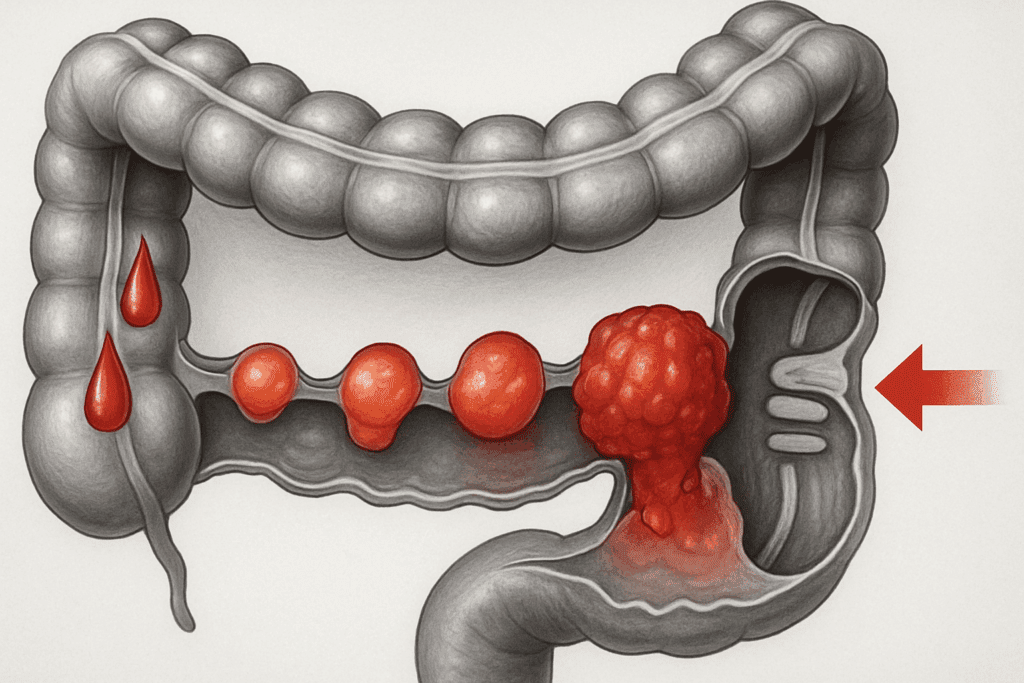
Blood in the stool—whether bright red or dark and tarry—should always be taken seriously. Though sometimes caused by hemorrhoids or minor tears, it may also indicate colon polyps, diverticulosis, or early signs of intestinal cancer. Pain in the lower abdomen, especially when localized and recurring, can be a symptom of diverticulitis, irritable bowel syndrome, or even obstruction. Other concerning symptoms include unexplained weight loss, persistent fatigue, and a noticeable change in stool consistency or color.
Individuals who experience these colon problem symptoms should consult a healthcare provider for proper evaluation. Diagnostic tests, including colonoscopy, sigmoidoscopy, and stool sample analysis, can identify inflammation, blockages, or abnormal growths. Early diagnosis is particularly critical for conditions such as colorectal cancer, where early-stage detection significantly improves survival rates.
Recognizing the Subtle Indicators of Colon Issues
Not all colon issues announce themselves with urgency. Many begin with subtle signs that can easily be dismissed or attributed to temporary dietary choices or stress. For instance, a persistent feeling of fullness or pressure in the lower abdomen, even after a complete bowel movement, may be an early warning sign. Similarly, minor shifts in the frequency or texture of stool, especially if they become the new norm, deserve attention.
Colon issues symptoms can also manifest through non-gastrointestinal complaints. Chronic fatigue, difficulty concentrating, or frequent headaches may stem from systemic inflammation linked to poor colon health. When the colon is inflamed or dysregulated, the body’s ability to absorb nutrients is compromised, often leading to deficiencies in iron, B vitamins, and magnesium—each of which contributes to energy production and cognitive function.
