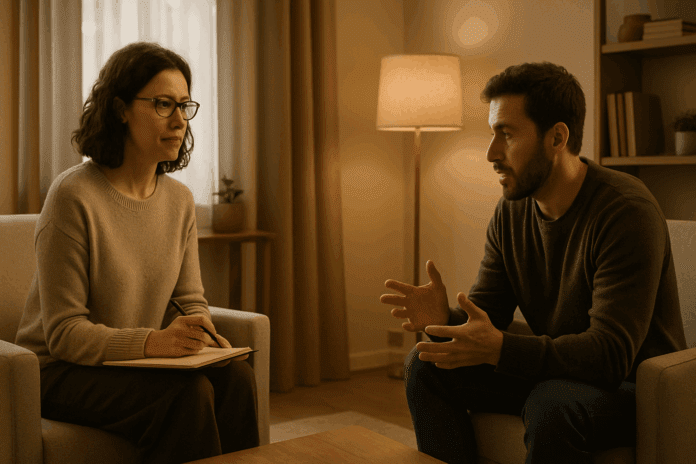
In today’s rapidly evolving mental health landscape, there is increasing public awareness about the importance of effective treatment options for psychological well-being. Yet, many individuals remain uncertain about how different therapeutic approaches compare, particularly when it comes to understanding psychotherapy and behavioral therapy. These two core modalities are often discussed interchangeably, but they diverge in methodology, goals, and application. A closer examination reveals meaningful distinctions, shared philosophies, and important considerations for choosing the most effective treatment based on individual needs and psychological profiles. As mental health care becomes more personalized and evidence-based, distinguishing between these therapeutic paradigms is vital for informed decision-making.
You may also like: How Does CBT Work to Improve Relationships and Communication? Science-Backed Techniques for Getting Along with Others
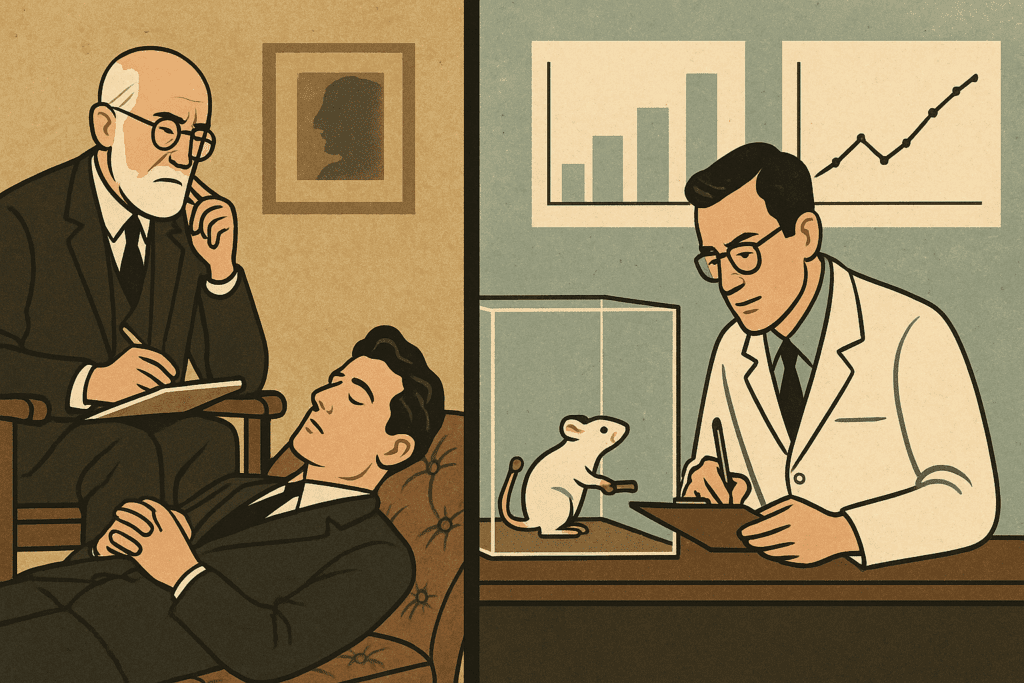
Psychotherapy and behavioral therapy each have unique histories that shaped their current clinical applications. Psychotherapy, in its broadest sense, encompasses a range of approaches grounded in the therapeutic relationship between patient and clinician. Traditionally, it includes talk therapy modalities such as psychodynamic therapy, humanistic therapy, and existential therapy, all of which emphasize insight, self-reflection, and emotional exploration. On the other hand, behavioral therapy emerged from the principles of learning theory in the early 20th century. It is rooted in the belief that behavior is learned and can therefore be unlearned or modified. Rather than focusing on unconscious drives or early developmental experiences, behavioral therapy addresses observable actions and measurable outcomes.
