The hip flexors, often overlooked in everyday fitness discussions, are a critical group of muscles responsible for hip flexion, enabling us to walk, run, and lift our legs. These muscles play an integral role in lower-body biomechanics and postural alignment, making their health essential for pain-free movement. When these muscles are strained, tight, or injured, they can cause considerable discomfort and functional impairment. This article explores in-depth how to fix hip flexor pain using evidence-based stretching techniques, highlighting expert-approved strategies for rehabilitation, prevention, and long-term recovery.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Understanding the Hip Flexor Muscles and Their Role in Movement
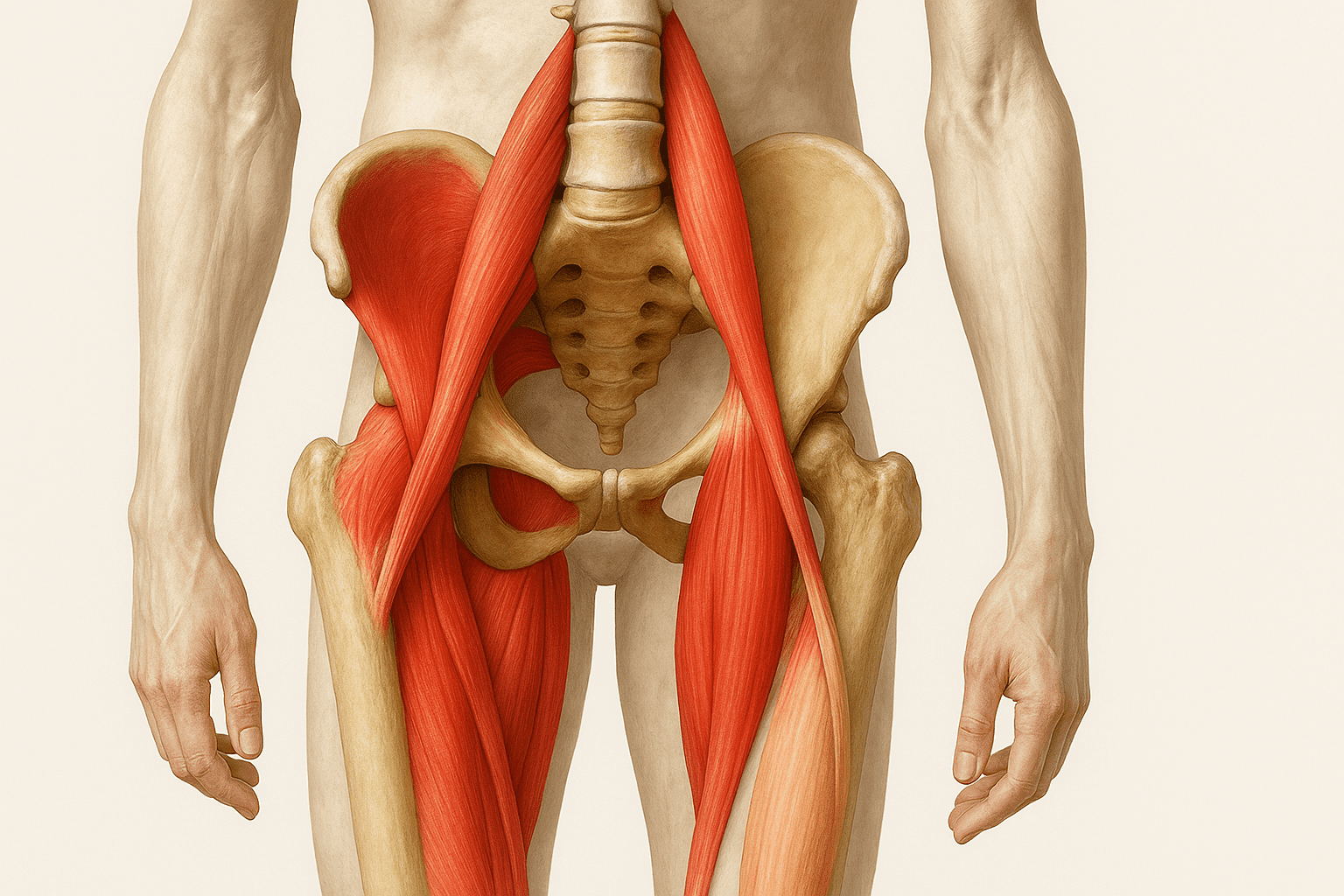
To address hip flexor pain effectively, we must first understand the anatomy and function of these muscles. The primary hip flexor muscles include the iliopsoas (comprised of the psoas major and iliacus), rectus femoris, sartorius, and tensor fasciae latae. These muscles originate from the lumbar spine and pelvis and insert into the femur, allowing the leg to lift toward the torso. Hip flexion is essential for dynamic movements such as sprinting, climbing stairs, and transitioning from sitting to standing.
