The aftermath of trauma is rarely a singular event. Its effects linger in the body and mind, reshaping emotional patterns, daily behavior, and even long-term relationships. While the immediate impact of traumatic experiences may subside over time for some individuals, for many others, unresolved trauma becomes a persistent undercurrent that influences their psychological well-being and sense of safety in the world. This enduring impact often presents as anxiety, emotional dysregulation, hypervigilance, avoidance behaviors, or intrusive memories. In addressing these patterns, trauma-focused cognitive behavioral therapy (TF-CBT) offers a highly structured and research-supported pathway toward healing.
You may also like: How Does CBT Work to Improve Relationships and Communication? Science-Backed Techniques for Getting Along with Others
As both a treatment modality and a therapeutic philosophy, TF-CBT has emerged as a cornerstone of trauma-informed mental health care. Developed initially to support children and adolescents, it is now widely used across diverse age groups and populations. By integrating the core principles of cognitive behavioral therapy with trauma-sensitive techniques, this approach helps individuals reprocess traumatic events, restructure maladaptive thought patterns, and gradually rebuild emotional stability. But what distinguishes trauma cognitive behavioral therapy from standard CBT models is its dual emphasis on symptom management and trauma resolution. Rather than simply modifying behavior, focused cognitive behavioral therapy creates space for individuals to reclaim their narratives, restore a sense of safety, and reconnect with emotions that trauma once distorted or suppressed.
Understanding the Foundations of Trauma-Focused Cognitive Behavioral Therapy
At its core, trauma-focused cognitive behavioral therapy merges established cognitive-behavioral principles with elements specifically designed to address the psychological ramifications of trauma. Traditional CBT focuses on the dynamic interaction between thoughts, feelings, and behaviors, guiding individuals to challenge cognitive distortions and develop healthier responses. In TF-CBT therapy, these foundational tools are maintained, but the therapeutic process also attends to trauma-specific symptoms, including avoidance, emotional numbing, and physiological hyperarousal.
TF-CBT is particularly effective for those experiencing post-traumatic stress disorder (PTSD), complex trauma, or trauma-related anxiety and depression. What sets it apart is its structured, phased approach: beginning with stabilization and coping skills, followed by trauma narration and processing, and culminating in integration and future safety development. This phased model not only supports gradual exposure to traumatic memories but also empowers clients with skills to manage distress before engaging with emotionally charged material.
A key principle of focused cognitive behavioral therapy is its collaborative nature. Clients are not passive recipients of treatment but active participants in shaping their therapeutic journey. Therapists work closely with individuals to build trust, normalize trauma reactions, and tailor interventions to meet unique needs. This flexibility ensures that the therapeutic process honors each client’s experience while grounding treatment in evidence-based practices.
Rewiring the Brain: Neurobiological Insights Into Trauma and Healing
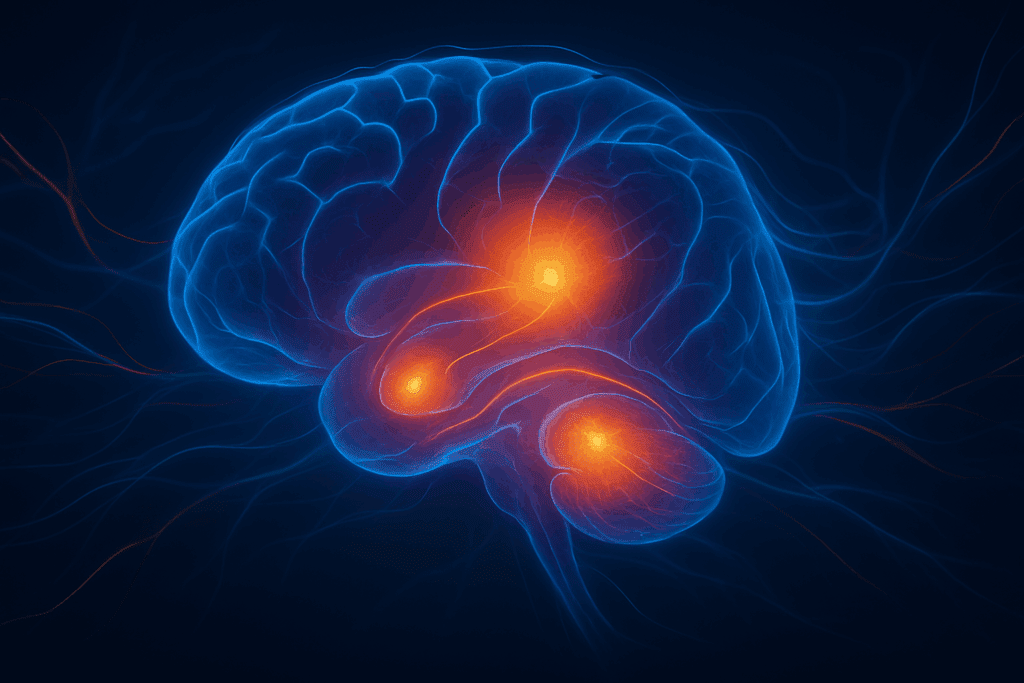