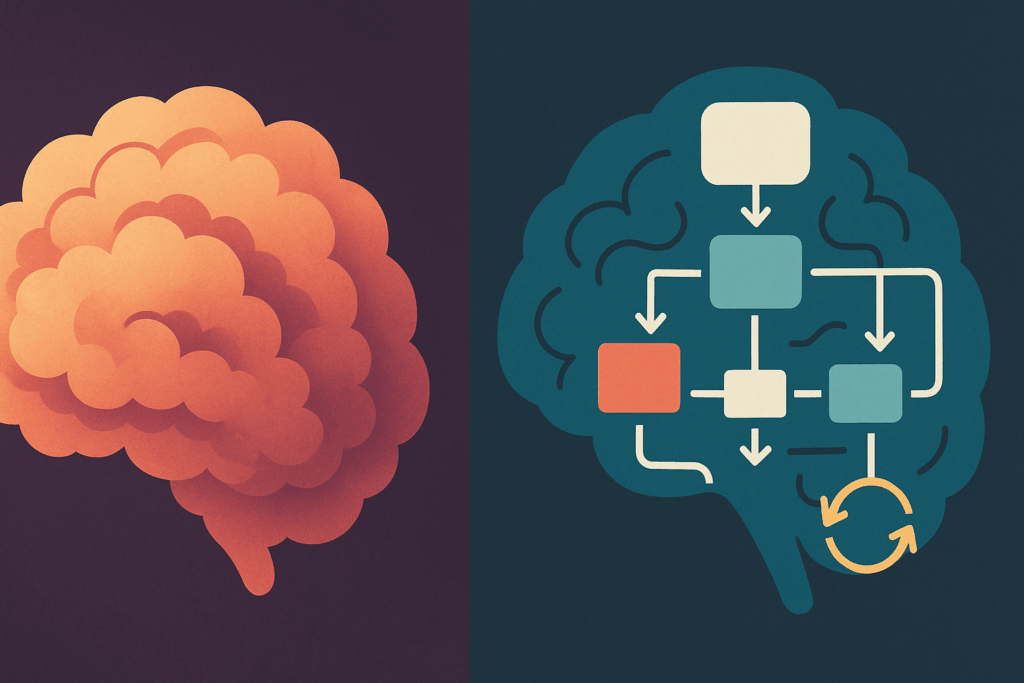
To understand how psychotherapy and behavioral therapy compare, it is essential to recognize that they are not always mutually exclusive. Many contemporary approaches blend elements from both traditions. Cognitive Behavioral Therapy (CBT), for instance, is one of the most researched and widely applied models in clinical practice. It integrates behavioral techniques with cognitive restructuring to treat a wide array of conditions including depression, anxiety, PTSD, and obsessive-compulsive disorder. This synthesis reflects the evolution of mental health care toward more integrative and client-centered frameworks. Yet, even within CBT, practitioners must often navigate the nuanced debate of cognitive behavioral therapy vs psychotherapy, especially when tailoring interventions for complex or treatment-resistant cases.