When someone asks, “Where is your hip flexor?” the answer involves a complex muscular network deep within the anterior hip region. The psoas major, for example, connects the spine to the femur, stabilizing both the lumbar spine and the pelvis during movement. Unfortunately, modern sedentary lifestyles contribute to the shortening and tightening of these muscles. Prolonged sitting, poor posture, and repetitive overuse can lead to sore hip flexors, chronic tightness, and functional limitations.

Symptoms of Tight Hip Flexors and Common Causes of Injury
Recognizing the symptoms of tight hip flexors is crucial for early intervention and effective treatment. Individuals often report a dull ache in the front of the hip, pain during hip flexion, or discomfort while transitioning from a seated to a standing position. Hip flexor pain when sitting, walking, or running can be early warning signs of underlying dysfunction. In more severe cases, people experience sharp pain in the hip flexor when lifting the leg, particularly during athletic activity or after prolonged periods of rest.
The causes of hip flexor pain are varied but often include acute strain, chronic overuse, or postural imbalances. Athletes, particularly runners, are prone to running hip flexor pain due to repetitive stress on the iliopsoas during the gait cycle. Likewise, office workers and individuals who sit for extended periods frequently experience symptoms of tight hip flexors due to adaptive muscle shortening. The accumulation of microtrauma without adequate recovery leads to strain and injury, necessitating a comprehensive rehabilitation strategy.
What Should I Do When I Injure My Hip Flexor?
When dealing with a hip flexor injury, the initial step should be to cease any aggravating activities to prevent further damage. Applying ice, resting the area, and using compression can help reduce inflammation in the early stages. Many wonder, “What should I do when I injure my hip flexor?” The answer depends on the severity of the injury, but most cases respond well to conservative management involving physical therapy and targeted stretching.
Early intervention is vital for minimizing long-term dysfunction. Pain in the hip flexor when lifting the leg rehab should focus on restoring range of motion without exacerbating symptoms. Once acute inflammation subsides, gentle hip flexor stretching and progressive loading can be introduced. Understanding how to heal a hurt hip flexor involves balancing rest with movement, avoiding both excessive immobilization and premature return to high-intensity activity.
How to Heal Hip Flexor Strain and Promote Recovery
A hip flexor strain occurs when the muscle fibers are overstretched or torn, often due to explosive movements or overexertion. To heal a hip flexor strain, a structured rehabilitation plan should include phases of recovery—beginning with protection and progressing to mobility, strength, and return to function. In the early stages, isometric contractions can maintain muscle engagement without risking further strain. As symptoms improve, dynamic mobility exercises can restore functional capacity.
Those wondering how to heal hip flexor pain should focus on gradual reintroduction of movement patterns. Hip flexor muscle strain treatment should incorporate not only stretching but also strength training for the surrounding musculature, including the glutes, hamstrings, and core. These muscle groups work synergistically to stabilize the pelvis and prevent compensatory overuse of the hip flexors. Chronic hip flexor pain treatment often requires addressing biomechanical imbalances and postural habits that contribute to persistent discomfort.

