The human brain is the most complex and enigmatic organ in the body, orchestrating every sensation, movement, emotion, and memory. It is therefore no surprise that brain-related diseases can significantly alter a person’s quality of life. While common brain disorders like Alzheimer’s disease or Parkinson’s disease are frequently discussed in both clinical settings and public discourse, rare brain disorders often remain in the shadows. These conditions, though less prevalent, are no less devastating, and they present unique diagnostic and therapeutic challenges. Understanding the broad landscape of brain conditions, including rare and common illnesses, is essential not only for patients and caregivers but also for clinicians, researchers, and public health advocates.
Rare brain disorders, by definition, affect a small percentage of the population, but their impact is disproportionately profound. Many rare brain conditions emerge without warning, disrupt neurological function in complex ways, and are difficult to diagnose due to their obscurity. Yet, they are part of a larger spectrum of brain disorders and diseases that collectively underscore the fragility and resilience of the nervous system. As science advances, so does our capacity to identify, manage, and potentially prevent these elusive conditions. This article offers a comprehensive exploration of brain illnesses and symptoms, delving into their diversity, clinical manifestations, diagnostic hurdles, and avenues for treatment and support.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Defining Brain Disorders and Their Classification
Brain disorders, or brain medical conditions, encompass a wide range of pathological states that interfere with normal brain function. These conditions may arise from structural abnormalities, genetic mutations, autoimmune processes, infections, trauma, or degenerative changes over time. The diversity within the list of brain diseases and disorders is staggering, ranging from common brain diseases such as migraine and epilepsy to rare brain conditions like Creutzfeldt-Jakob disease and Rasmussen’s encephalitis.
A useful classification system divides these disorders into categories based on their underlying mechanisms or affected areas. For instance, neurodegenerative disorders such as Huntington’s disease involve progressive neuronal death, while demyelinating conditions like multiple sclerosis result from immune-mediated damage to the myelin sheath. Infections like encephalitis, metabolic conditions like Leigh syndrome, and vascular brain problems like stroke each belong to distinct subsets within the brain diseases list. Regardless of origin, these brain ailments share a common feature: they alter the delicate equilibrium required for optimal brain function.
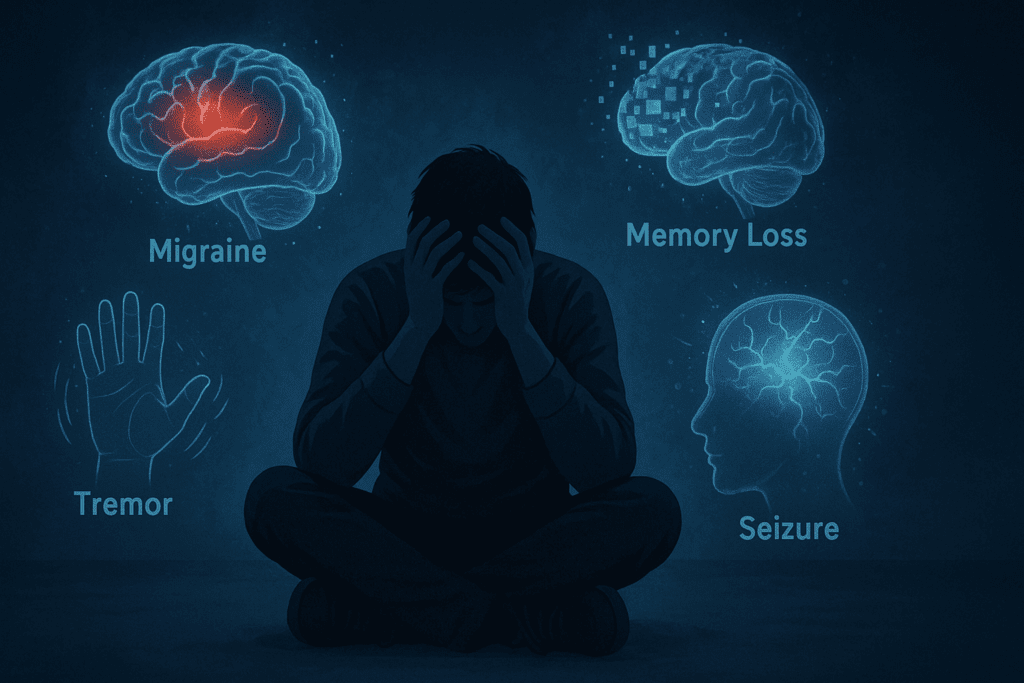
Common Brain Disorders and Diseases: Recognizing the Signs
While the term “common brain disorders” may imply a lesser degree of severity, these conditions are often life-altering and demand significant medical attention. Conditions such as epilepsy, migraine, and major depressive disorder are among the most prevalent, yet each presents with its own unique set of brain condition symptoms. Epilepsy, for example, is characterized by recurrent seizures resulting from abnormal electrical activity in the brain. Migraines, on the other hand, may present as recurrent headaches accompanied by visual disturbances, nausea, and sensitivity to light or sound.