Skin issues, too, can reflect deeper digestive imbalances. Conditions like eczema, acne, or unexplained rashes sometimes have roots in gut dysfunction. When toxins are not efficiently eliminated through the colon, they may circulate in the bloodstream, provoking inflammatory skin responses. Thus, persistent skin problems that do not respond to conventional treatment should prompt a broader investigation into digestive health.
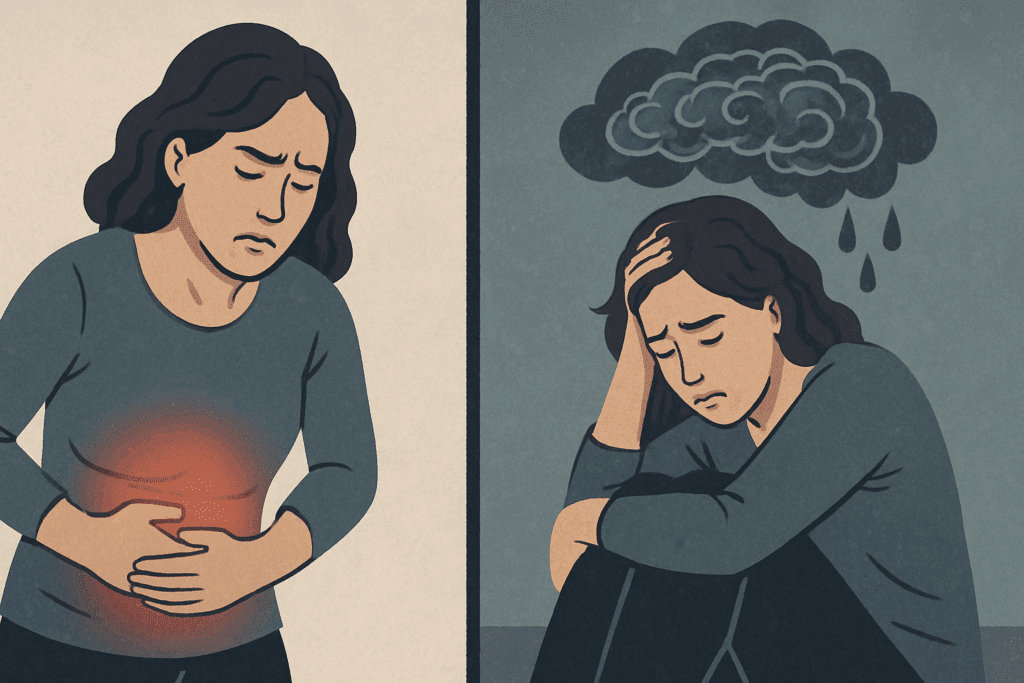
Colon Issues and Their Psychological Impact
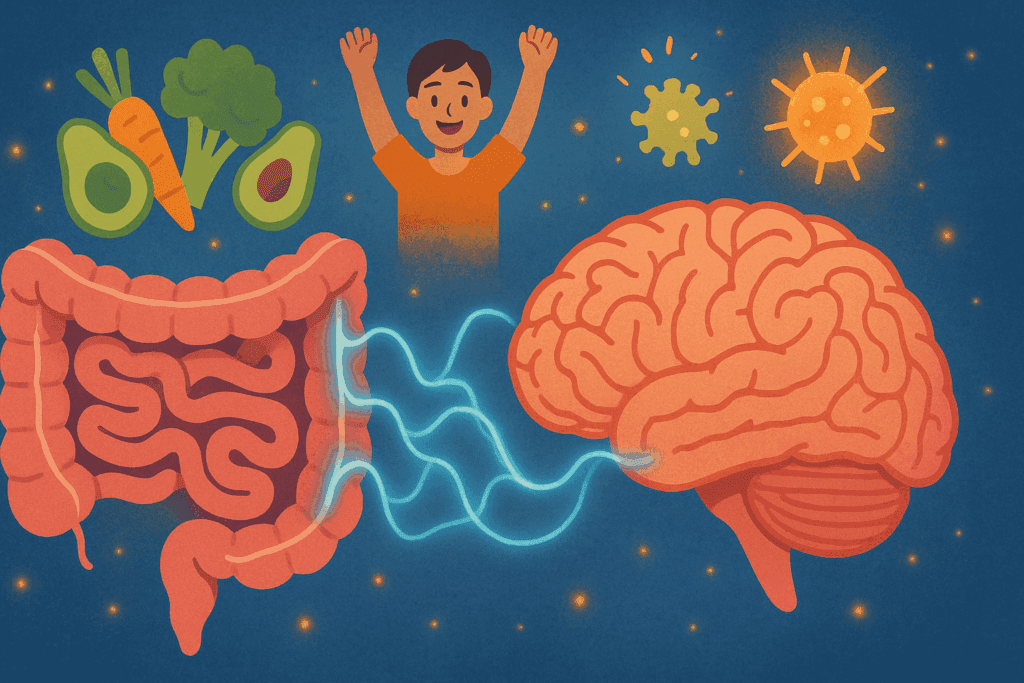
The connection between the brain and the gut is well-established, often referred to as the gut-brain axis. Emotional distress, anxiety, and depression are frequently reported in individuals with chronic colon problems. This link is not merely psychosomatic; the colon produces and regulates neurotransmitters like serotonin, which influence mood and emotional regulation. When colon health deteriorates, it can lead to chemical imbalances that directly affect mental well-being.
Patients with irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or chronic constipation often report heightened levels of stress and anxiety. In some cases, these psychological symptoms may precede or exacerbate physical colon issues, creating a feedback loop that complicates treatment. Cognitive behavioral therapy, mindfulness techniques, and gut-directed hypnotherapy have all shown promise in improving both the psychological and physical symptoms of colon dysfunction.
Acknowledging the bidirectional relationship between colon issues and mental health encourages a more holistic approach to diagnosis and treatment. Rather than focusing solely on physical symptoms, addressing emotional well-being can lead to more sustainable health outcomes. This integrated approach aligns with growing evidence supporting the importance of treating the person, not just the problem.
Intestinal Cancer Symptoms and the Urgency of Early Detection
One of the most pressing reasons to monitor colon health is the risk of intestinal cancer. Also referred to as colorectal cancer when it involves the colon or rectum, this disease often develops silently, progressing through benign polyps that gradually become malignant. Intestinal cancer symptoms in their early stages are frequently overlooked because they mimic common gastrointestinal complaints. These include changes in bowel habits, rectal bleeding, unexplained anemia, and persistent abdominal discomfort.
As cancer progresses, more specific symptoms may emerge, such as a narrowing of the stool, a sense of incomplete evacuation, or visible blood in the stool. Unintentional weight loss, chronic fatigue, and appetite changes are additional red flags. Unfortunately, by the time these symptoms become pronounced, the cancer may have advanced to a stage where treatment becomes more complex.
Routine screening is the most effective method of early detection. Guidelines generally recommend that individuals begin colon cancer screening at age 45, earlier if there is a family history or known genetic predisposition. Colonoscopy remains the gold standard, allowing for the detection and removal of precancerous polyps during the same procedure. Non-invasive options, such as stool DNA tests, are also available but may be less sensitive. Recognizing and acting on intestinal cancer symptoms can dramatically improve prognosis and reduce mortality rates.