Trauma is not only a psychological wound; it is also a neurological event. Emerging research in neuroscience has illuminated the profound impact of trauma on brain function and development. Areas such as the amygdala, hippocampus, and prefrontal cortex are particularly affected, leading to heightened fear responses, memory fragmentation, and impaired emotion regulation. TF-CBT therapy aims to interrupt these maladaptive neural circuits by introducing new patterns of thinking, feeling, and behaving.
Through repeated exposure to adaptive cognitive and behavioral strategies, the brain can gradually form new connections. Neuroplasticity—the brain’s capacity to change—plays a crucial role in this process. When individuals learn to reframe negative thoughts, confront avoidance, and tolerate distress in a safe environment, they engage in mental exercises that strengthen neural pathways associated with resilience and emotional regulation.
In practice, this means that each session of trauma cognitive behavioral therapy contributes to long-term changes in the way the brain processes fear, memory, and emotion. By incorporating relaxation techniques, mindfulness exercises, and narrative restructuring, therapists help clients recalibrate their physiological and emotional responses. Over time, previously triggering stimuli may lose their power, allowing individuals to navigate life with increased confidence and reduced fear.
The Role of Narrative in Reclaiming Personal Agency
One of the most powerful tools in TF-CBT is trauma narration—a structured process in which individuals share their traumatic experiences in a safe, supportive environment. This practice may initially seem counterintuitive, especially to those who have spent years trying to suppress painful memories. Yet research consistently shows that when traumatic experiences are avoided rather than processed, they retain their psychological grip. Narration transforms avoidance into agency.
Telling one’s trauma story does not mean reliving the pain. Instead, it provides an opportunity to organize fragmented memories, integrate cognitive understanding, and gain perspective. In TF-CBT therapy, narration is approached gradually and respectfully. Clients choose how much to share, when to share it, and how to frame their story. This sense of control is essential, especially for survivors of interpersonal violence, abuse, or exploitation, whose autonomy may have been severely compromised.
Moreover, focused cognitive behavioral therapy views narration not merely as a disclosure but as a meaning-making process. Clients are guided to examine beliefs that may have formed during or after the trauma—such as self-blame, hopelessness, or mistrust—and to challenge these beliefs through evidence-based techniques. In doing so, individuals can reframe their identity not around victimization, but around survival, strength, and growth.
Building Emotional Regulation and Coping Skills
Emotional dysregulation is a hallmark of trauma-related disorders. Intense emotional reactions, mood swings, irritability, and emotional numbing can interfere with daily functioning and strain relationships. A central focus of trauma cognitive behavioral therapy is equipping clients with tools to regulate these overwhelming emotions.
Before diving into trauma processing, therapists work with clients to establish a toolkit of coping strategies. These may include deep breathing, progressive muscle relaxation, cognitive restructuring, and emotion identification exercises. While these skills may appear simple on the surface, their consistent application can have profound effects. They provide a sense of predictability and control, which can be deeply reassuring for individuals who have experienced chaos or danger.
