Vascular dementia is a complex and often progressive neurological condition marked by cognitive impairments that result from reduced blood flow to the brain. This condition frequently arises following a stroke or due to chronic issues such as high blood pressure, diabetes, or vascular disease. Unlike Alzheimer’s disease, which is typically linked to the accumulation of amyloid plaques and neurofibrillary tangles, vascular dementia is primarily caused by cerebrovascular events that damage brain tissue over time. This distinction plays a critical role in guiding treatment options, particularly when considering appropriate medication for vascular dementia. Understanding what experts recommend in terms of pharmacological interventions is essential for individuals, caregivers, and healthcare providers navigating this challenging diagnosis.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding the Underlying Mechanisms of Vascular Dementia
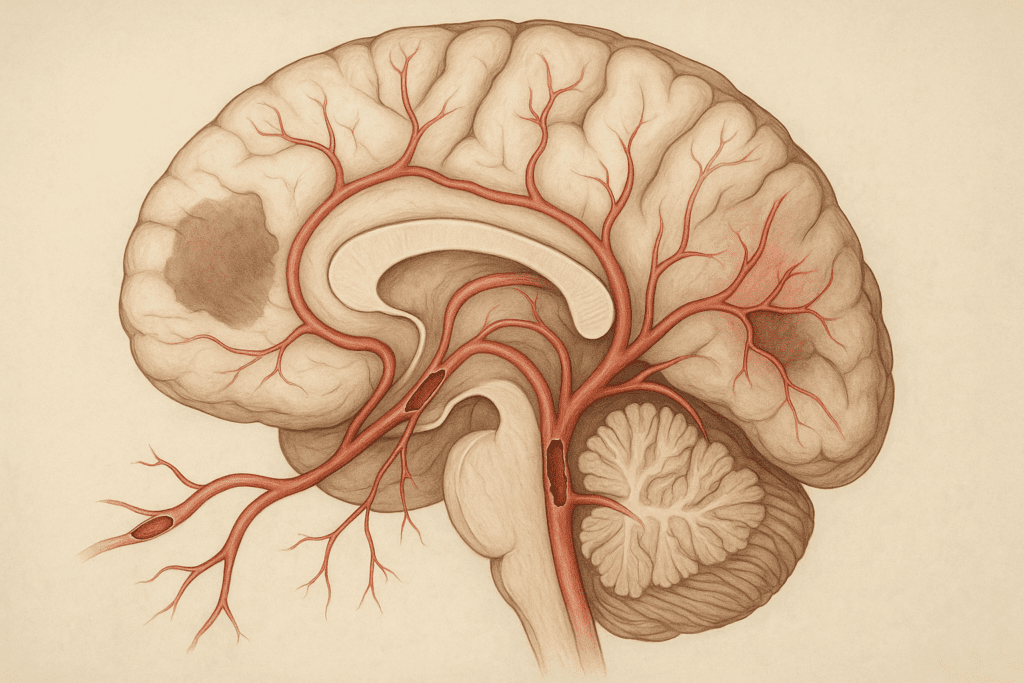
To appreciate the role of medication in vascular dementia management, one must first understand the biological underpinnings of the condition. Vascular dementia occurs when blood vessels that supply the brain become narrowed or blocked, leading to ischemic events and brain cell death. These vascular insults may be sudden, as in the case of a stroke, or more gradual due to chronic conditions like atherosclerosis. The brain regions affected can vary, resulting in a wide range of symptoms such as memory impairment, difficulty concentrating, confusion, and reduced problem-solving skills.
This vascular origin means that, unlike purely neurodegenerative diseases, the progression of vascular dementia may be modifiable if underlying vascular risk factors are aggressively managed. It is precisely this modifiability that underscores the importance of timely and targeted use of medication for vascular dementia. Drugs may not only improve cognitive symptoms but also help mitigate the underlying vascular pathology contributing to the disease.
The Role of Pharmacological Interventions in Cognitive Support
While there is currently no cure for vascular dementia, pharmacological therapies aim to support cognitive function, reduce behavioral symptoms, and slow the rate of decline. Medical professionals often approach treatment with a combination of strategies that target both the vascular and neurological aspects of the disease. In this multifaceted approach, drugs for vascular dementia play a pivotal role.
