In recent years, the growing awareness of mental health issues has been accompanied by a surge in interest in evidence-based treatments. Among the most widely researched and implemented strategies for addressing anxiety disorders is exposure therapy. As public curiosity about therapeutic modalities grows, a common question arises: is exposure therapy a type of CBT, or does it stand alone as a distinct intervention? Understanding this relationship is critical not only for clinicians and researchers but also for individuals seeking effective treatment for anxiety. This article explores the intricate connection between exposure therapy and cognitive behavioral therapy (CBT), examining the theoretical foundations, clinical applications, and research evidence that support their use in treating anxiety.
You may also like: How Does CBT Work to Improve Relationships and Communication? Science-Backed Techniques for Getting Along with Others
Defining Exposure Therapy: Origins and Principles
Exposure therapy is a psychological treatment designed to help individuals confront and overcome fears, phobias, and anxieties by gradually and systematically exposing them to the feared stimuli in a controlled and safe environment. Rather than avoiding anxiety-provoking situations, which often reinforces fear, exposure therapy encourages direct engagement with these stimuli, allowing individuals to desensitize their fear response over time. The roots of exposure therapy can be traced back to classical conditioning theories and behavioral psychology, particularly the work of Ivan Pavlov and B.F. Skinner.
A cornerstone of this approach is the concept of habituation. As a person repeatedly encounters a feared object or situation without experiencing the anticipated negative outcome, their anxiety begins to diminish. This principle is complemented by the mechanism of extinction, wherein the learned association between a stimulus and a feared consequence is weakened. Exposure therapy often involves various forms of exposure, including in vivo (real-life), imaginal (visualizing the feared situation), and interoceptive (exposing individuals to feared bodily sensations).
Importantly, exposure therapy for anxiety is not a one-size-fits-all intervention. It must be tailored to the individual’s specific fears, history, and psychological profile. This personalization enhances effectiveness and fosters a sense of agency in the therapeutic process. Clinicians work collaboratively with clients to develop exposure hierarchies—graded lists of feared situations—guiding them through structured, step-by-step exposure exercises that build tolerance and resilience over time.
Cognitive Behavioral Therapy: An Integrated Framework
To address the question “is exposure therapy a type of CBT,” it is essential to understand what CBT entails. Cognitive behavioral therapy is a structured, time-limited, and goal-oriented approach that focuses on identifying and modifying dysfunctional thoughts, emotions, and behaviors. At its core, CBT is based on the cognitive model, which posits that thoughts influence emotions, which in turn influence behavior. By changing maladaptive thinking patterns, individuals can achieve emotional and behavioral change.
CBT encompasses a broad range of techniques, including cognitive restructuring, behavioral activation, problem-solving training, and relaxation strategies. It is highly empirical, with a strong emphasis on collaborative empiricism—where therapist and client work together to examine the validity of beliefs and assumptions. This scientific rigor underpins the credibility of CBT as a gold-standard treatment for numerous mental health conditions, particularly anxiety and depressive disorders.
Within the CBT framework, exposure therapy functions as one of several behavioral strategies. It is especially prominent in the treatment of anxiety-related disorders, where avoidance behaviors and catastrophic thinking are central features. Exposure techniques align seamlessly with CBT’s emphasis on behavioral experimentation and cognitive reappraisal, making them an integral part of many CBT protocols.
The Relationship Between Exposure Therapy and CBT
Exposure therapy is best understood not as a separate modality, but as a specialized technique embedded within the broader CBT paradigm. While it is possible to use exposure therapy outside of CBT—particularly in pure behavioral treatments—the most effective and empirically supported applications of exposure therapy for anxiety occur within a cognitive-behavioral framework.
In practical terms, this integration means that exposure exercises are often accompanied by cognitive interventions. For example, a client with social anxiety may be asked to give a short presentation in front of a small group (an exposure task) while also examining and challenging their automatic thoughts about being judged or ridiculed (a cognitive task). This dual approach targets both the behavioral and cognitive components of anxiety, producing more comprehensive and lasting change.
Moreover, research has consistently shown that combining cognitive and behavioral elements enhances treatment outcomes. Clients not only learn to tolerate anxiety-provoking situations but also develop a more balanced and realistic perspective on their fears. This synergy supports the conclusion that exposure therapy is indeed a type of CBT, particularly when used in a manner that incorporates cognitive restructuring and ongoing evaluation of progress.
