In the constantly evolving landscape of medical research, few topics generate as much anticipation and emotional resonance as the search for an effective Alzheimer treatment. Over the past several decades, scientists, clinicians, patients, and families have been locked in a relentless pursuit of answers to this devastating neurodegenerative condition. Now, with the emergence of Leqembi (lecanemab), a new drug for dementia, hope has been rekindled. Marketed as a possible new cure for dementia by some, Leqembi has sparked fervent discussion in both clinical circles and the general public. Yet, this potential breakthrough is accompanied by critical questions regarding its efficacy, safety, and broader implications for dementia care.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding Leqembi: The New Alzheimer Drug Generating Buzz
Leqembi, known generically as lecanemab, is part of a growing class of monoclonal antibody therapies designed to target amyloid beta, a protein that accumulates abnormally in the brains of individuals with Alzheimer’s disease. This build-up of beta-amyloid plaques is believed to contribute significantly to cognitive decline, memory loss, and neurodegeneration. The goal of this alzheimer new therapy is to reduce these plaques and potentially slow disease progression, rather than merely alleviating symptoms.
Approved by the U.S. Food and Drug Administration (FDA) under the Accelerated Approval pathway and later receiving full traditional approval, the Leqembi drug has become a central point of focus in discussions around the latest treatment for dementia. For the first time, a therapy demonstrated a modest but measurable effect in slowing cognitive decline in early-stage Alzheimer’s patients. While not a miracle cure for dementia, this achievement has been hailed as a signpost on the path toward more effective, disease-modifying treatments.
This new dementia treatment, developed collaboratively by Eisai and Biogen, is administered intravenously every two weeks and is most effective when initiated early in the disease course. Such timing is crucial, as it aligns with the growing emphasis on early detection and intervention in Alzheimer’s care. Yet, it also presents a challenge: identifying patients in the earliest stages of disease, often before major cognitive deficits are apparent.
The Science Behind the Dementia Breakthrough
Lecanemab’s mechanism of action lies in its selective binding to soluble amyloid-beta protofibrils, which are thought to be particularly neurotoxic. By binding to these forms of amyloid, the new medicine for dementia facilitates their removal from the brain, theoretically preserving neural function and slowing neurodegeneration. In phase 3 clinical trials, participants receiving lecanemab exhibited a 27% slower rate of decline in cognitive scores over 18 months compared to those on placebo.
This slowing of cognitive impairment represents a meaningful, though not transformative, shift in the disease trajectory. In real-world terms, patients on Leqembi may retain the ability to perform daily activities and engage socially for longer periods than those not receiving the treatment. While this doesn’t constitute a definitive dementia cure breakthrough, it offers a clinically significant improvement that could change the landscape of dementia care.
These findings have reinforced the role of anti-amyloid therapies in the ongoing development of new dementia medication options. As researchers continue to refine their understanding of Alzheimer’s pathology, therapies like Leqembi may serve as the foundation for combination treatments that also target tau proteins, inflammation, and other neurodegenerative processes.
Potential Risks and Lecanemab Side Effects
Despite its promise, the Leqembi drug is not without controversy. One of the most pressing concerns surrounding this alzheimer treatment is the emergence of adverse events, particularly brain swelling and microhemorrhages. These conditions, known respectively as ARIA-E (amyloid-related imaging abnormalities with edema) and ARIA-H (with hemorrhage), have been reported in a notable percentage of patients receiving the drug.
The lecanemab side effects documented in clinical trials and post-market surveillance suggest that these complications are more common in individuals with certain genetic profiles, particularly carriers of the APOE4 gene variant. This risk has prompted calls for genetic screening prior to initiating therapy, though such measures add complexity and cost to what is already an intensive treatment regimen. In addition to ARIA events, patients may experience headaches, dizziness, and infusion-related reactions, all of which require careful clinical monitoring.
The possibility of severe adverse outcomes has led some to question whether the benefits of this new alzheimer drug justify the risks, particularly in populations with limited access to advanced diagnostic tools or the capacity to manage side effects. These concerns underscore the necessity of patient-centered decision-making and rigorous risk-benefit assessments. As the medical community gains more experience with this therapy, clearer guidelines and patient selection criteria will likely evolve.