Even among the top 10 brain diseases, symptoms can vary widely. Alzheimer’s disease, a leading cause of dementia, leads to progressive memory loss and cognitive decline, while Parkinson’s disease manifests with tremors, stiffness, and slowed movement. These brain problems and symptoms can interfere with day-to-day activities, often progressing gradually and insidiously. Early diagnosis and intervention are key to managing these brain illnesses effectively, as treatments tend to be more successful when initiated in the early stages of the disease.
The Challenge of Rare Brain Disorders
Rare brain disorders pose a unique set of challenges. Their rarity often means that few clinicians have firsthand experience diagnosing or treating them, leading to delays in recognition and misdiagnosis. Moreover, individuals affected by rare brain conditions frequently endure long diagnostic journeys involving multiple specialists, invasive tests, and uncertain outcomes. These disorders may not appear in standard medical texts or routine differential diagnoses, complicating their identification.
Examples of rare brain disorders include conditions such as Moyamoya disease, a progressive cerebrovascular disorder characterized by the narrowing of arteries at the base of the brain, and Stiff Person Syndrome, an autoimmune condition leading to severe muscle stiffness and spasms. Others, like Alexander disease or Batten disease, are genetic disorders that typically manifest in childhood and result in severe neurological deterioration. While these conditions are individually rare, collectively, they account for a significant portion of neurological illness burden worldwide. Increased awareness and research funding are vital for improving diagnosis, treatment, and quality of life for affected individuals.
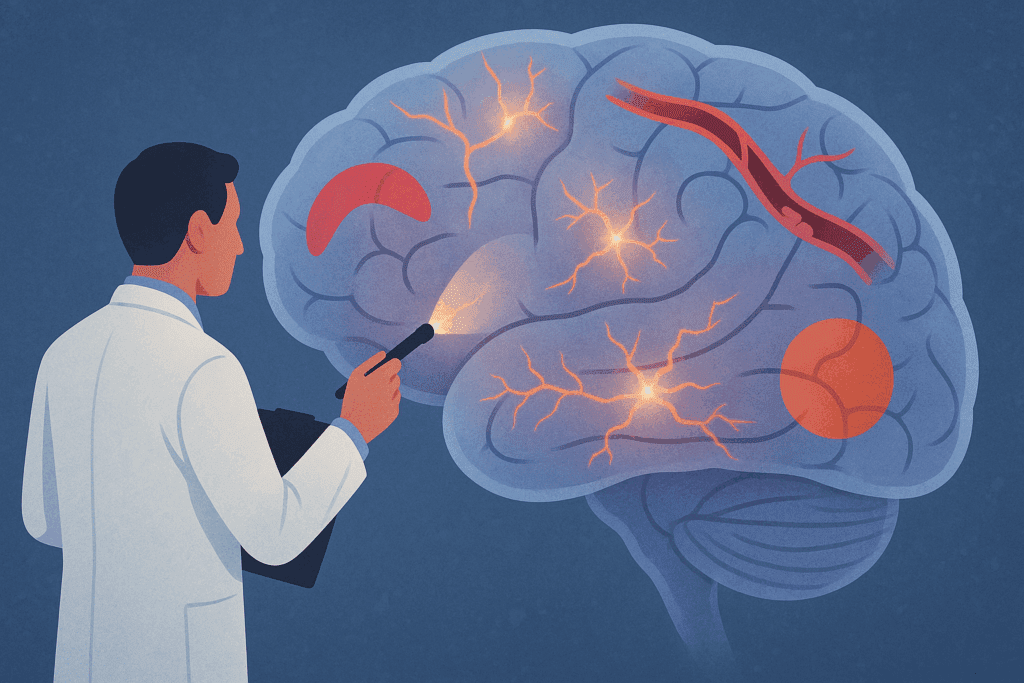
Symptoms and Diagnostic Clues Across the Spectrum
Brain illnesses and symptoms often overlap, making diagnosis a nuanced and evolving process. Regardless of whether a condition is common or rare, certain symptoms should raise clinical suspicion and prompt further investigation. These may include sudden changes in mental status, unrelenting headaches, unexplained seizures, movement disorders, or alterations in personality or behavior. Cognitive decline, visual disturbances, and sensory deficits may also point to underlying brain issues.
Neurologists often rely on a combination of neuroimaging, genetic testing, lumbar puncture, and electrophysiological studies to identify the nature of a disorder of brain function. However, a single test rarely provides definitive answers. Instead, clinicians must interpret a constellation of findings in the context of a patient’s history and presentation. In cases involving rare brain conditions, clinicians may consult specialized databases or collaborate with research institutions to identify less commonly seen patterns.