One of the clearest distinctions lies in the theoretical underpinnings of each approach. Psychotherapy, particularly in its classical psychodynamic or humanistic forms, operates on the premise that internal conflicts, unresolved past experiences, and core emotional wounds shape present-day functioning. Therapeutic progress is seen as unfolding over time through deepening awareness, emotional processing, and the therapeutic alliance itself. In contrast, behavioral therapy tends to be more structured, goal-oriented, and time-limited. Its success is often measured by observable behavioral change, with less emphasis on unconscious motivation or relational dynamics. This difference in orientation can be crucial when selecting a therapy model, especially for clients who prefer a solution-focused approach versus those who seek to understand the deeper roots of their emotional difficulties.
Another defining feature of behavioral therapy is its reliance on empirically supported techniques derived from principles such as classical conditioning, operant conditioning, and social learning theory. Interventions like exposure therapy for phobias, systematic desensitization for anxiety, and behavior modification plans for children with ADHD are all grounded in this framework. These techniques have been lauded for their efficiency and practical application. One of the key advantages of behavioral therapy is its focus on skill acquisition and measurable improvement. Clients are taught specific tools to cope with distressing situations, regulate emotions, and build adaptive habits. For many, this structured approach provides a sense of mastery and empowerment early in the treatment process.
Psychotherapy, by contrast, often involves a slower, more exploratory path. It may be less structured but offers depth and richness in addressing core issues that behavioral methods alone may overlook. For example, psychodynamic therapy explores how early attachment experiences influence adult relationships, while humanistic therapy focuses on self-actualization and authentic living. In some cases, psychotherapy serves as a vital space for grief, trauma integration, or existential questioning—issues that may not respond as effectively to behavior-focused strategies. This deeper introspective work can be particularly beneficial for clients who struggle with identity, long-standing relational patterns, or unresolved emotional pain.
When comparing psychotherapy vs CBT, it is important to note that CBT, though structured, also promotes cognitive insight. Unlike pure behavioral therapy, CBT emphasizes the role of distorted thinking in emotional distress. By identifying and challenging cognitive distortions such as catastrophizing, black-and-white thinking, or overgeneralization, clients can learn to reframe their thoughts and thereby alter their emotional responses and behaviors. This dual focus on cognition and behavior places CBT at the intersection of the psychotherapy and behavioral therapy spectrum. It is both directive and reflective, offering an evidence-based path for clients who need both practical tools and psychological insight.
Cognitive behavioral therapy vs psychotherapy debates often surface when clinicians must choose between depth-oriented versus skills-based treatment. For example, a client with a history of trauma might benefit from psychodynamic work to process unresolved emotional wounds, whereas another individual with social anxiety might respond better to CBT’s exposure techniques and cognitive restructuring. However, many therapists draw from both traditions, recognizing that psychological healing is not one-size-fits-all. The clinician’s training, the client’s goals, and the nature of the presenting issue all influence the treatment trajectory. This integrated mindset reflects a broader shift in the field toward therapeutic pluralism, which values flexibility, personalization, and outcome-driven care.