Risk Factors Contributing to Colon Problems
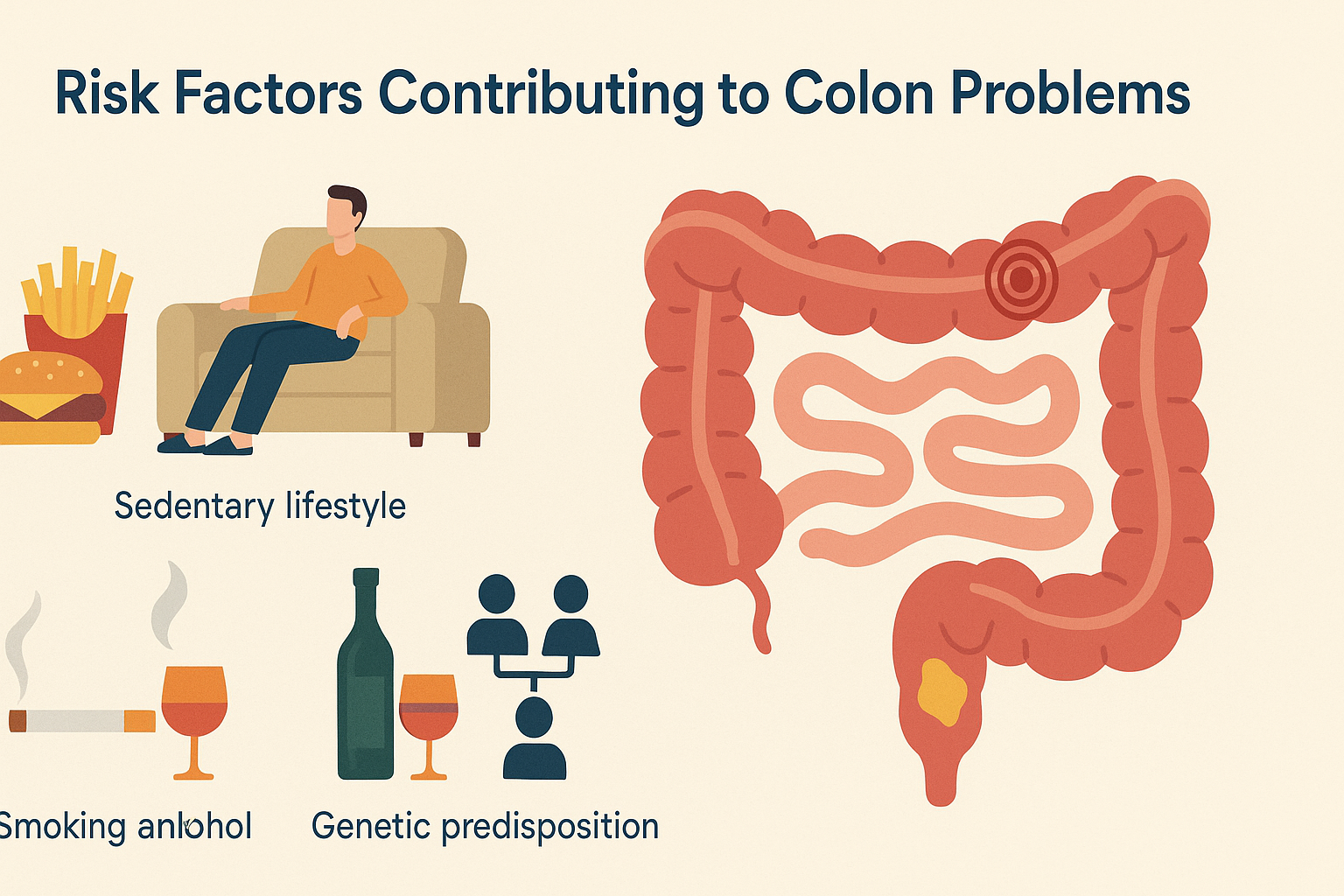
Understanding the risk factors that contribute to colon issues can empower individuals to make lifestyle changes that support long-term digestive health. Diet plays a pivotal role, with high intake of processed meats, refined carbohydrates, and low fiber levels being associated with increased risk of colon disease. Fiber-rich diets that include whole grains, fruits, and vegetables support regular bowel movements and promote a healthy microbiome, reducing inflammation and carcinogen exposure in the colon.
Sedentary behavior is another critical factor. Regular physical activity supports healthy bowel motility and helps maintain a healthy weight, both of which are protective against colon cancer and other colon problems. Smoking and excessive alcohol consumption further increase the risk of colon issues, as they contribute to inflammation and oxidative stress in the gastrointestinal tract.
Genetic predisposition also plays a role. Individuals with a family history of colon polyps or colorectal cancer should be particularly vigilant, as they may carry inherited mutations like Lynch syndrome or familial adenomatous polyposis (FAP). These conditions dramatically increase the likelihood of developing intestinal cancer, making early and frequent screening essential.