Evidence Supporting Exposure Therapy for Anxiety
The effectiveness of exposure therapy for anxiety is among the most robustly supported findings in clinical psychology. Numerous randomized controlled trials, meta-analyses, and systematic reviews have demonstrated its efficacy across a wide range of anxiety disorders, including panic disorder, specific phobias, social anxiety disorder, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD).
For instance, in the treatment of OCD, exposure and response prevention (ERP)—a specialized form of exposure therapy—is considered the gold standard. In this approach, clients are exposed to anxiety-provoking stimuli while being prevented from engaging in compulsive rituals. Over time, this leads to habituation, reduced distress, and greater cognitive flexibility. Similarly, in PTSD treatment, prolonged exposure therapy helps individuals gradually process traumatic memories and reduce avoidance, leading to significant symptom reduction.
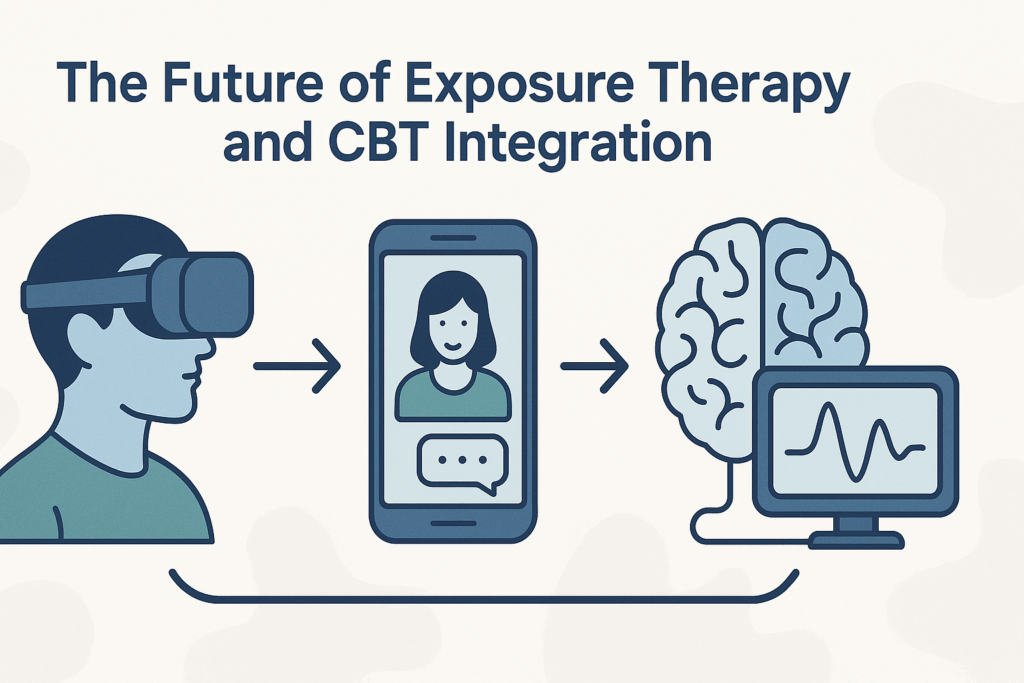
One of the strengths of exposure therapy lies in its adaptability. It can be delivered in individual or group formats, in clinical settings or through self-help protocols, and even via digital platforms. Virtual reality exposure therapy (VRET), for example, has emerged as a promising tool, allowing clients to confront fears in immersive, computer-generated environments. This innovation has expanded access to treatment and increased engagement among populations who may be reluctant to participate in traditional therapy.
Integrating Exposure Therapy in Clinical Practice
Incorporating exposure therapy into clinical practice requires a thoughtful and informed approach. Clinicians must be well-trained in both the theoretical underpinnings and practical implementation of exposure techniques. This includes understanding the principles of fear learning and extinction, as well as being able to manage client distress effectively during exposure tasks.