Public Reception and Ethical Considerations of the Alzheimer Breakthrough
The approval of Leqembi as a new treatment for Alzheimer was met with a mixture of optimism, skepticism, and ethical debate. For patients and families devastated by the progressive loss of memory and identity, the announcement of a dementia breakthrough felt like a long-awaited victory. For clinicians and scientists, it marked a milestone that validated decades of research into amyloid theory. Yet, the enthusiasm has been tempered by questions surrounding access, affordability, and medical equity.
Leqembi’s price tag, currently estimated at $26,500 annually, places it out of reach for many without comprehensive insurance coverage. Medicare has agreed to cover the therapy under certain conditions, but requirements for documentation, diagnostic confirmation, and ongoing monitoring may exclude vulnerable populations, including those in rural or underserved areas. This raises fundamental questions about who benefits from medical innovation and how the healthcare system can ensure equitable access to new meds for dementia.
Moreover, the framing of this drug as a “miracle cure for dementia” in some media outlets has sparked concern among medical ethicists. While hopeful language may inspire patients, it can also create unrealistic expectations and pressure to pursue aggressive interventions regardless of individual circumstances. A nuanced understanding of what this alzheimer breakthrough offers—and what it does not—is essential to promoting informed consent and responsible care.

Real-World Implementation: Challenges and Opportunities
Transitioning from clinical trials to real-world clinical practice introduces a host of logistical and systemic challenges. The new dementia medication requires regular infusions, advanced imaging to monitor for ARIA events, and multidisciplinary care teams capable of responding to adverse reactions. Implementing such infrastructure widely across diverse healthcare settings will be no small feat.
Healthcare systems must invest in training, diagnostics, and patient education to ensure safe and effective use of this therapy. In particular, neurologists, radiologists, primary care providers, and nursing staff must collaborate closely to manage treatment protocols. Furthermore, patient adherence and understanding are vital, as the therapeutic window for the Leqembi drug hinges on consistent administration and proactive management of potential complications.
Despite these hurdles, the broader adoption of Leqembi presents an opportunity to elevate the standard of dementia care. By integrating the latest treatment for dementia into existing care frameworks, clinicians can offer patients a more comprehensive and proactive approach to managing their condition. This evolution will likely influence future drug development, care models, and public awareness campaigns surrounding cognitive health.
How Leqembi Compares to Other New Meds for Dementia
Leqembi is not the only new alzheimer drug on the horizon. Several other agents are under investigation or pending regulatory review, including donanemab and gantenerumab. Each of these therapies targets amyloid or related pathways, but differences in molecular structure, dosing schedules, and side effect profiles create distinctions in their clinical utility.
In head-to-head comparisons, Leqembi has demonstrated a balance of efficacy and tolerability that positions it favorably among new medicine for dementia. Unlike some earlier drugs that failed to show cognitive benefit despite amyloid clearance, lecanemab achieved measurable improvements in clinical outcomes. This reinforces the growing consensus that the timing and specificity of treatment may be as important as the biological target itself.
Still, ongoing research will determine how these therapies are best integrated into treatment algorithms. Combination strategies that address both amyloid and tau, or that include anti-inflammatory and neuroprotective agents, may offer even greater potential. The future of Alzheimer care will likely be defined by a more personalized, multimodal approach, building upon the foundational knowledge gained from current therapies.
Exploring What the Future Holds for Alzheimer New Therapy Development
Leqembi’s emergence as a viable option in the fight against Alzheimer’s disease has reinvigorated the field and sparked renewed interest in therapeutic innovation. For decades, progress in dementia drug development was characterized by frustration, with numerous high-profile trial failures casting doubt on the amyloid hypothesis. Today, the successful implementation of the Leqembi drug represents both vindication and a springboard for future inquiry.
Pharmaceutical companies, academic researchers, and public health institutions are now investing more heavily in new cure for dementia initiatives. This includes exploration of immunotherapies, gene editing techniques, and lifestyle interventions that may complement pharmacological treatments. Additionally, advances in biomarker development are enabling earlier diagnosis and more precise monitoring, critical components for the success of any new alzheimer drug.