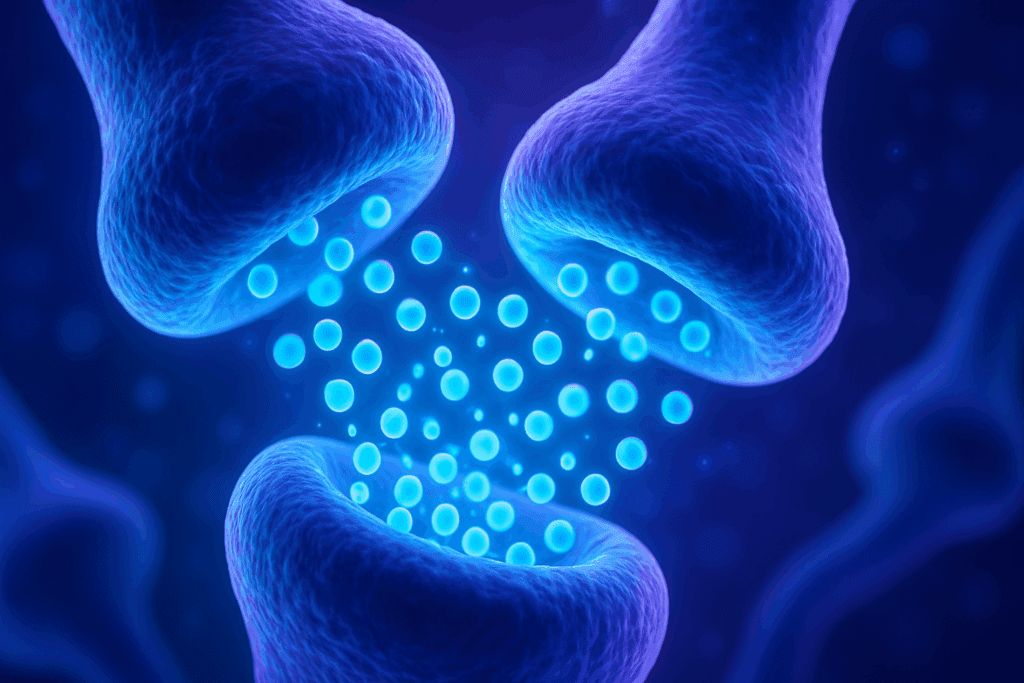
One of the first-line pharmacologic options often considered includes cholinesterase inhibitors, such as donepezil and galantamine. These medications were originally developed for Alzheimer’s disease but have demonstrated modest cognitive benefits in some individuals with vascular dementia. These benefits are thought to stem from improved communication between neurons by increasing levels of acetylcholine, a key neurotransmitter involved in memory and learning.
Memantine, an NMDA receptor antagonist, is another drug commonly prescribed. Though its efficacy in vascular dementia is still under study, it may help moderate symptoms in patients exhibiting mixed dementia (a combination of vascular and Alzheimer’s pathology). Memantine functions by regulating the activity of glutamate, which in excessive amounts can lead to neurotoxicity. Experts often recommend this medication for vascular dementia in cases where cognitive symptoms significantly impair daily living and functionality.
Managing Underlying Vascular Risk Factors With Medication
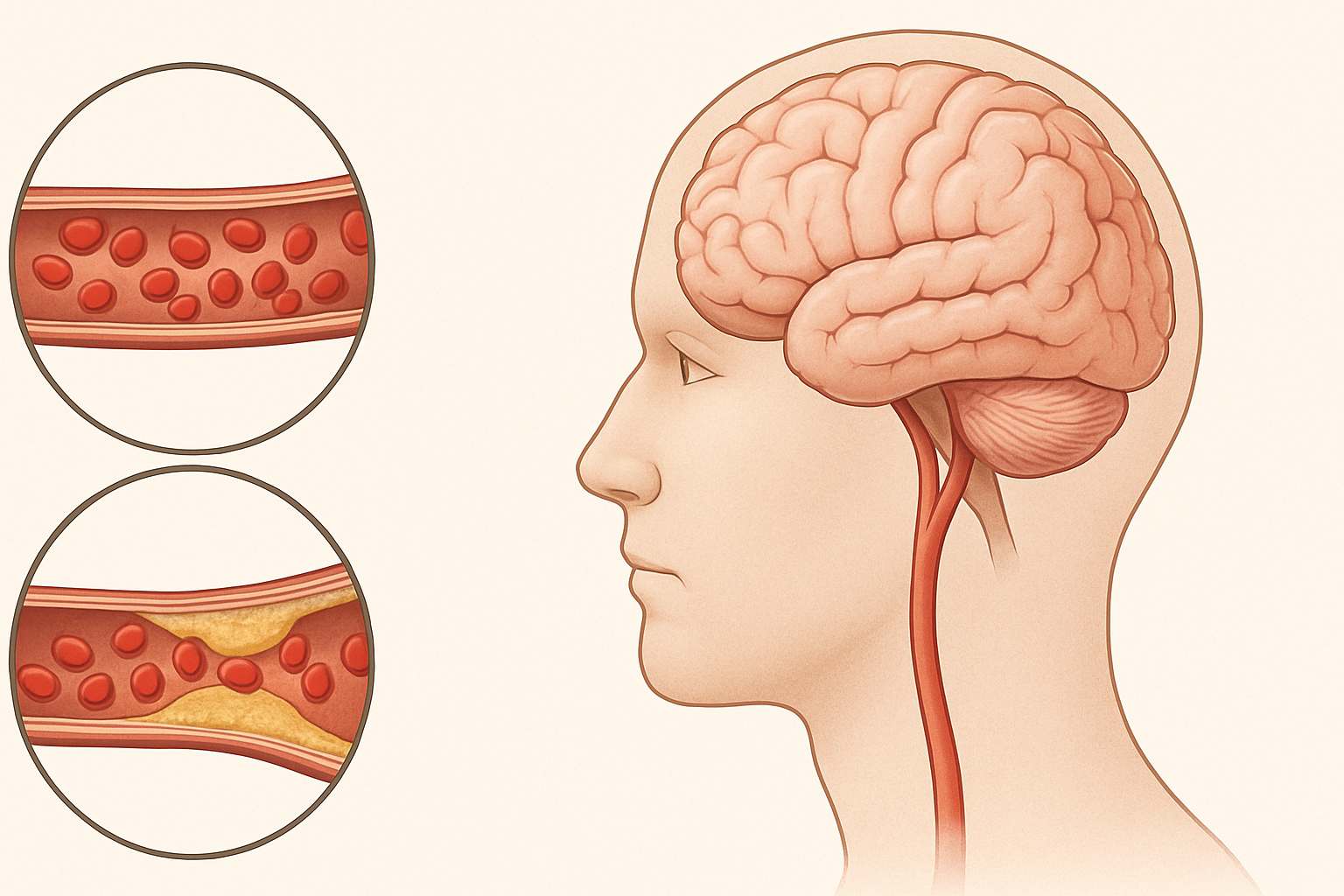
Effectively managing vascular risk factors is essential in slowing the progression of vascular dementia. This often involves prescribing medications that address hypertension, high cholesterol, diabetes, and cardiac conditions. The rationale behind this strategy is straightforward: improving overall cardiovascular health can enhance cerebral blood flow and reduce further vascular insults to the brain.
Antihypertensive drugs such as ACE inhibitors, calcium channel blockers, and beta-blockers are commonly used to manage high blood pressure—a primary contributor to vascular dementia. Controlling blood pressure has been shown to reduce the risk of recurrent strokes and may delay cognitive deterioration. Likewise, statins are frequently prescribed to manage dyslipidemia and lower the risk of atherosclerosis-related events. Although statins are not specifically drugs for vascular dementia, their role in vascular protection makes them a vital component of a comprehensive treatment plan.