A key component of successful exposure therapy for anxiety is psychoeducation. Clients must understand the rationale behind exposure, including how avoidance maintains anxiety and how facing fears can promote change. This knowledge empowers clients and fosters trust in the therapeutic process. Additionally, clinicians must conduct thorough assessments to identify specific triggers, patterns of avoidance, and safety behaviors that may undermine exposure efforts.
Therapeutic alliance is also crucial. Because exposure therapy can be emotionally challenging, a strong, collaborative relationship between therapist and client provides a foundation of support. Therapists must validate the client’s experience while gently encouraging them to confront fears at a manageable pace. Flexibility is essential, as clients may progress at different rates and require adjustments to the exposure hierarchy.
Misconceptions and Barriers to Exposure Therapy
Despite its strong empirical foundation, exposure therapy is sometimes misunderstood or underutilized. One common misconception is that exposure therapy is inherently traumatic or harmful. In reality, when conducted ethically and competently, exposure therapy is a safe and effective way to reduce anxiety. It is never about forcing clients into overwhelming situations but rather guiding them through a gradual and collaborative process of fear reduction.
Another barrier is therapist reluctance. Some clinicians may avoid using exposure techniques due to concerns about client distress or a lack of confidence in their own skills. Addressing this requires improved training, supervision, and support for mental health professionals. Continuing education and experiential learning opportunities can help build competence and comfort with exposure-based interventions.
Client resistance can also pose a challenge. Individuals with anxiety disorders often experience intense fear at the thought of confronting their triggers, which can lead to avoidance of therapy altogether. To address this, clinicians must build motivation, set realistic expectations, and celebrate incremental progress. Helping clients reframe exposure as a path to empowerment rather than suffering can shift attitudes and increase engagement.
Cultural Considerations and Ethical Practice
Cultural factors can significantly influence how exposure therapy is perceived and received. Beliefs about mental health, fear, and therapy vary across cultures and may impact client willingness to engage in exposure tasks. Clinicians must approach treatment with cultural humility, seeking to understand the client’s worldview and incorporating culturally relevant values and practices into the therapeutic process.
Language barriers, stigma, and systemic disparities can also affect access to and outcomes of exposure therapy. Efforts to promote equity in mental health care must include culturally adapted protocols, outreach to underserved communities, and training for providers in cultural competence. Ethical practice demands that clinicians not only deliver evidence-based care but also ensure that such care is accessible, respectful, and responsive to individual needs.
The Future of Exposure Therapy and CBT Integration
The future of exposure therapy for anxiety lies in continued innovation, dissemination, and refinement. Technological advancements are opening new avenues for delivery, including mobile apps, virtual reality, and telehealth platforms. These tools can enhance accessibility, particularly for individuals in remote or underserved areas. Moreover, they offer opportunities for real-time monitoring, feedback, and personalization of treatment.
Research is also expanding our understanding of the mechanisms underlying exposure therapy. Studies on neurobiological correlates, such as changes in amygdala activity or connectivity between brain regions, are shedding light on how exposure leads to lasting change. This knowledge may inform the development of more targeted interventions and the integration of pharmacological agents to enhance learning during exposure.
As CBT continues to evolve, there is growing interest in transdiagnostic approaches that address underlying processes common across mental health conditions. Exposure-based strategies are well-suited to this paradigm, given their focus on reducing avoidance and increasing emotional tolerance. By framing exposure therapy as a core component of flexible, personalized care, clinicians can better meet the diverse needs of their clients.
Reflecting on the Role of Exposure Therapy in Evidence-Based Anxiety Care
In answering the question “is exposure therapy a type of CBT,” the evidence is clear: exposure therapy is not only compatible with CBT but thrives within its framework. As one of the most effective tools for treating anxiety, exposure therapy exemplifies the strengths of cognitive behavioral approaches—empirical grounding, structured intervention, and measurable outcomes. Its integration into CBT protocols enhances both the cognitive and behavioral dimensions of treatment, providing a comprehensive strategy for addressing the complexities of anxiety disorders.
The role of exposure therapy for anxiety extends beyond symptom reduction. It empowers individuals to reclaim agency over their fears, build resilience, and engage more fully with life. When implemented thoughtfully and ethically, exposure therapy offers a transformative path toward healing. As mental health care continues to prioritize evidence-based practice, exposure therapy stands as a vital component of compassionate, effective, and person-centered treatment. Understanding its place within CBT not only clarifies its role but also reinforces the value of integrative, research-informed care in promoting mental well-being.