The Role of Gut Microbiota in Colon Health
The colon houses the densest concentration of microbiota in the human body, comprising a complex community of bacteria, fungi, and viruses that work symbiotically with their host. When balanced, these microbes assist in breaking down dietary fibers, synthesizing essential vitamins, and regulating immune responses. However, disruptions in this ecosystem—termed dysbiosis—are closely linked to a variety of colon problems.
Dysbiosis has been implicated in conditions ranging from irritable bowel syndrome to colorectal cancer. Imbalances in gut flora can promote chronic inflammation, reduce colon barrier integrity, and allow harmful pathogens to proliferate. Diet, antibiotics, stress, and illness all influence the composition of gut microbiota. Restoring balance through the use of probiotics, prebiotics, and diverse, fiber-rich foods may reduce colon issues symptoms and support broader health goals.
Research into the gut microbiome is rapidly expanding, with emerging evidence suggesting its role not only in digestive disorders but also in systemic diseases including obesity, autoimmune conditions, and even neurodegenerative disorders. As science deepens its understanding, microbiota-targeted therapies may become a cornerstone of colon disease prevention and treatment strategies.
When to Seek Medical Evaluation
Despite the stigma that still surrounds discussions of bowel habits, delaying evaluation of colon problem symptoms can be dangerous. If symptoms such as unexplained bleeding, persistent constipation or diarrhea, or abdominal pain last longer than a few weeks, medical attention is warranted. These symptoms should not be dismissed as minor inconveniences, particularly if accompanied by fatigue, weight loss, or anemia.
Healthcare providers can perform a range of diagnostic tests to identify or rule out serious conditions. These may include fecal occult blood tests, imaging studies like CT colonography, or direct visualization through colonoscopy. In many cases, early detection of benign or precancerous conditions allows for minimally invasive treatment, preventing progression to more severe disease.
It is equally important to advocate for oneself in the healthcare system. Individuals who feel their concerns are not being taken seriously should seek a second opinion or consult a gastroenterologist directly. Timely intervention not only improves outcomes but may also prevent the need for more aggressive treatments such as surgery or chemotherapy.
Practical Steps for Supporting Colon Health
While some colon issues arise from genetic predisposition or unavoidable environmental exposures, many are influenced by modifiable lifestyle factors. Maintaining a balanced, fiber-rich diet remains one of the most effective ways to support colon health. Fiber not only promotes regular bowel movements but also feeds beneficial gut bacteria that protect against inflammation and carcinogenesis.
Hydration is equally important. Adequate fluid intake ensures smooth passage of waste through the colon and prevents constipation. Physical activity contributes by stimulating peristalsis—the muscle contractions that move stool through the intestines—while also supporting metabolic and immune health.
Regular screenings, even in the absence of symptoms, are vital. Colonoscopy is a preventive tool, not just a diagnostic one. By removing precancerous polyps early, it prevents cancer from developing altogether. Individuals with high-risk factors should work with their healthcare providers to create a personalized screening schedule.
Addressing stress and maintaining emotional health also contribute to better colon function. Mindfulness practices, adequate sleep, and therapy can reduce gut-related anxiety and improve symptom management for those with chronic conditions. A holistic view of health that incorporates both physical and psychological well-being yields the most sustainable results.
Frequently Asked Questions: Recognizing Colon Problem Symptoms Early
1. Can stress or anxiety trigger colon problem symptoms even in otherwise healthy individuals?
Yes, psychological stress can significantly influence colon health, even among those without underlying disease. Chronic anxiety or high levels of stress can disrupt the autonomic nervous system and trigger irregular bowel movements, leading to colon issues such as cramping, bloating, or urgency. For some people, these symptoms mimic those of serious colon problems, despite an absence of structural abnormalities. The gut-brain axis, which links the central nervous system with gastrointestinal function, helps explain how emotional distress can manifest as physical colon issues symptoms. Over time, if unmanaged, stress-related bowel symptoms may contribute to more persistent colon problem symptoms and warrant further evaluation to rule out coexisting conditions.