In individuals with type 2 diabetes, achieving glycemic control is crucial. Medications such as metformin or SGLT2 inhibitors may be prescribed to reduce blood sugar levels and prevent microvascular damage. Antiplatelet agents like aspirin or clopidogrel may also be used to prevent further cerebrovascular events. These medications do not directly treat cognitive symptoms, but their importance in the context of vascular health and brain function cannot be overstated. For this reason, experts view these vascular-targeting drugs as indirect yet essential tools in the broader pharmacologic arsenal against vascular dementia.

Addressing Behavioral and Psychological Symptoms With Targeted Treatments
Behavioral and psychological symptoms are common in individuals with vascular dementia. These may include depression, agitation, anxiety, apathy, and even psychotic symptoms like hallucinations or delusions. These manifestations can significantly reduce quality of life and increase caregiver burden, making their management a priority in dementia care.
Selective serotonin reuptake inhibitors (SSRIs) such as sertraline and citalopram are frequently prescribed to manage depression and anxiety. These drugs can stabilize mood and improve daily functioning, especially in the early to moderate stages of the disease. Antipsychotic medications, including risperidone and quetiapine, may be used sparingly and with caution, typically reserved for severe behavioral disturbances that pose a safety risk. Because of the potential for increased mortality and stroke risk in dementia patients taking antipsychotics, these drugs for vascular dementia are used only under close medical supervision.