Frequently Asked Questions: Exposure Therapy, CBT, and Anxiety Treatment
1. Can exposure therapy be used outside of traditional talk therapy settings?
Absolutely. While exposure therapy for anxiety is commonly associated with clinical sessions in structured therapy environments, it can also be implemented through digital platforms, mobile apps, and virtual reality systems. Many individuals now engage in exposure exercises at home under remote supervision or through guided self-help protocols. This flexibility has allowed people with mobility issues, limited access to clinicians, or high anxiety about in-person sessions to still benefit from exposure-based care. As exposure therapy for anxiety evolves, its presence in digital health continues to expand, empowering users to manage their anxiety in real-world contexts.
2. How does exposure therapy fit into trauma-informed care?
Exposure therapy for anxiety can be adapted within a trauma-informed framework, but it requires careful calibration. Trauma-informed care emphasizes safety, choice, and empowerment, which means exposure tasks must be approached collaboratively and with full client consent. For individuals with PTSD or complex trauma histories, exposure therapy often includes a slower pace, additional stabilization techniques, and integration with other therapeutic elements. While exposure therapy is a type of CBT, applying it within trauma contexts demands an enhanced sensitivity to triggers, dissociation, and the potential for retraumatization. Clinicians trained in trauma-focused CBT are best positioned to deliver this nuanced care effectively.
3. Are there age-specific considerations when using exposure therapy for anxiety?
Yes, developmental stage plays a significant role in how exposure therapy for anxiety is structured and delivered. With children and adolescents, clinicians often incorporate play-based methods, parental involvement, and age-appropriate metaphors to support understanding and motivation. For older adults, factors such as physical limitations, cognitive changes, or comorbid health issues may necessitate a slower pace or creative adjustments to the exposure hierarchy. While exposure therapy is a type of CBT applicable across the lifespan, the therapeutic alliance and mode of delivery must be tailored to each age group to optimize results.
4. Can exposure therapy backfire or worsen anxiety symptoms?
When not delivered correctly, exposure therapy for anxiety can indeed be counterproductive. If a client is pushed too quickly or without adequate preparation, it can reinforce fear or lead to premature termination of therapy. However, when implemented with proper pacing, consent, and cognitive support, exposure therapy typically results in decreased avoidance and long-term anxiety reduction. While exposure therapy is a type of CBT known for its efficacy, it demands expertise and sensitivity to prevent misapplication. Supervised training and ongoing consultation are essential for therapists who use exposure-based methods, particularly with complex cases.
5. What role do family members or caregivers play in exposure-based treatment?
In many cases, the involvement of family members can significantly enhance the outcomes of exposure therapy for anxiety. Supportive caregivers can assist in homework exercises, model adaptive behaviors, and help reduce accommodation of anxiety-driven avoidance. In CBT programs that incorporate exposure therapy, family psychoeducation is often part of the treatment plan. However, family members must be careful not to pressure or overprotect the individual, as either extreme can disrupt the therapeutic process. Ideally, their role is to create a safe, consistent environment that reinforces progress made during exposure tasks.
6. How does exposure therapy impact the brain’s response to fear over time?
Emerging neuroscience research sheds light on how exposure therapy for anxiety reshapes brain function. Repeated and controlled exposure reduces hyperactivity in the amygdala—the brain region linked to fear processing—while strengthening regulatory pathways in the prefrontal cortex. Over time, these neurological shifts support improved emotional regulation and decreased reactivity to previously feared stimuli. Although exposure therapy is a type of CBT grounded in behavioral principles, its effects are also deeply biological, contributing to lasting changes in how the brain perceives and responds to threats. These findings help validate exposure-based care from a neurobiological standpoint.
7. Is exposure therapy equally effective for all types of anxiety disorders?
While exposure therapy for anxiety is broadly effective, its application and results can vary depending on the disorder. Specific phobias, panic disorder, and OCD often respond quickly and robustly to exposure techniques. However, conditions like generalized anxiety disorder (GAD) or health anxiety may require more complex, cognitively driven approaches alongside exposure. Since exposure therapy is a type of CBT, it often works best when paired with cognitive restructuring or acceptance-based techniques in these cases. Treatment plans must therefore be individualized, with consideration given to the unique mechanisms sustaining each person’s anxiety.