Importantly, TF-CBT also addresses the role of avoidance—an understandable but ultimately counterproductive coping mechanism. By gently guiding clients to confront distressing memories or situations in a controlled, therapeutic context, the therapy fosters emotional resilience. Over time, clients learn that they can survive emotional discomfort without becoming overwhelmed, which reinforces a sense of mastery and self-efficacy.
Addressing Developmental and Cultural Considerations
Trauma manifests differently across age groups and cultural backgrounds. What may be experienced as a traumatic event in one context might not have the same psychological impact in another. TF-CBT recognizes these variations and incorporates developmentally appropriate and culturally sensitive practices into its framework.
For children and adolescents, therapy often includes caregivers as active participants. This family component of trauma cognitive behavioral therapy helps to strengthen attachment relationships, improve communication, and provide a supportive home environment for healing. Caregivers are taught how to respond to trauma symptoms, model healthy coping, and reinforce therapeutic skills outside the session.
Cultural considerations are equally vital. Beliefs about trauma, mental health, and emotional expression vary widely across cultures, and therapists are trained to respect and integrate these perspectives. In some communities, collective healing practices or spiritual frameworks may complement the therapeutic process. By honoring these traditions while maintaining clinical rigor, TF-CBT becomes more accessible and effective across diverse populations.
Restoring Trust and Rebuilding Relationships
Trauma often disrupts interpersonal trust, especially when the source of trauma is relational in nature. Survivors of abuse, neglect, or betrayal may struggle to form secure attachments or to feel safe with others. One of the long-term goals of focused cognitive behavioral therapy is to help individuals reestablish trust—both in themselves and in their relationships.
TF-CBT addresses relational challenges by helping clients explore and correct maladaptive beliefs about others, such as the assumptions that people are inherently dangerous or that vulnerability always leads to harm. These beliefs, while protective in the immediate aftermath of trauma, can hinder intimacy and connection over time. Therapy gently challenges these patterns through behavioral experiments, cognitive restructuring, and gradual exposure to social situations.
In addition, therapists model consistent, respectful, and empathic interactions. This therapeutic relationship becomes a safe space in which clients can test new ways of relating. Over time, as individuals experience trustworthy relationships within therapy, they are more likely to seek and sustain such connections outside of it. The restoration of trust is not only a psychological milestone but a foundational step toward holistic well-being.
Preventing Retraumatization and Promoting Long-Term Resilience
While the initial stages of TF-CBT are designed to build safety and stability, long-term success depends on the prevention of retraumatization and the cultivation of resilience. Trauma recovery is not a linear process, and setbacks may occur. However, when clients have internalized coping skills, built support systems, and redefined their narratives, they are better equipped to handle future stressors.
Therapists emphasize the importance of relapse prevention planning. This includes identifying potential triggers, developing proactive strategies, and reinforcing strengths gained through therapy. Clients are encouraged to view recovery as an ongoing journey rather than a finite goal. By setting realistic expectations and recognizing incremental progress, they can maintain motivation and self-compassion.
Focused cognitive behavioral therapy also fosters resilience by helping individuals reconnect with values, goals, and sources of meaning. Trauma may have disrupted one’s sense of purpose or identity, but therapy provides space to explore these themes anew. Whether through creative expression, volunteerism, spirituality, or career aspirations, clients are supported in building lives that feel fulfilling and self-directed.
Integrating TF-CBT Into Broader Mental Health Systems
As TF-CBT continues to demonstrate its effectiveness in clinical settings, there is growing interest in integrating it into broader mental health systems, schools, and community programs. Its structured framework and strong evidence base make it a valuable addition to trauma-informed care models.
In school settings, TF-CBT can be adapted to support children who have experienced bullying, domestic violence, or community trauma. Trained school counselors and psychologists can deliver the core components of the model, providing early intervention and preventing escalation of symptoms. Similarly, community mental health agencies are increasingly adopting trauma cognitive behavioral therapy to serve individuals affected by poverty, displacement, or systemic violence.
The accessibility of TF-CBT is also enhanced by telehealth platforms, which allow clients in rural or underserved areas to receive care. As digital therapy becomes more prevalent, efforts are underway to ensure that virtual TF-CBT maintains fidelity to its evidence-based components while adapting to the unique dynamics of remote interaction.