Non-pharmacologic interventions, including cognitive behavioral therapy (CBT), music therapy, and structured routines, are often recommended alongside medication. However, when behavioral symptoms are particularly severe or unresponsive to non-drug approaches, medications may provide the necessary relief to stabilize the individual and improve interactions with their environment.
Individualizing Treatment Plans Based on Patient Profiles
Not all patients with vascular dementia will benefit equally from the same medications. Personalized treatment plans are essential, taking into account the patient’s cognitive profile, comorbid conditions, medication tolerability, and risk of adverse events. Experts emphasize the importance of routine cognitive assessments and close monitoring to adjust treatment plans as the disease progresses.
In elderly patients, polypharmacy is a concern. The interaction between different medications must be carefully evaluated, especially when multiple chronic conditions coexist. A patient taking anticoagulants for atrial fibrillation, for instance, may face increased bleeding risks if also prescribed antiplatelet agents. Balancing the benefits and risks of medication for vascular dementia requires a nuanced understanding of each individual’s unique health landscape.
Moreover, cultural, social, and family dynamics may influence treatment adherence and expectations. Involving caregivers in the decision-making process fosters better compliance and ensures that medication regimens align with the patient’s lifestyle and values. This holistic approach not only supports cognitive function but also enhances overall well-being.
The Evolving Landscape of Drug Research for Vascular Dementia
The search for more effective drugs for vascular dementia continues, with several promising avenues under investigation. Researchers are exploring medications that target neuroinflammation, oxidative stress, and endothelial dysfunction—all of which are implicated in vascular damage and cognitive decline.
Anti-inflammatory agents, such as minocycline and statins, are being studied for their potential neuroprotective effects. Likewise, antioxidants like vitamin E, resveratrol, and coenzyme Q10 are under evaluation for their ability to reduce oxidative damage to brain cells. Though these agents are not yet standard treatment, they represent the future of medication for vascular dementia by addressing its underlying mechanisms rather than just its symptoms.
Clinical trials are also examining drugs that enhance neuroplasticity and promote neurogenesis, aiming to regenerate damaged brain networks. These experimental therapies may one day complement existing treatments and provide new hope for slowing or even reversing cognitive impairment. Until then, optimizing current pharmacologic strategies remains the best course of action, guided by a continually evolving body of scientific evidence.
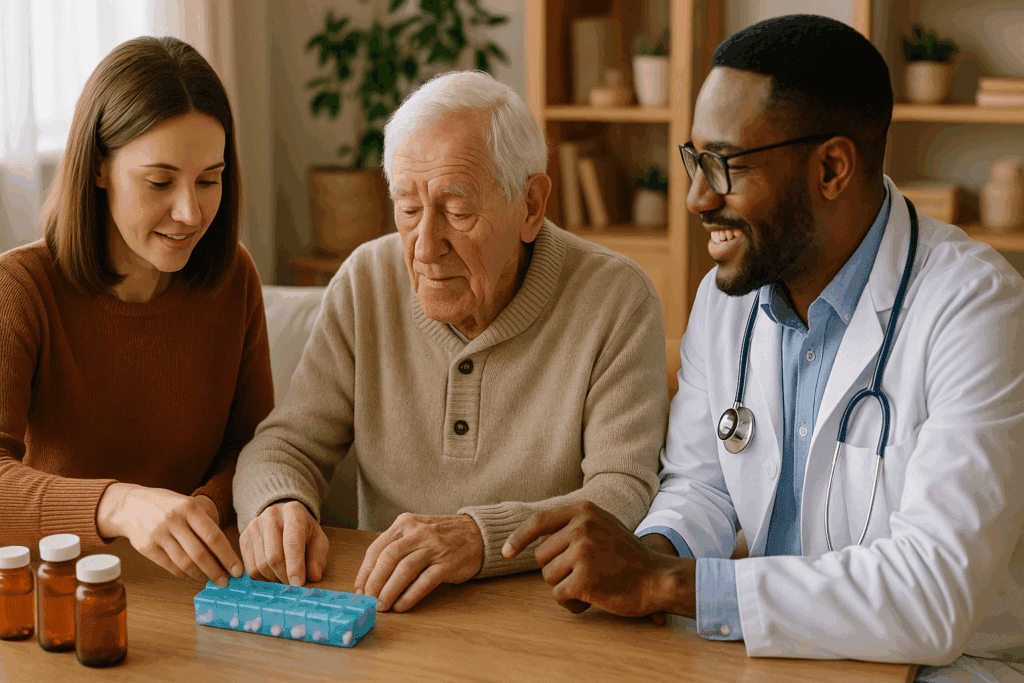
The Role of Caregivers and Healthcare Teams in Medication Management
Administering medication for vascular dementia requires more than simply writing a prescription. It involves careful coordination between healthcare providers, pharmacists, and family caregivers. Medication adherence can be challenging, particularly for patients with memory loss and executive dysfunction. Pill organizers, reminder systems, and caregiver education are vital tools in promoting consistent medication use.