2. How do colon problems affect long-term nutrient absorption and metabolic health?
While the small intestine is primarily responsible for nutrient absorption, colon health still plays a critical role in overall metabolic stability. When colon issues such as inflammation, dysbiosis, or impaired motility occur, they can indirectly hinder absorption by altering the balance of gut bacteria and slowing digestive transit. This imbalance can disrupt fermentation processes that produce short-chain fatty acids, which are essential for colonocyte energy and systemic metabolic regulation. Chronic colon problem symptoms may therefore be linked to subtle nutrient deficiencies, particularly in magnesium, folate, and vitamin K. Over time, these deficiencies can contribute to fatigue, immune dysfunction, and reduced resilience against disease.
3. What emerging diagnostic tools are improving early detection of intestinal cancer symptoms?
In recent years, advancements in non-invasive diagnostics have significantly improved early detection of intestinal cancer symptoms. Stool DNA testing, for example, can identify genetic mutations and blood traces associated with early-stage colorectal cancer or advanced adenomas. Liquid biopsy techniques, although still under investigation, show promise in detecting circulating tumor DNA long before traditional symptoms emerge. Additionally, artificial intelligence is being integrated into colonoscopy technology to enhance the identification of polyps, including flat lesions that are harder to detect. These innovations offer hope for identifying intestinal cancer symptoms well before progression, especially in populations where standard screening uptake is low.
4. Are colon issues symptoms always linked to visible changes in bowel habits?
Not necessarily. Many early-stage colon problems present without dramatic changes in bowel frequency or consistency, making them difficult to identify without medical evaluation. Some individuals may experience subtle shifts such as increased urgency, mild bloating, or a vague sensation of incomplete evacuation that doesn’t align with overt constipation or diarrhea. Others may notice fatigue, low-grade anemia, or even back discomfort without associating these with colon issues. It is crucial to recognize that colon issues symptoms can evolve slowly and appear indirectly, requiring a high index of suspicion and awareness to pursue timely diagnostic investigation.
5. How can lifestyle changes help prevent or minimize colon problem symptoms in high-risk individuals?
For individuals with a family history of colorectal disease or prior colon issues, proactive lifestyle adjustments can serve as a powerful preventive strategy. A diet rich in fiber, polyphenols, and resistant starch supports beneficial gut flora and minimizes inflammation linked to colon problem symptoms. Physical activity improves motility and enhances gut-brain communication, while limiting processed meats and alcohol reduces exposure to carcinogenic compounds. Stress management through techniques such as yoga, cognitive behavioral therapy, or biofeedback can further reduce colon issues symptoms that are stress-sensitive. Regular screening, guided by personal risk factors, remains foundational in preventing intestinal cancer symptoms from progressing unnoticed.
6. Can unresolved colon problems affect cognitive function or brain health over time?
Emerging research suggests a strong link between chronic colon issues and cognitive performance, particularly through the gut-brain axis and systemic inflammation. When colon problem symptoms persist, they can fuel low-grade inflammation that crosses the blood-brain barrier, potentially impairing memory, focus, and mood. Disruptions in gut microbiota also affect neurotransmitter production, notably serotonin and gamma-aminobutyric acid (GABA), which regulate emotional and cognitive stability. Inflammatory markers associated with colon issues symptoms have even been found elevated in patients with neurodegenerative conditions like Parkinson’s and Alzheimer’s. Maintaining colon health may therefore be integral not only for digestive comfort but also for preserving long-term mental clarity.
7. How do colon issues differ between younger adults and older populations?
While colon problems can affect all age groups, their presentation and implications often vary significantly across the lifespan. In younger adults, colon issues symptoms are more likely to be functional, such as those seen in irritable bowel syndrome (IBS), and often triggered by stress or dietary intolerances. In contrast, older individuals face a higher likelihood of structural changes such as diverticulosis, ischemic colitis, or polyps that may progress to intestinal cancer if untreated. Additionally, elderly patients may underreport symptoms due to normalization of discomfort, or they may experience atypical signs like unexplained anemia or cognitive changes. These differences highlight the need for age-tailored diagnostic strategies and a nuanced understanding of how colon problem symptoms evolve with aging.