Emerging digital tools, such as wearable cognitive assessments and AI-driven imaging analysis, promise to further enhance the ability to track disease progression and therapeutic impact. These innovations may eventually support the widespread implementation of the latest treatment for dementia in a cost-effective and scalable manner. They also offer a glimpse into a future where individualized care pathways replace the one-size-fits-all model that has long defined dementia management.

Patient Perspectives and the Human Side of the Dementia Breakthrough
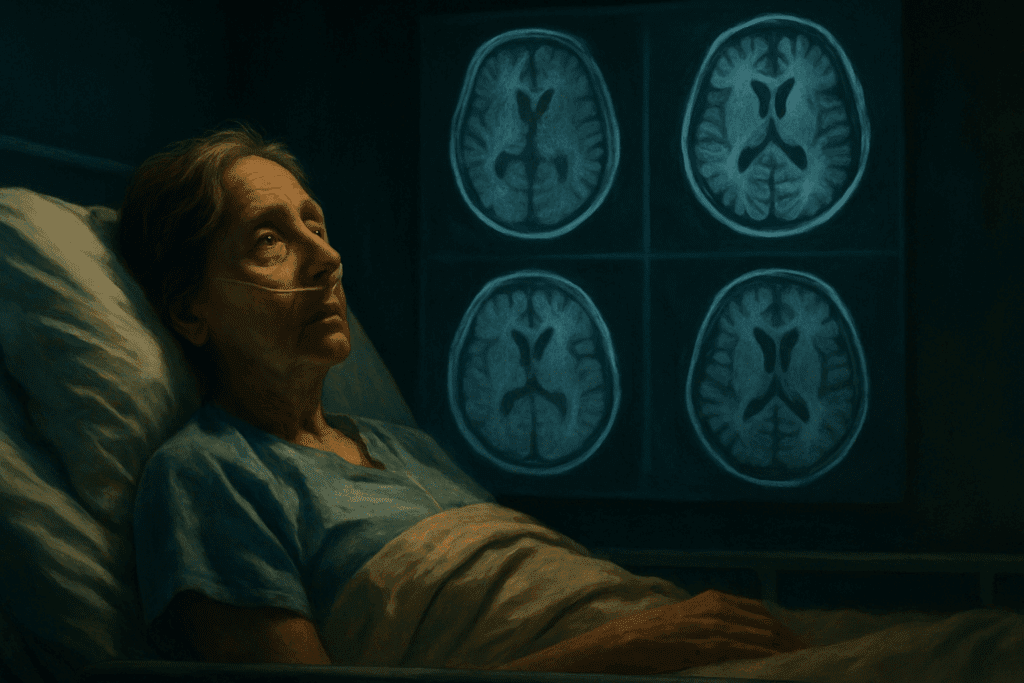
Amidst the science and statistics, it is essential not to lose sight of the human experience at the heart of this discussion. For individuals living with early-stage Alzheimer’s, the availability of a new drug for dementia is more than a clinical development; it is a symbol of hope. Many patients and caregivers have described Leqembi’s approval as a reason to be optimistic about the future, even if cautiously so.
Personal narratives reveal the complexities of navigating new dementia treatment options. Some patients report a renewed sense of agency and purpose, while others express concerns about the demands of biweekly infusions, financial strain, and the possibility of side effects. These lived experiences underscore the need for compassionate, patient-centered care that honors individual preferences and realities.
Support networks, counseling services, and caregiver education will be essential components of a holistic response to this dementia breakthrough. As more individuals consider or begin therapy with the Leqembi drug, healthcare providers must remain attuned to the emotional and psychological dimensions of treatment decisions. Building trust and fostering open communication will be as important as managing biomarkers and infusion schedules.
A New Era in Alzheimer Treatment: Key Takeaways on Leqembi and Beyond
The introduction of Leqembi represents a turning point in the quest for effective Alzheimer treatment. While not a miracle cure for dementia, it marks a significant step forward, offering tangible benefits to patients and reinvigorating the field of neurodegenerative research. As a new alzheimer drug, Leqembi has proven that disease-modifying therapies are possible and can meaningfully alter the trajectory of cognitive decline.
Nevertheless, this progress is tempered by the complexities of real-world implementation, including lecanemab side effects, financial barriers, and the need for advanced diagnostics. Addressing these challenges will require coordinated efforts across the healthcare system, policy landscape, and research community. The promise of the latest treatment for dementia can only be realized if it is accessible, equitable, and responsibly administered.