Effective Hip Flexor Stretches to Cure Hip Flexor Pain
Stretching is a cornerstone of hip flexor treatment and offers an effective strategy to alleviate tightness, improve flexibility, and reduce pain. One of the most effective stretches is the kneeling hip flexor stretch, which targets the iliopsoas while encouraging spinal extension. To perform this stretch, kneel on one knee with the opposite foot in front, forming a 90-degree angle. Tucking the pelvis under and gently shifting forward increases the stretch across the front of the hip.
Another effective approach is the couch stretch, which enhances flexibility in the rectus femoris by extending the hip and knee simultaneously. These movements, when performed consistently, help cure hip flexor pain by elongating tight muscle fibers and restoring normal joint mechanics. Foam rolling the quadriceps and hip flexor region can also improve tissue mobility and facilitate deeper stretches.
Practitioners must emphasize proper form and breathing during stretches to maximize effectiveness and reduce the risk of aggravating symptoms. Hip flexor pain when walking often stems from muscle tension and poor gait mechanics, both of which can be corrected with diligent mobility work. Understanding how to alleviate hip flexor pain through stretching empowers individuals to manage symptoms proactively and prevent recurrence.

How to Treat Hip Flexor Pain with Mobility and Strength Training
While stretching is vital, strengthening the surrounding musculature is equally important in hip flexor treatment. A well-rounded approach to how to treat hip flexor pain involves activating underused muscles and improving neuromuscular coordination. For instance, weak glutes often lead to compensatory overuse of the hip flexors, perpetuating a cycle of pain and dysfunction. Glute bridges, clamshells, and resistance band exercises can re-establish balance and prevent overload.
Incorporating dynamic exercises such as leg swings and lunges improves both hip flexion and extension range of motion, allowing for smoother, more efficient movement patterns. These exercises are particularly beneficial for those experiencing hip flexor pain while sitting or transitioning between positions. Functional mobility drills should be progressed gradually, ensuring that the individual can perform each movement without compensatory patterns or pain.
Many athletes also inquire about how to fix a hip flexor injury when returning to sport. The key lies in a phased reintroduction of sport-specific drills that mimic the demands of their activity. Sprint drills, agility ladders, and plyometric training can be added once foundational mobility and strength are restored. Regular assessments by a physical therapist can guide this process and ensure safe progression.
The Importance of Postural Awareness and Ergonomics
Postural habits play a significant role in the development and persistence of hip flexor pain. Prolonged slouching, anterior pelvic tilt, and improper seated alignment all contribute to increased strain on the hip flexor muscles. Understanding how to heal a hurt hip flexor includes cultivating awareness of one’s posture throughout daily activities, not just during workouts. Ergonomic adjustments to chairs, desks, and computer screens can reduce sustained stress on the anterior hip.
Incorporating micro-movements and standing breaks throughout the day helps mitigate the effects of prolonged sitting. Standing desks and active sitting options, such as stability balls or kneeling chairs, encourage dynamic positioning of the pelvis and spine. These strategies reduce the likelihood of developing sore hip flexors from repetitive postural strain and support long-term joint health.
Educating patients on proper postural alignment during both static and dynamic tasks is essential for sustained recovery. Whether walking, driving, or exercising, maintaining neutral pelvic alignment prevents compensatory patterns and reduces the load on the hip flexors. By adopting these ergonomic and postural principles, individuals gain greater control over their recovery and reduce the risk of future injury.
Chronic Hip Flexor Pain Treatment and Long-Term Solutions
For individuals dealing with long-standing discomfort, chronic hip flexor pain treatment requires a more nuanced and multifaceted approach. In such cases, imaging studies or a consultation with an orthopedic specialist may be necessary to rule out underlying conditions such as labral tears, tendinopathy, or femoroacetabular impingement. Once structural issues are addressed or ruled out, a comprehensive rehabilitation plan can be implemented.
Persistent pain in the hip flexor when lifting the leg rehab often reveals deficits in motor control or compensatory mechanics. Rehabilitation programs should be individualized based on movement assessments and functional testing. Manual therapy, including soft tissue mobilization and joint manipulation, can complement active treatment strategies to restore range of motion and reduce tissue adhesions.