8. What role does sleep play in the development or exacerbation of colon issues?
Sleep quality and circadian rhythm disruptions can significantly impact gastrointestinal health, particularly in individuals predisposed to colon issues. Sleep disturbances can alter the secretion of key digestive hormones such as melatonin and cortisol, both of which regulate motility and immune function in the colon. Poor sleep has been linked to increased intestinal permeability, or “leaky gut,” which may intensify colon issues symptoms through heightened inflammation and immune dysregulation. Studies also suggest that night-shift workers and those with sleep apnea have a higher prevalence of gastrointestinal complaints, including chronic constipation and bloating. Optimizing sleep hygiene may therefore be a practical yet underrecognized strategy in managing chronic colon problems.
9. How do hormonal fluctuations impact colon problem symptoms, particularly in women?
Hormonal shifts, especially those related to the menstrual cycle, pregnancy, and menopause, can significantly modulate colon function and trigger or worsen colon issues symptoms. Estrogen and progesterone influence gut motility and sensitivity, which is why many women report increased bloating, cramping, or altered bowel habits during different phases of their cycle. During pregnancy, the growing uterus and hormonal changes can slow digestion and exacerbate existing colon problems, including hemorrhoids and constipation. Postmenopausal changes in hormone levels may also affect microbiome composition and barrier integrity in the colon, raising the risk for chronic inflammation. Recognizing these patterns can lead to more personalized care strategies that address both hormonal and digestive health.
10. What future therapies are being developed to address persistent colon issues symptoms?
The future of colon health management is moving toward more personalized, microbiome-focused treatments that address root causes rather than just symptoms. Fecal microbiota transplantation (FMT), already used for refractory Clostridioides difficile infections, is being explored for broader use in chronic colon problems such as ulcerative colitis and irritable bowel syndrome. Next-generation probiotics, designed to deliver targeted bacterial strains, are also under development to restore microbial balance and alleviate colon issues symptoms. Advances in precision nutrition aim to tailor diets based on an individual’s microbiome profile, potentially reducing inflammation and improving tolerance to specific foods. These innovations signal a shift from one-size-fits-all treatment to customized interventions that support lasting colon health and reduce the long-term burden of intestinal cancer symptoms and related disorders.
A Final Word on Recognizing Colon Problem Symptoms Early
Recognizing colon problem symptoms early offers one of the best opportunities to safeguard long-term digestive and overall health. From minor changes in bowel habits to more ominous signs like unexplained bleeding or persistent abdominal discomfort, the body often sends clear signals when something is amiss. Listening to these cues—rather than dismissing or delaying action—can make the difference between early intervention and advanced disease.
Whether it is the early detection of intestinal cancer symptoms, management of chronic colon issues symptoms, or addressing systemic imbalances rooted in gut dysfunction, proactive health literacy is key. The colon is not merely a passive conduit for waste but a dynamic organ deeply intertwined with immunity, mood, metabolism, and overall vitality. Prioritizing its health through mindful lifestyle choices, routine screening, and timely medical consultation is a foundational step in holistic wellness.
As scientific understanding of the gut-brain connection and microbiome expands, the importance of digestive health will only grow. Individuals who learn to recognize and respond to colon problem symptoms with urgency and informed care stand to benefit not only in terms of disease prevention but also in enhanced quality of life. In the realm of preventive medicine, few actions are more empowering than listening to what your digestive system is trying to tell you.
digestive tract health, signs of bowel disease, gastrointestinal inflammation, early detection of colon cancer, gut microbiome balance, bowel movement changes, rectal bleeding concerns, gastrointestinal wellness, bloating and discomfort, colorectal screening options, fiber and digestive health, symptoms of gastrointestinal distress, inflammatory bowel conditions, probiotics for gut health, abdominal pain causes, gut-brain connection, cancer screening guidelines, stool irregularities, lifestyle and gut health, functional digestive symptoms
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out
Further Reading:
Colon cancer – Symptoms and causes
Nine Colon Cancer Symptoms You Should Not Ignore
How to Know Your Colon is Healthy
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.