The Importance of a Comprehensive Brain Diseases List
Compiling an accurate and detailed brain diseases list serves more than just academic interest; it is a foundational tool for clinical care, research, and education. A list of brain diseases and disorders helps clinicians recognize patterns and make connections that might otherwise go unnoticed. It also empowers patients and families by providing terminology they can use to better understand and communicate their condition.
Among the top ten brain diseases regularly included on such lists are Alzheimer’s, Parkinson’s, multiple sclerosis, epilepsy, stroke, Huntington’s disease, brain tumors, meningitis, traumatic brain injury, and migraine. However, comprehensive lists should also include less familiar entries such as anti-NMDA receptor encephalitis, progressive supranuclear palsy, and autoimmune encephalitis. By acknowledging both common and rare entries, we foster a more inclusive understanding of diseases that affect the brain, support more accurate diagnoses, and inspire broader scientific inquiry.
Understanding Brain Syndrome and Related Terms
The term “brain syndrome” has evolved over time but continues to be used in various clinical contexts. Historically, it referred to a collection of symptoms indicating generalized brain dysfunction, such as confusion, agitation, and cognitive decline. Today, it is sometimes used interchangeably with terms like delirium or encephalopathy, although distinctions remain. Brain syndrome symptoms are typically acute and reversible, often arising from infections, metabolic imbalances, or medication side effects.
Nevertheless, brain syndrome can also be used to describe more chronic or progressive conditions. For instance, Korsakoff syndrome, a chronic memory disorder linked to thiamine deficiency, falls under this umbrella. Brain syndrome list entries are diverse, reflecting the multifaceted nature of brain-related diseases. Clarifying these terms helps improve communication among clinicians and ensures appropriate diagnostic and therapeutic approaches are pursued.
Navigating the Spectrum of Brain Problems and Symptoms
Brain problems and symptoms often reflect the underlying complexity of the central nervous system. Symptoms may be focal, affecting a specific part of the body or cognitive domain, or diffuse, impacting multiple systems simultaneously. For example, a brain tumor in the frontal lobe may present with personality changes and executive dysfunction, while a cerebellar stroke may cause coordination and balance problems. The breadth of possible manifestations underscores the importance of a detailed clinical evaluation.