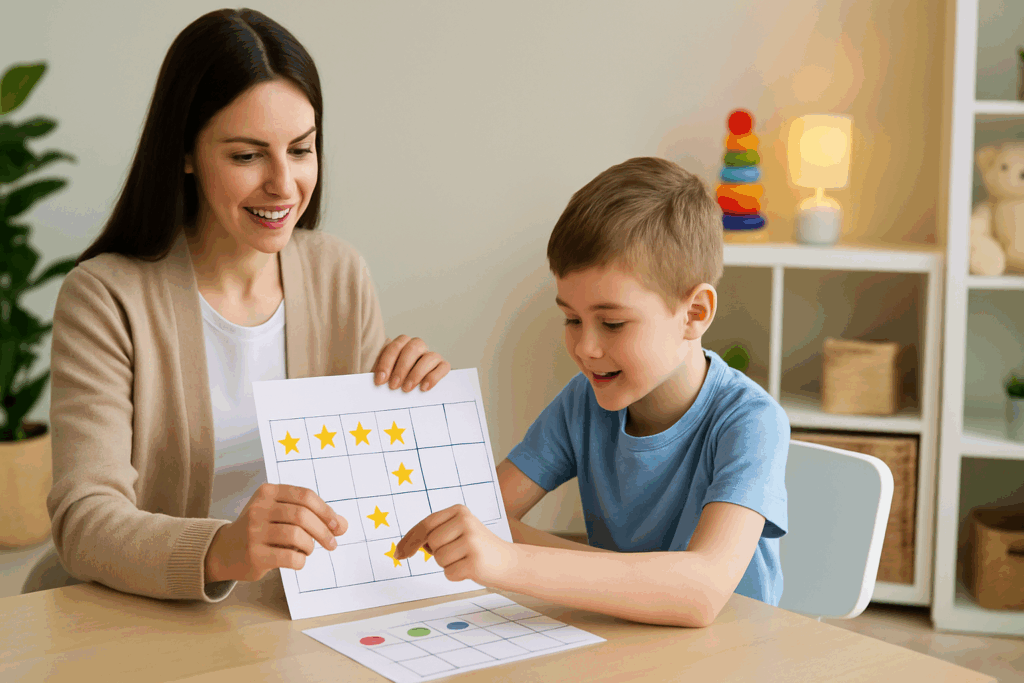
The advantages of behavioral therapy become particularly evident in certain clinical populations. For children and adolescents with behavioral disorders, for instance, structured interventions such as token economies or parent training programs can yield significant improvements in functioning. Similarly, individuals with specific phobias or compulsions often experience rapid relief from exposure-based treatments. Behavioral therapy also aligns well with managed care models and brief therapy formats, which prioritize cost-effectiveness and outcome measurement. In these contexts, the concrete nature of behavioral goals—such as reducing panic attacks, increasing social engagement, or improving sleep hygiene—makes this modality especially appealing.
Nonetheless, behavioral therapy is not without limitations. Critics argue that its focus on surface-level behavior change may neglect deeper emotional or relational factors that contribute to psychological distress. While clients may learn to suppress symptoms, they may not resolve the underlying causes. For some, this can lead to symptom substitution or relapse once external reinforcement is removed. In contrast, psychotherapy often seeks to transform the client’s internal world, fostering lasting change through insight and emotional healing. This contrast underscores the importance of thoughtful assessment and individualized treatment planning.
The current trend in mental health care favors integrative models that draw from both traditions. Many clinicians practice from an eclectic or integrative orientation, combining techniques based on the client’s needs rather than rigidly adhering to one school of thought. For instance, a therapist might use exposure therapy to address a client’s panic symptoms while also employing psychodynamic strategies to explore how early attachment trauma contributes to chronic anxiety. This holistic approach ensures that treatment addresses both symptom relief and deeper emotional growth.
Another vital consideration in choosing between psychotherapy and behavioral therapy is the client’s personal preferences, values, and readiness for change. Some clients are drawn to the structure and predictability of behavioral techniques, especially when facing acute crises or functional impairments. Others may seek a more open-ended and exploratory process to make sense of long-standing emotional challenges. Understanding these preferences allows therapists to collaborate with clients in co-constructing a treatment plan that feels both effective and meaningful.
The setting in which therapy occurs can also shape the choice of modality. In primary care settings or community mental health clinics, brief behavioral interventions may be favored due to time constraints and the need for quick results. In contrast, private practice settings may afford the luxury of longer-term psychotherapy. Additionally, access to care, cultural considerations, and insurance coverage often play a role in determining which approaches are feasible and sustainable. These real-world factors highlight the complexity of mental health care delivery and the need for flexibility and advocacy within the system.