Healthcare providers must routinely review medication effectiveness and side effects. Periodic cognitive assessments and behavioral evaluations can help determine whether the current regimen remains appropriate. Adjustments may be necessary to account for disease progression, changes in health status, or new research findings.
In this context, the partnership between the medical team and caregivers becomes invaluable. Caregivers are often the first to notice subtle changes in mood, behavior, or cognition, providing critical feedback that informs treatment decisions. Their role in supporting consistent drug administration and reporting adverse effects contributes significantly to the overall success of pharmacologic interventions.
Navigating the Challenges of Access and Affordability
Access to appropriate drugs for vascular dementia can be limited by cost, insurance coverage, and geographic location. Some newer medications may not be covered by standard insurance plans or may require prior authorization. This financial burden can deter families from pursuing optimal treatment, potentially compromising the patient’s care.
In rural or underserved areas, availability of specialists familiar with vascular dementia may be scarce, complicating the prescription and monitoring of complex drug regimens. Telemedicine has emerged as a valuable solution in such cases, offering remote consultations with neurologists or geriatricians who can guide treatment decisions.
Generic versions of key medications—such as donepezil, memantine, and many antihypertensives—can reduce costs and improve accessibility. Patient assistance programs and nonprofit organizations also provide support in navigating insurance challenges and securing necessary medications. Ensuring equitable access to effective treatments is a key component of ethical and effective dementia care.
Balancing Hope With Realism in Medication Outcomes
It is important to recognize the limitations of current medications for vascular dementia. While they can offer meaningful improvements in cognition, mood, and behavior, they are not curative. The progression of vascular dementia may be slowed, but not entirely halted, and expectations must be managed with both compassion and clarity.
Nonetheless, even modest improvements in mental clarity or reduction in agitation can significantly enhance the quality of life for both patients and caregivers. A well-managed medication regimen may allow individuals to maintain independence longer, engage in meaningful activities, and preserve dignity in the face of a challenging diagnosis.
Experts stress the value of comprehensive care that integrates pharmacologic, lifestyle, and psychosocial interventions. Nutrition, physical activity, mental stimulation, and social engagement all work synergistically with medication to support brain health. In this light, drugs for vascular dementia are not standalone solutions but vital components of a larger, person-centered approach.
Moving Forward: Integrating Innovation, Compassion, and Clinical Wisdom
As our understanding of vascular dementia deepens, so too will our ability to tailor medications to each individual’s unique needs. The future of treatment will likely involve a blend of conventional drugs, novel therapeutics, and precision medicine techniques that account for genetic, environmental, and lifestyle factors.
Until such advancements become widely available, the current focus remains on optimizing known treatments, enhancing medication adherence, and supporting patients through collaborative care. Medical professionals must stay informed about evolving guidelines and emerging research, while caregivers and families play an essential role in ensuring that pharmacologic strategies translate into meaningful, day-to-day improvements.
Ultimately, the use of medication for vascular dementia represents a critical opportunity to slow cognitive decline, manage distressing symptoms, and support the dignity and autonomy of those affected. While the road ahead may be complex, it is not without hope—especially when guided by the combined forces of scientific innovation, clinical expertise, and human compassion.
Final Thoughts: Medication for Vascular Dementia as Part of Holistic Cognitive Support
In conclusion, the role of medication for vascular dementia is multifaceted, offering both symptomatic relief and disease-modifying potential when used appropriately. Whether through direct cognitive enhancement, management of behavioral symptoms, or control of vascular risk factors, drugs for vascular dementia serve as essential tools in the effort to preserve brain function and quality of life.
However, their effectiveness depends on thoughtful integration into a broader care framework that includes personalized treatment planning, regular monitoring, caregiver involvement, and attention to psychosocial well-being. As new therapies emerge and existing drugs are better understood, the potential to transform the experience of living with vascular dementia grows ever more promising.
For families and healthcare providers alike, staying informed and engaged with evolving treatment options is the key to providing compassionate, evidence-based care. In this endeavor, medications are not simply pharmaceutical interventions but bridges to better understanding, deeper connection, and more hopeful outcomes for those navigating the challenges of vascular dementia.
Further Reading:
Medications for Memory, Cognition and Dementia-Related Behaviors