Frequently Asked Questions: Trauma-Focused Cognitive Behavioral Therapy
1. Can trauma cognitive behavioral therapy be effective for individuals who don’t meet full PTSD diagnostic criteria?
Absolutely. Trauma cognitive behavioral therapy is not limited to individuals diagnosed with post-traumatic stress disorder. Many people experience subthreshold trauma symptoms—such as chronic anxiety, emotional numbing, or flashbacks—without meeting full diagnostic criteria. TF-CBT therapy offers structured interventions that can still address these symptoms effectively, especially when they interfere with daily functioning or quality of life. In fact, early intervention using focused cognitive behavioral therapy can prevent the escalation of symptoms and promote healthier long-term emotional patterns. It’s a proactive approach, not just a reactive one, which is why therapists increasingly recommend TF-CBT for individuals dealing with unresolved trauma-related stress.
2. How does TF-CBT differ from exposure therapy when treating trauma?
While both approaches may involve revisiting traumatic memories, they differ significantly in their methodology and emotional pacing. TF-CBT therapy emphasizes safety, emotion regulation, and cognitive restructuring before exploring trauma narratives. In contrast, traditional exposure therapy often begins more directly with prolonged exposure to traumatic stimuli to desensitize the emotional response. Trauma cognitive behavioral therapy builds a foundation of trust and coping skills first, which can make it more tolerable—especially for individuals who are emotionally overwhelmed or those with complex trauma. This distinction allows focused cognitive behavioral therapy to serve a broader and more diverse client population, including children and those with concurrent mental health diagnoses.
3. Is TF-CBT suitable for adults, or is it primarily a treatment for children and adolescents?
While TF-CBT was originally developed for younger populations, it has evolved and proven effective for adults as well. Many therapists adapt the core principles of trauma cognitive behavioral therapy to meet the needs of adult clients facing trauma from childhood abuse, military service, domestic violence, or other life-altering events. Adult clients often bring deeper cognitive and emotional insight into therapy, which can enhance the impact of cognitive restructuring and trauma processing. Focused cognitive behavioral therapy in adult populations may incorporate more advanced mindfulness practices and explore existential concerns related to identity and meaning. The versatility of TF-CBT therapy makes it a valuable tool across age groups.
4. What happens if someone feels worse during the course of TF-CBT therapy?
Temporary emotional discomfort is a common and expected part of trauma work, especially as repressed memories and emotions are brought to the surface. However, trauma cognitive behavioral therapy is designed to prevent emotional flooding by equipping clients with coping strategies before trauma processing begins. If distress increases during TF-CBT therapy, therapists can slow the pace, revisit grounding skills, or shift focus temporarily to stabilization. Feeling worse before feeling better doesn’t indicate failure—instead, it often signals that previously avoided emotions are being engaged. With a strong therapeutic alliance, these moments can become turning points toward deeper healing in focused cognitive behavioral therapy.
5. How does TF-CBT integrate with medication management in trauma treatment?
Many individuals benefit from a combined approach involving both therapy and pharmacological support. TF-CBT therapy can work in tandem with medications such as SSRIs, which help manage symptoms like anxiety and depression that frequently accompany trauma. When emotional regulation is bolstered pharmacologically, clients may be better able to engage in trauma narrative work and cognitive restructuring. Collaboration between therapists and prescribing physicians ensures that both aspects of care are aligned and responsive to client needs. Trauma cognitive behavioral therapy does not rely on medication, but when thoughtfully integrated, medication can enhance the overall treatment outcomes of focused cognitive behavioral therapy.
6. Are there digital tools that support the practice of focused cognitive behavioral therapy?
Yes, the digital landscape has introduced a range of tools that can complement in-person TF-CBT sessions. These include mobile apps that reinforce coping strategies, digital journaling platforms for trauma narratives, and guided audio resources for relaxation or mindfulness. Some telehealth platforms now offer full TF-CBT therapy protocols with therapist support, expanding access to individuals in remote or underserved communities. These tools can make trauma cognitive behavioral therapy more engaging and sustainable between sessions, especially for younger clients accustomed to digital interaction. However, therapists remain critical in ensuring that technology is used thoughtfully and does not replace the human connection central to focused cognitive behavioral therapy.