Technological advances have further expanded the landscape of therapy delivery, particularly through digital mental health platforms. Online CBT programs and mobile apps offering behavioral interventions are increasingly available and have shown efficacy for conditions such as depression, anxiety, and insomnia. These innovations align well with the principles of behavioral therapy, which lend themselves to structured, self-guided formats. However, they may lack the relational depth and nuanced exploration that characterize traditional psychotherapy. This digital divide raises important questions about the role of human connection in healing and the need to balance technological convenience with therapeutic presence.
Ultimately, the decision between psychotherapy and behavioral therapy is not about choosing a superior model but rather about aligning treatment with the unique needs, goals, and circumstances of each individual. Both modalities offer valuable tools for healing, growth, and psychological well-being. When used thoughtfully, they can complement each other and contribute to a comprehensive and compassionate approach to mental health care. The most effective therapy is one that resonates with the client, is grounded in clinical evidence, and is delivered by a skilled, attuned practitioner.
Frequently Asked Questions: Psychotherapy and Behavioral Therapy
What are some lesser-known benefits of integrating psychotherapy and behavioral therapy in treatment plans?
An emerging benefit of combining psychotherapy and behavioral therapy is the enhancement of emotional regulation through real-time behavioral experimentation. For instance, a client might explore childhood attachment wounds in a psychodynamic session and then practice assertive communication through behavioral role-play. This synthesis allows for deeper insight to translate into real-life changes more efficiently. Moreover, integration can reduce dropout rates, as patients are more likely to stay engaged when therapy feels both emotionally meaningful and practically useful. While each modality can stand alone, their synergy often supports more comprehensive and sustainable outcomes.
How do therapists determine whether a client is better suited for psychotherapy vs CBT?
Therapists often assess several factors when deciding between psychotherapy vs CBT, including symptom duration, severity, personality structure, and cognitive readiness. Clients experiencing intense emotional dysregulation or identity confusion may benefit from the introspective nature of psychotherapy. In contrast, those seeking symptom relief for anxiety or panic disorders might respond better to CBT’s structured framework. The distinction becomes especially important in cases where time or insurance constraints necessitate shorter treatment durations. Ultimately, informed clinical judgment paired with client preference guides this decision.
Can cultural or generational differences influence the effectiveness of psychotherapy and behavioral therapy?
Absolutely. Cultural norms around emotional expression, authority figures, and behavioral expectations can significantly impact how a client engages with either psychotherapy or behavioral therapy. For example, younger generations often favor CBT because of its transparency, goal orientation, and reliance on measurable progress. In contrast, clients from cultures that emphasize interpersonal harmony may resonate more with psychotherapy’s relational depth and exploration of unspoken dynamics. Tailoring the modality to align with cultural and generational values can significantly enhance therapeutic efficacy.
What innovations are shaping the future of cognitive behavioral therapy vs psychotherapy?
Digital platforms, AI-assisted interventions, and virtual reality exposure tools are transforming cognitive behavioral therapy vs psychotherapy debates. CBT has been especially adaptive to these innovations, with numerous self-guided apps offering modules on cognitive restructuring and behavior tracking. Meanwhile, developments in teletherapy and AI-driven mood analysis are beginning to influence psychotherapy, allowing therapists to detect subtle emotional shifts through language patterns. These tools offer therapists real-time data to inform treatment without replacing the nuance of human connection. As technology evolves, it may help bridge the gap between data-driven CBT and the reflective depth of psychotherapy.
How do the advantages of behavioral therapy apply to children and adolescents differently than to adults?
The advantages of behavioral therapy are particularly pronounced in pediatric populations, where developmental stages favor concrete feedback, repetition, and clear reinforcement systems. Token economies, behavior charts, and parent-led interventions provide external structure, which aligns with how children learn best. Adolescents, especially those with ADHD or conduct issues, often benefit from structured problem-solving strategies embedded in behavioral therapy. Unlike adults, who may have more ingrained behavioral patterns, youth are still forming their core habits—making early intervention highly impactful. Integrating behavioral therapy into school systems and family routines further extends its reach and effectiveness.