Some brain issues emerge gradually, as in neurodegenerative conditions, while others strike suddenly, as with hemorrhagic stroke or acute encephalitis. Regardless of onset, the presence of neurological red flags—such as seizures, persistent confusion, weakness, or altered consciousness—should prompt immediate medical evaluation. Recognizing early symptoms can lead to timely diagnosis, intervention, and, in some cases, improved outcomes. For rare brain disorders, early detection may also provide eligibility for clinical trials or emerging therapies.
Differentiating Between Rare and Common Brain Diseases
While both rare and common brain diseases can be debilitating, their clinical journeys often differ. Common conditions benefit from established diagnostic criteria, treatment protocols, and public awareness. In contrast, rare brain disorders frequently lack consensus guidelines and may be subject to limited treatment options. This discrepancy can result in delayed diagnoses, emotional distress, and fewer resources for affected individuals and their families.
Nonetheless, efforts to bridge this gap are underway. Advocacy organizations and rare disease registries are working to gather data, educate healthcare providers, and support research. Patients with rare brain conditions often become powerful voices in these efforts, sharing their stories and participating in studies that advance knowledge. As science evolves, the distinction between rare and common may become less rigid, particularly as genetic and molecular tools uncover shared mechanisms across the spectrum of brain related diseases.
The Role of Genetics and Environment in Brain Illness
The etiology of brain illness often lies at the intersection of genetic predisposition and environmental exposure. Some disorders, such as familial Alzheimer’s disease or Huntington’s disease, follow clear Mendelian inheritance patterns. Others may result from complex interactions between multiple genes and external factors, including infections, toxins, and head trauma. Understanding these dynamics can aid in risk assessment, early detection, and targeted intervention.
In the case of rare brain disorders, genetic testing has revolutionized diagnostic capabilities. Techniques such as whole-exome sequencing and genome-wide association studies have identified novel mutations and pathways involved in previously mysterious conditions. Environmental factors, while harder to quantify, remain crucial in understanding diseases that affect the brain. Ongoing research explores how lifestyle, pollution, nutrition, and stress impact neurological health across the lifespan.
When to Seek Medical Attention for Brain Symptoms
Many individuals delay seeking medical care for brain symptoms, attributing them to stress, fatigue, or aging. However, certain signs warrant immediate attention. These include sudden confusion, vision loss, new or severe headaches, speech disturbances, limb weakness, or uncharacteristic behavior changes. Even seemingly benign symptoms may indicate underlying pathology, particularly if they persist or worsen.
Prompt evaluation by a neurologist or primary care provider can lead to early diagnosis and intervention. Diagnostic workups typically involve neuroimaging, blood tests, and neurological examinations tailored to the patient’s presentation. In cases of rare brain conditions, referral to specialty centers or research institutions may be necessary. Early engagement with healthcare services not only improves prognosis but also opens the door to supportive care, therapy, and education for patients and their families.
Toward a Holistic Approach to Brain Medical Conditions
Managing brain medical conditions requires more than pharmacological treatment; it calls for a multidisciplinary and patient-centered approach. This may include physical therapy, occupational therapy, speech therapy, psychological counseling, and social support. For patients with chronic or progressive disorders, palliative care and advanced care planning are essential components of long-term management.
Education plays a critical role in empowering patients and caregivers. Understanding the nature of brain disorders and diseases helps reduce fear and stigma, facilitates informed decision-making, and fosters collaboration between patients and healthcare providers. Community support networks, advocacy groups, and online platforms further enhance access to information and emotional support.
A Forward-Looking Perspective on Brain Health
As our knowledge of brain sickness continues to expand, so too does our capacity to intervene more effectively. Advances in neuroimaging, biomarkers, artificial intelligence, and personalized medicine are transforming how we approach diagnosis and treatment. Rare brain conditions, once considered untreatable curiosities, are now entering the realm of precision medicine.