Those searching for how to treat a hurt hip flexor in chronic cases must also consider lifestyle factors such as stress, sleep, and systemic inflammation. Nutritional support, hydration, and adequate recovery all influence tissue healing and resilience. Mind-body practices like yoga and meditation can enhance proprioception and reduce muscle guarding, further supporting healing efforts.
Understanding the Role of Antagonist Muscles and Synergistic Inhibition
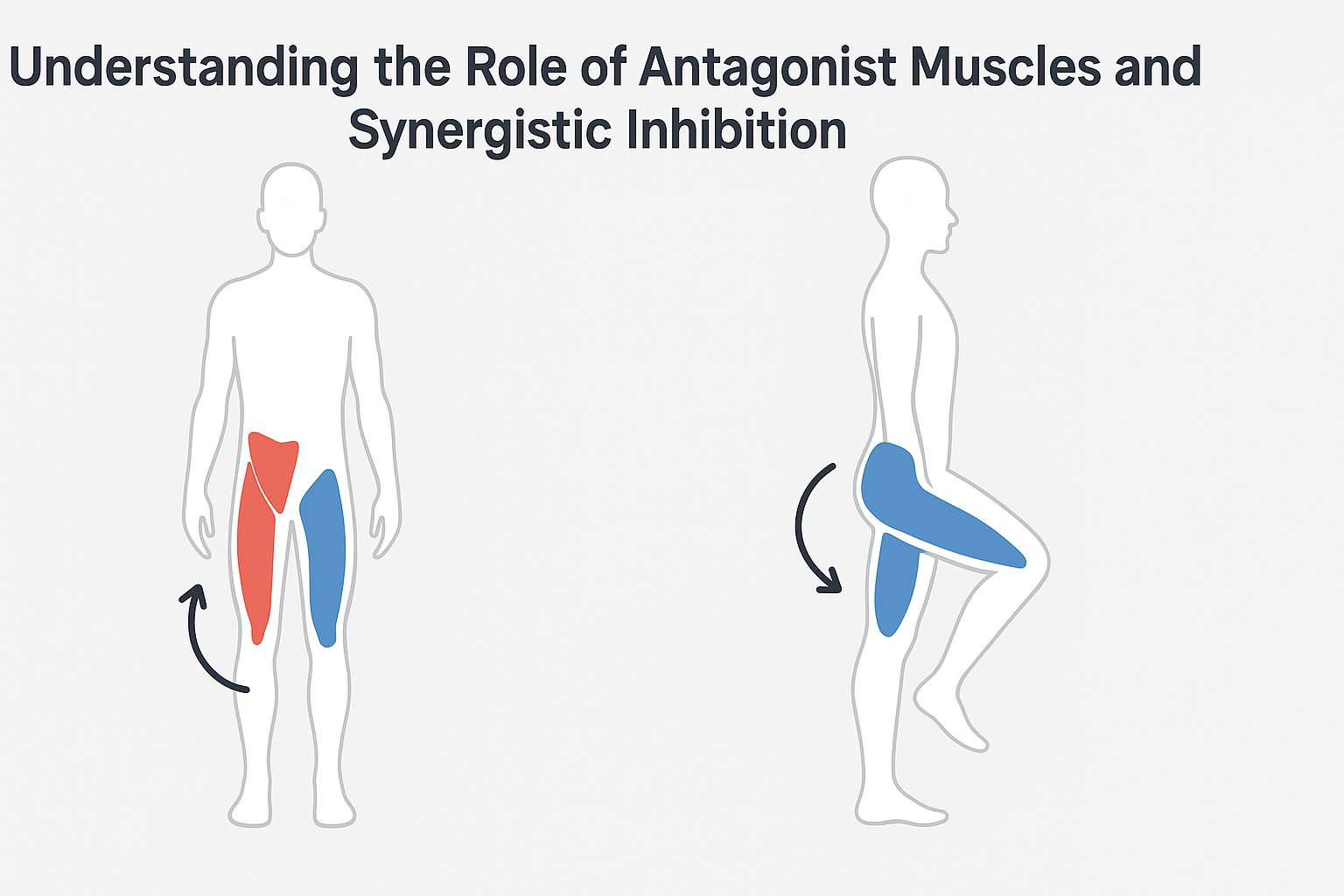
Muscles work in pairs, with one contracting while the other lengthens. In the case of hip flexion, the primary antagonists are the gluteus maximus and hamstrings. Weak or underactive antagonists can lead to overcompensation by the hip flexors, contributing to chronic overuse injuries. This phenomenon, known as reciprocal inhibition, emphasizes the importance of gluteal activation in hip flexor rehabilitation.