What role does therapeutic alliance play in psychotherapy and behavioral therapy outcomes?
While therapeutic alliance is a cornerstone of psychotherapy, it also plays a vital but often underestimated role in behavioral therapy outcomes. Research increasingly supports that even in skill-based interventions, the clinician-client relationship enhances motivation, compliance, and long-term results. In psychotherapy, the alliance facilitates emotional safety and narrative development. In behavioral therapy, it fosters trust necessary for clients to engage in uncomfortable tasks like exposure or habit reversal. Thus, regardless of modality, a strong therapeutic bond amplifies treatment gains and promotes resilience.
How do you evaluate long-term effectiveness when comparing psychotherapy vs CBT?
Evaluating long-term outcomes in psychotherapy vs CBT involves looking beyond symptom reduction to broader life functioning and personal growth. CBT often yields faster gains in targeted symptoms, especially for anxiety and depression. However, psychotherapy may result in deeper personality changes and improved relational health over extended timelines. Measures of success include not only decreased distress but enhanced life satisfaction, vocational functioning, and relationship quality. Longitudinal studies suggest that psychotherapy may produce slower but more enduring internal shifts compared to CBT’s rapid symptom relief.
Are there situations where the advantages of behavioral therapy may be outweighed by its limitations?
Yes, particularly in cases where the underlying cause of a behavior is emotionally rooted or trauma-based, the advantages of behavioral therapy may be less pronounced. If a client is using avoidance behaviors to manage unresolved grief or abuse, behavioral modification alone might address the symptom without healing the source. In such contexts, psychotherapy provides a space to unpack and process deeper emotional layers. Additionally, clients who value introspection or struggle with emotional expression may find behaviorally focused interventions too superficial or mechanistic. These cases underscore the importance of nuanced assessment.
What ethical considerations arise when using cognitive behavioral therapy vs psychotherapy across different populations?
Ethical considerations include cultural sensitivity, informed consent, and therapist competence in delivering the chosen modality. Cognitive behavioral therapy vs psychotherapy raises questions about accessibility and equity—for example, CBT’s standardized format may benefit underserved communities through digital tools, while psychotherapy often requires extended time and financial resources. There are also concerns about pathologizing behaviors that may be culturally normative. Ensuring that the chosen approach respects the client’s background, values, and autonomy is key to ethical, person-centered care. Therapists must also be transparent about the benefits and limitations of each method.
How do practitioners remain flexible while maintaining fidelity to psychotherapy and behavioral therapy techniques?
Practitioners often use treatment manuals as a foundation while adapting their style to the client’s feedback and needs. In psychotherapy and behavioral therapy alike, flexibility involves tailoring interventions without compromising core principles. For instance, a CBT therapist might adjust homework assignments to reflect a client’s cultural values, while a psychotherapist might use narrative techniques within a structured goal-setting context. Supervision, ongoing training, and outcome monitoring help ensure that clinical integrity is upheld. The key is to prioritize client outcomes over rigid adherence to theoretical models.
In conclusion, a nuanced understanding of psychotherapy and behavioral therapy empowers both clinicians and clients to make informed decisions about mental health treatment. While psychotherapy offers deep insight into emotional patterns and relational dynamics, behavioral therapy provides practical tools for change and measurable progress. The intersection of these approaches is exemplified in cognitive behavioral therapy, which bridges the gap between reflection and action. As the field continues to evolve, integrative care that honors both traditions will likely become the standard. By appreciating the strengths and limitations of each modality, we can ensure that mental health care remains responsive, effective, and deeply human.
Further Reading:
Psychotherapy vs. CBT: What’s the Difference?