Furthermore, increased public awareness and policy initiatives focused on neurological health are bringing much-needed attention to diseases that affect the brain. Funding for brain research is growing, and interdisciplinary collaboration is yielding new insights into prevention, early detection, and neurorehabilitation. While challenges remain, the future of brain health is increasingly hopeful.
Frequently Asked Questions (FAQ): Understanding Rare Brain Disorders and Related Brain Conditions
1. What makes diagnosing rare brain disorders so complex compared to more common neurological conditions?
Diagnosing rare brain disorders often involves navigating a maze of overlapping symptoms and limited clinical familiarity. Unlike common brain disorders such as epilepsy or migraine, many rare brain conditions lack standardized diagnostic pathways and are not routinely screened in primary care. This can lead to years of misdiagnoses or delayed recognition. Moreover, rare disorders may require advanced genetic panels, metabolic assessments, or functional neuroimaging that are not readily accessible in all healthcare settings. These challenges emphasize the need for specialized centers and a continually updated list of brain diseases and disorders that includes both well-known and emerging diagnoses.
2. How do brain syndrome and brain illness differ in clinical practice?
While both terms refer to impaired brain function, brain syndrome is typically used to describe transient or reversible conditions, such as delirium from an infection or medication. In contrast, brain illness generally refers to longer-term or chronic neurological deterioration, such as seen in neurodegenerative disorders. The brain syndrome list often includes conditions that can resolve with treatment, while the broader brain illnesses list captures progressive or incurable disorders. Understanding the distinction is essential for determining prognosis and treatment urgency. Clinicians must be cautious not to conflate the two, as doing so could delay appropriate care for either category of disease.
3. Why are neurological illness lists critical for medical education and public health planning?
Comprehensive neurological illness lists serve as essential reference tools for clinicians, researchers, and policymakers. By cataloging both rare brain disorders and common brain diseases, these lists aid in training healthcare professionals to recognize subtle brain condition symptoms. Public health efforts also benefit, as accurate data on disease prevalence and burden allows for better resource allocation. In addition, having an updated brain diseases list fosters more inclusive clinical trials and guides the development of therapeutic guidelines. Importantly, such lists also provide validation for patients, helping them understand that their brain problems are recognized and studied, even if uncommon.
4. What role do patient advocacy groups play in addressing rare brain conditions?
Advocacy organizations are often lifelines for individuals with rare brain disorders. These groups provide education, funding for research, and platforms for sharing lived experiences. Because many rare brain conditions are underrepresented in scientific literature, patient-led groups help drive awareness and accelerate the inclusion of these disorders in clinical research. They also collaborate with neurologists to refine classifications within the brain diseases list and influence policy decisions at national and international levels. Through support networks and public campaigns, these organizations humanize complex brain medical conditions and ensure that affected individuals do not face their diagnoses in isolation.
5. How do cultural attitudes impact the perception and treatment of brain-related diseases?
Cultural interpretations of brain illness can influence everything from symptom reporting to willingness to seek care. In some communities, brain disorders and diseases may be stigmatized or associated with supernatural beliefs, which can prevent early intervention. Others may prioritize physical symptoms over cognitive or emotional ones, delaying diagnosis of brain ailments that present subtly. Understanding brain problems and symptoms within a cultural context allows providers to offer more empathetic and effective care. Educational outreach and culturally tailored communication are essential for bridging gaps in understanding and reducing the global burden of diseases that affect the brain.
6. Are there preventive strategies for rare brain conditions, or are they entirely genetic and unmodifiable?
While many rare brain disorders have a genetic origin, emerging research suggests that certain environmental or lifestyle modifications may influence disease progression or symptom severity. For instance, in metabolic or mitochondrial brain diseases, early dietary interventions and avoidance of specific toxins may delay neurological decline. Epigenetic studies are also uncovering how environmental exposures can activate or silence genes associated with brain issues. Although prevention may not be feasible for all rare conditions, early detection through genetic counseling and newborn screening is a powerful tool. Ongoing trials are exploring gene therapies and enzyme replacement for some rare entries in the brain diseases list.