8. How does cultural background influence a person’s experience with exposure therapy?
Cultural beliefs and values can deeply shape how individuals perceive both anxiety and therapeutic interventions. For some, openly confronting fears as encouraged in exposure therapy for anxiety may conflict with norms around emotional expression or coping. Language barriers, stigma, and mistrust of psychological services may also affect engagement. While exposure therapy is a type of CBT rooted in Western models of mental health, culturally adapted protocols are being developed to ensure more inclusive and effective care. These adaptations include incorporating cultural metaphors, respecting spiritual frameworks, and collaborating with community leaders to build trust.
9. Can exposure therapy be helpful even if anxiety isn’t the primary diagnosis?
Interestingly, exposure therapy for anxiety can also benefit individuals whose primary diagnoses involve mood disorders, eating disorders, or substance use. Many of these conditions include elements of avoidance or fear-based behavior patterns. For instance, individuals with depression may avoid social situations, while those with anorexia might fear specific foods. Although exposure therapy is a type of CBT primarily designed for anxiety, its techniques can be repurposed to address broader avoidance patterns. Integrative CBT approaches increasingly apply exposure strategies beyond traditional anxiety treatments.
10. What innovations are emerging in exposure therapy delivery and design?
The landscape of exposure therapy for anxiety is rapidly evolving with technological advancements. Virtual reality exposure therapy (VRET) now allows clients to confront specific fears—such as flying or public speaking—in immersive, controlled simulations. Mobile apps offer real-time guidance and tracking for exposure exercises, increasing accountability and accessibility. Biofeedback devices can be integrated to help users monitor physiological responses during exposure tasks. While exposure therapy is a type of CBT with decades of validation, its future lies in hybrid models that combine human support with AI-driven customization. These innovations hold promise for expanding reach, personalizing treatment, and enhancing long-term adherence.
Conclusion: Why Exposure Therapy Remains a Cornerstone in CBT for Anxiety Treatment
In the broader landscape of mental health interventions, few approaches offer the scientific rigor, adaptability, and clinical success seen in exposure therapy for anxiety. As we’ve explored throughout this article, not only is exposure therapy a type of CBT, but it is also one of its most impactful and empirically supported modalities. By directly addressing the behavioral avoidance and cognitive distortions that fuel anxiety, this method empowers individuals to gradually reclaim control over their responses to feared situations—replacing avoidance with resilience and fear with familiarity.
The question “Is exposure therapy a type of CBT?” may initially appear academic, but understanding the answer carries real-world implications for anyone navigating the challenges of anxiety. This isn’t simply a matter of semantics or classification; it’s about recognizing how evidence-based techniques like exposure therapy are grounded in a larger therapeutic philosophy that values cognitive restructuring, behavioral change, and emotional growth. When patients and clinicians alike grasp the foundational connections between exposure work and cognitive-behavioral strategies, they can tailor treatment with greater precision and confidence.
Moreover, the success of exposure therapy for anxiety is not limited to traditional in-office settings. Innovations such as virtual reality-assisted exposure, online CBT platforms, and telehealth delivery are expanding access and improving outcomes across diverse populations. These advancements speak to the enduring relevance of CBT principles in modern mental healthcare and highlight the flexibility of exposure therapy as a tool for long-term recovery. Whether used to address specific phobias, social anxiety, panic disorder, or PTSD, exposure therapy stands as a testament to what structured, methodical, and compassionate treatment can achieve.
Ultimately, recognizing exposure therapy as a form of CBT allows both patients and practitioners to appreciate its deeper theoretical roots and practical versatility. It reminds us that facing fears is not just a metaphorical phrase but a measurable, achievable process guided by science and supported by decades of clinical practice. For individuals living with anxiety, this realization can mark the beginning of a new chapter—one defined not by avoidance, but by agency, healing, and renewed confidence in their ability to live fully.
Further Reading:
Exposure Therapy: What It Is, What It Treats & Types
The Practice of Exposure Therapy: Relevance of Cognitive-Behavioral Theory and Extinction Theory