Incorporating targeted glute exercises, such as hip thrusts, banded lateral walks, and single-leg Romanian deadlifts, can re-establish muscular balance around the hip. Moreover, activating the posterior chain before engaging in dynamic movement helps prevent the hip flexors from becoming dominant. This strategy is particularly relevant for athletes with anterior pelvic tilt or swayback posture, where gluteal inhibition is common.
Synergistic inhibition can also occur when supporting stabilizers like the transverse abdominis or adductors are weak, placing additional load on the hip flexors. Functional movement screens and electromyographic testing can identify these imbalances and inform a more precise training program. By addressing the root causes of compensation, patients can achieve more durable and sustainable recovery outcomes.

Neurodynamics and Nerve Flossing Techniques
In some cases, hip flexor pain is not solely muscular but involves neural tension—particularly of the femoral nerve, which travels through the iliopsoas region. Entrapment or irritation of this nerve can produce symptoms that mimic muscular pain, such as burning, tingling, or sharp discomfort during hip flexion. Nerve flossing, also known as neurodynamic mobilization, offers a non-invasive solution to restore nerve glide and reduce sensitization.
A basic femoral nerve glide involves lying prone, supporting the upper body with the forearms, and gently bending one knee while keeping the pelvis stable. This movement lengthens the femoral nerve pathway and can be progressed with gentle oscillations or head movements to increase the stretch. When performed consistently, nerve glides reduce neural tension and improve mobility without triggering protective muscle spasms.
Integrating neurodynamic techniques is particularly useful when traditional stretching fails to produce results or exacerbates symptoms. It also complements fascial and soft tissue interventions, offering a comprehensive approach to managing complex hip flexor presentations.
Visualizing Anatomy: Picture of Hip Flexor Muscle Function in Motion
For a deeper understanding of hip flexor dynamics, visual tools such as a picture of the hip flexor muscle can be invaluable. These illustrations reveal the complex interplay between bones, tendons, and musculature involved in hip flexion. Seeing how the psoas major originates from the lumbar spine and inserts into the femur helps contextualize the biomechanical demands placed on this area.
Such images are especially helpful in identifying dysfunctional movement patterns. For instance, individuals experiencing hip flexor pain when walking can observe how altered joint positioning or muscle imbalance disrupts efficient stride mechanics. Visual aids also enhance client education, improving adherence to rehabilitation protocols by fostering anatomical literacy and body awareness.
Educational platforms and fitness professionals can incorporate these visuals into their instruction to guide clients through safe, effective movement. The increased accessibility of anatomical apps and virtual training tools has made it easier than ever to personalize rehabilitation based on visual feedback. Understanding the picture of hip flexor muscle function transforms abstract concepts into practical strategies for healing.

Mobility Flow Design: Building Effective Daily Routines
Creating a personalized mobility flow that incorporates stretching, joint mobilization, and dynamic movement is a powerful way to reinforce hip health. Rather than relying on static stretches alone, mobility flows incorporate multi-joint patterns that challenge balance, coordination, and range of motion. A typical flow might begin with diaphragmatic breathing, transition into dynamic stretches like leg swings or lunge reaches, and conclude with isometric holds or resistance-based exercises.