Looking ahead, Leqembi’s legacy may lie not only in its clinical outcomes but also in its role as a catalyst for continued innovation. It has opened the door for new medicine for dementia, inspired hope among patients, and challenged assumptions about what is possible in Alzheimer care. As we navigate this new frontier, the question is no longer whether we can change the course of dementia—but how far we are willing to go to make that vision a reality.
Frequently Asked Questions: Leqembi and the Future of Alzheimer Treatment
1. How does Leqembi differ from past Alzheimer treatments that have failed to deliver results?
Unlike many earlier therapies that focused solely on symptomatic relief, Leqembi represents a new medicine for dementia that actively targets the underlying pathology of Alzheimer’s disease. This new alzheimer drug was specifically designed to bind to soluble amyloid-beta protofibrils, which are believed to be more neurotoxic than the larger, insoluble plaques targeted by older medications. Leqembi’s clinical trials demonstrated that it could modestly slow cognitive decline, a milestone not previously achieved by most other interventions. Importantly, this therapy is administered in the early stages of the disease, which may explain its greater efficacy compared to previous drugs trialed in later stages. The FDA’s decision to grant full approval to this alzheimer drug approved a pivotal shift in therapeutic philosophy, reinforcing a new era of proactive and targeted interventions.
2. What are some lesser-known lecanemab side effects patients should be aware of?
While most discussions about lecanemab side effects focus on ARIA (amyloid-related imaging abnormalities), emerging data suggest more subtle risks that warrant attention. Some patients have reported sleep disturbances, changes in mood, and sensory perception issues, particularly visual distortions following infusions. Though these events are less common and often temporary, they may impact quality of life and adherence. It’s essential for clinicians to ask patients about these symptoms, as they may not be detected during routine exams. As the new drug for dementia gains wider usage, further post-marketing surveillance will provide critical insights into how these less-visible side effects influence long-term treatment adherence.
3. Could the Leqembi drug be combined with lifestyle changes for improved outcomes?
There is growing interest in whether combining the Leqembi drug with lifestyle modifications might enhance its effectiveness. Cognitive health specialists have long emphasized the role of diet, physical activity, and social engagement in slowing dementia progression. While Leqembi alone offers a pharmacological avenue, its integration with a Mediterranean-style diet, cognitive training, and cardiovascular risk management could amplify outcomes. Preliminary studies are exploring this synergistic model, and early findings suggest that such holistic approaches may improve resilience against disease progression. As a new dementia treatment, Leqembi may best serve patients as part of a multimodal intervention strategy.
4. Why is early diagnosis essential for patients considering this new dementia medication?
Leqembi has demonstrated its greatest benefits when administered at the earliest stages of Alzheimer’s, before major cognitive decline has set in. Because this new cure for dementia works by targeting toxic amyloid accumulations, early detection enables timely intervention before irreversible neural damage occurs. However, most patients are diagnosed well after these changes have become widespread. This lag presents a challenge for broad adoption of the latest treatment for dementia, which relies heavily on biomarker-driven screening tools like PET scans and cerebrospinal fluid analysis. The push toward more accessible and affordable diagnostic technologies will be essential if the full promise of this alzheimer new therapy is to be realized.
5. Is Leqembi accessible to underrepresented communities in dementia care?
Accessibility remains a pressing concern for equitable adoption of this new treatment for Alzheimer. Many underrepresented populations face systemic barriers to early diagnosis, specialist consultations, and insurance coverage. Since the Leqembi drug requires sophisticated diagnostic imaging and continuous monitoring, rural and underserved areas may lack the infrastructure to safely deliver care. Additionally, patients from minority backgrounds are historically underrepresented in clinical trials, raising questions about how this new dementia medication performs across diverse genetic and cultural populations. Bridging this equity gap is essential if we are to realize a truly inclusive dementia breakthrough.