7. How is TF-CBT adapted for clients who have experienced racial, cultural, or systemic trauma?
TF-CBT therapy has evolved to incorporate cultural humility and responsiveness, acknowledging that trauma is shaped by social and historical context. For clients who have experienced racial or systemic trauma, therapy must validate those experiences without pathologizing the individual. Culturally adapted trauma cognitive behavioral therapy includes exploring intergenerational trauma, integrating community healing traditions, and challenging internalized beliefs rooted in societal injustice. Therapists trained in cultural competence can adapt focused cognitive behavioral therapy frameworks to ensure that they reflect the client’s lived experiences and identity. This inclusive approach helps TF-CBT become a vehicle for both individual and collective healing.
8. What role does the therapeutic relationship play in the success of trauma cognitive behavioral therapy?
The therapeutic alliance is a foundational component of successful TF-CBT therapy. Clients are often revisiting the most vulnerable aspects of their lives, so trust, safety, and empathy are essential. A strong therapist-client relationship facilitates open communication, reduces fear of judgment, and encourages clients to take emotional risks necessary for healing. In focused cognitive behavioral therapy, therapists actively model healthy interpersonal dynamics, which can repair relational templates damaged by trauma. Beyond technique, it is the quality of this connection that often determines the depth and durability of healing in trauma cognitive behavioral therapy.
9. How can caregivers or family members support someone undergoing TF-CBT?
Support from family members or caregivers can significantly enhance the outcomes of TF-CBT therapy. By learning about trauma responses and the goals of treatment, caregivers can provide emotional reinforcement and reduce stigma. In pediatric and adolescent cases, caregivers may be included directly in sessions to help normalize reactions, reinforce coping strategies, and create a safe environment outside of therapy. For adults, supportive family dynamics may involve respecting boundaries, being patient during emotional fluctuations, and encouraging consistency in attending sessions. Focused cognitive behavioral therapy emphasizes that healing is not isolated to the individual—it often thrives in supportive, informed relational contexts.
10. What are some long-term outcomes for individuals who complete TF-CBT therapy?
Long-term studies show that individuals who complete TF-CBT therapy often experience sustained improvements in emotional regulation, interpersonal relationships, and overall mental health. Many report decreased symptoms of anxiety and depression, as well as improved sleep and concentration. Beyond symptom reduction, trauma cognitive behavioral therapy fosters a renewed sense of agency, allowing clients to pursue goals that were previously obstructed by trauma. Focused cognitive behavioral therapy also teaches transferrable skills that can be applied to future stressors, increasing resilience and adaptability. For many, the conclusion of TF-CBT marks not just the end of treatment, but the beginning of a more empowered, emotionally coherent life.
Conclusion: Rewiring Emotional Patterns Through Trauma-Informed Healing
The emotional patterns forged in the wake of trauma are not immutable. With the right tools, guidance, and therapeutic alliance, individuals can reshape their responses, challenge harmful beliefs, and reengage with life in empowering ways. Trauma-focused cognitive behavioral therapy offers a pathway for this transformation—grounded in science, delivered with compassion, and tailored to the unique needs of each individual.
By integrating cognitive restructuring with trauma processing, TF-CBT therapy helps to dismantle the emotional barriers that once served as survival mechanisms but now limit growth. Through narrative healing, emotional regulation, and relationship repair, clients can move beyond the fear and isolation that trauma often breeds. Most importantly, focused cognitive behavioral therapy reminds survivors that healing is possible—not by forgetting the past, but by facing it with courage, support, and new understanding.
As the demand for trauma-informed care grows, the role of TF-CBT will continue to expand. Its adaptability, accessibility, and strong research foundation position it as a leading intervention in the field of mental health. For those navigating the complexities of trauma recovery, it offers not just hope, but a clear, evidence-based roadmap toward healing and resilience.
Further Reading:
Trauma-Focused Cognitive Behavioral Therapy
How Therapy Helps Rewire the Brain After Trauma
How Trauma Rewires the Brain: Insights from a CBT Therapist
.