7. How do brain problems affect caregivers and family members of those diagnosed?
Caring for someone with a brain illness can be emotionally, physically, and financially draining. Many brain disorders and diseases require long-term supervision, complex medication regimens, and assistance with daily tasks. Caregivers often experience secondary trauma, anxiety, and social isolation. Brain condition symptoms such as behavioral changes, aggression, or memory loss can strain relationships and create additional emotional burdens. Recognizing caregivers as part of the therapeutic team and offering them psychological and social support is crucial to maintaining both patient and caregiver well-being across the spectrum of brain medical conditions.
8. How is technology advancing the diagnosis and management of brain ailments?
Artificial intelligence and machine learning are revolutionizing the identification of subtle patterns within neurological data, allowing earlier and more accurate diagnoses of both rare and common brain diseases. Wearable devices can now track brain activity in real time, helping monitor seizures, tremors, or cognitive fluctuations. Digital platforms are also improving access to rare brain conditions databases, enabling real-time collaboration between global experts. Furthermore, personalized medicine—driven by big data—is tailoring treatments based on individual genetic, environmental, and biomarker profiles. These innovations are transforming the clinical landscape, offering renewed hope for those affected by brain-related diseases.
9. Can early-life brain injuries mimic symptoms of progressive brain disorders later in life?
Yes, early head trauma or untreated neurological insults in childhood can sometimes produce symptoms resembling degenerative brain conditions in adulthood. This overlap can complicate diagnosis, especially when brain problems and symptoms include cognitive decline or motor deficits. For example, post-traumatic epilepsy or delayed-onset neuroinflammation may be misattributed to Alzheimer’s or other top ten brain diseases. Differentiating between sequelae of childhood brain injuries and progressive disorders requires detailed history-taking, advanced imaging, and longitudinal observation. Including such cases in the broader brain illnesses list enhances our understanding of how diverse injuries can converge into similar symptom profiles.
10. What are the implications of misclassifying a brain disorder as psychiatric rather than neurological?
Mislabeling a brain condition as purely psychiatric can delay appropriate treatment and cause unnecessary stigma. Certain rare brain disorders, such as autoimmune encephalitis or Wilson’s disease, often begin with psychiatric-like symptoms such as hallucinations, anxiety, or mood swings. Without proper recognition of the underlying disorder of brain function, patients may be misdiagnosed with schizophrenia or bipolar disorder. This highlights the critical need for interdisciplinary evaluations and awareness of atypical presentations within the list of brain diseases and disorders. Accurate classification ensures timely access to treatments that can reverse or halt disease progression—outcomes that are rarely possible in untreated cases.
Conclusion: Recognizing the Urgency and Complexity of Brain Disorders and Diseases
In the intricate landscape of neurological illness, rare brain disorders and common brain diseases alike demand our attention, empathy, and action. The symptoms they produce are more than clinical curiosities; they are lived experiences that shape the identities and realities of millions of individuals around the world. From the subtleties of a gradually worsening memory to the sudden onset of seizures or paralysis, brain condition symptoms serve as signals of deeper dysfunction that merit careful evaluation and thoughtful response.
By understanding the full spectrum of brain problems and symptoms—including both rare brain conditions and widely known ailments—we equip ourselves to respond more effectively as healthcare providers, caregivers, and informed individuals. A robust neurological illness list not only aids in diagnosis but also in research and advocacy. We must continue to build bridges between clinical practice, scientific discovery, and compassionate care, recognizing that diseases associated with the brain are as diverse as they are impactful.
Ultimately, our collective responsibility lies in supporting individuals facing these brain medical conditions and in promoting research, awareness, and equitable access to care. The journey through brain disorders and diseases may be complex, but with knowledge, support, and innovation, it need not be one of despair. Instead, it can be one of resilience, discovery, and hope.