6. How might future Alzheimer drugs build upon the success of this new alzheimer drug?
The success of Leqembi has reinvigorated investment in the development of new meds for dementia, particularly those targeting multiple pathways. While Leqembi focuses on amyloid-beta, future therapies may incorporate tau-protein modulators, anti-inflammatory agents, and even gene-editing technologies. Pharmaceutical companies are exploring combination therapies that synchronize well with Leqembi’s mechanism, offering a layered defense against neurodegeneration. Additionally, personalized medicine approaches, using genomic and biomarker profiling, may enable clinicians to match patients with the most effective treatment regimen. This alzheimer breakthrough sets the stage for a pipeline of smarter, more tailored dementia interventions.
7. What long-term monitoring is required when taking this new dementia treatment?
Patients on Leqembi require ongoing neurological and radiological assessments to track both efficacy and safety. Regular MRI scans are critical for detecting lecanemab side effects like ARIA-E and ARIA-H, which may be asymptomatic initially. Neurocognitive testing is also needed to determine whether the new alzheimer drug is achieving its intended therapeutic milestones. As with any chronic treatment, patient education is vital—individuals must be aware of potential red flags such as sudden headaches, confusion, or changes in gait. The infrastructure required to support this level of monitoring is a key determinant of whether this new drug for dementia will be widely adopted in community-based settings.
8. How do caregivers play a role in the success of this new cure for dementia?
Caregivers are central to the success of any new dementia treatment, especially one as complex as Leqembi. They are often the first to notice subtle cognitive or behavioral shifts that may signal either therapeutic benefits or emerging complications. Beyond administering medications and attending appointments, caregivers provide emotional support that bolsters patient engagement with their treatment regimen. Their insights can guide clinicians in tailoring the therapy over time, especially as the patient’s needs evolve. Empowering caregivers through education and support networks will be critical to sustaining the gains offered by this dementia cure breakthrough.
9. What should patients ask their doctors before starting this alzheimer new therapy?
Patients should initiate thorough discussions about eligibility criteria, including biomarker confirmation and genetic risk factors such as APOE4 status. Questions about infusion logistics, side effect management, and contingency plans for adverse reactions are equally important. Understanding the cost structure—both direct and ancillary—is essential, especially since this latest treatment for dementia requires long-term monitoring. Patients should also inquire about how this therapy integrates with their broader care plan, including non-pharmacologic approaches like nutrition and physical activity. Being proactive with these conversations ensures that individuals approach this new dementia medication with realistic expectations and strong clinical guidance.
10. Is Leqembi the answer to the question: What is the miracle drug for dementia?
While some headlines may tout Leqembi as the miracle cure for dementia, the reality is more nuanced. It is undeniably a groundbreaking step and the first new dementia medication in decades to show measurable clinical benefit. However, calling it a miracle drug oversimplifies both its limitations and the complex nature of Alzheimer’s disease. Leqembi offers hope, but it is not curative—it slows progression but does not reverse existing damage. Still, for many families and clinicians, it represents the most encouraging alzheimer breakthrough in recent memory, and perhaps the beginning of a future where “what is the miracle drug for dementia” has more than one viable answer.
Conclusion: Leqembi and the Evolving Landscape of Dementia Innovation
As the world grapples with the rising prevalence of Alzheimer’s disease, the approval of Leqembi represents more than just a pharmacological advancement—it signals a paradigm shift in how we approach neurodegenerative care. For decades, the notion of a new cure for dementia seemed elusive, clouded by clinical trial failures and limited symptom-based treatments. Today, the Leqembi drug demonstrates that meaningful intervention is possible when science targets the root of the disease and does so early.
Yet, this alzheimer breakthrough is only as powerful as the system that supports its delivery. Equitable access, informed consent, caregiver engagement, and long-term patient monitoring are not supplementary—they are essential. The new dementia medication will only fulfill its potential if the medical community embraces a truly interdisciplinary and inclusive model of care. Moreover, we must remain vigilant about the lecanemab side effects that continue to unfold, ensuring that patients are supported through every stage of their treatment journey.
Ultimately, while Leqembi may not answer the question of what is the miracle drug for dementia in its entirety, it forces us to reconsider the question itself. Perhaps the miracle lies not in a single pill or infusion, but in the convergence of science, compassion, and commitment to continuous discovery. As we enter a new era defined by the latest treatment for dementia, the opportunity is clear: to redefine what hope looks like for millions facing cognitive decline—and to do so with both rigor and humanity.
Further Reading:
Alzheimer’s treatments: What’s on the horizon?