Mobility flows can be performed as warm-ups before training or as standalone recovery sessions. For individuals dealing with hip flexor pain while sitting or standing, integrating such routines into daily life enhances circulation and joint lubrication. Flows that include 90/90 transitions, deep squat holds, and hip CARs (controlled articular rotations) improve hip capsule health and neuromuscular control.
Consistency is the key to progress. Performing even a short 10-minute flow each morning or evening can yield noticeable improvements in mobility and pain reduction. These routines also foster mindfulness, helping individuals stay attuned to bodily signals and adjust their movement patterns accordingly.
Leveraging Technology for Recovery Monitoring and Optimization
Technology has revolutionized rehabilitation by providing tools to track progress, ensure proper technique, and personalize interventions. Wearable devices like accelerometers and EMG sensors can measure hip joint angles, muscle activation patterns, and gait asymmetries. These data points allow clinicians to fine-tune programs and patients to visualize improvements over time.
Apps such as ROM Coach, Keelo, and PhysiApp offer video-guided rehabilitation plans that integrate hip flexor treatment with full-body conditioning. Many platforms include pain tracking, session reminders, and feedback loops that support adherence. Virtual reality (VR) and augmented reality (AR) are emerging as immersive tools for motor retraining and proprioceptive enhancement.
For those managing chronic conditions or returning to sport, remote coaching and telehealth physical therapy offer convenience without sacrificing effectiveness. With proper guidance, patients can safely perform advanced techniques like progressive overload, velocity-based training, or manual therapy with self-applied tools. Technology serves as both a motivator and a diagnostic aid, accelerating recovery and minimizing risk.
Psychological Resilience and the Mind-Body Connection in Injury Recovery
Physical pain is not solely a mechanical issue—psychological and emotional factors often influence the experience and duration of symptoms. Fear-avoidance behavior, in which individuals limit movement to avoid perceived harm, can perpetuate dysfunction and hinder progress. Addressing these barriers through education, reassurance, and cognitive-behavioral strategies is essential for holistic healing.
Mindfulness practices, including body scans, breath awareness, and progressive relaxation, reduce muscle tension and improve interoception. This heightened body awareness enhances motor control and reduces involuntary guarding, especially in cases of chronic hip flexor pain when walking or transitioning positions. Incorporating guided meditation into rehabilitation routines also supports mental well-being and fosters resilience.
Narrative therapy and journaling can help individuals reframe their experience of injury, shifting from a mindset of limitation to one of empowerment. Celebrating small wins, visualizing recovery milestones, and cultivating self-efficacy improve adherence and outlook. As the body heals, so too can the mind, creating a synergistic effect that reinforces long-term success.
What to Do for a Hurt Hip Flexor: Integrating Recovery into Daily Life
Learning what to do for a hurt hip flexor involves more than isolated stretches and exercises. It requires a lifestyle-oriented approach that incorporates recovery into daily routines. Active recovery practices such as walking, low-impact cardio, and gentle yoga promote circulation and prevent stiffness. These activities also support mental well-being, which is closely tied to physical healing.
Applying heat therapy in the subacute stages of injury can enhance blood flow and facilitate muscle relaxation. Sleep hygiene is another crucial yet often overlooked component of recovery. Since muscle regeneration occurs during deep sleep, maintaining consistent sleep routines aids in the repair of strained tissue. Hydration and balanced nutrition further support cellular repair and inflammation management.
For those wondering how to help hip flexor strain without exacerbating it, the answer lies in progressive loading and mindfulness. Avoiding high-intensity activity too soon is key to preventing reinjury. Instead, gradually reintroducing movement while observing the body’s response ensures a steady and sustainable return to function. Journaling symptoms and progress can also guide adjustments to the rehabilitation plan as needed.
Advanced Recovery Tools and Adjunctive Therapies
In addition to traditional rehabilitation strategies, several adjunctive therapies have shown promise in accelerating tissue healing and reducing pain. Blood flow restriction (BFR) training, for example, allows individuals to build strength at lower loads by partially occluding venous return during exercise. This technique stimulates hypertrophy and hormonal responses that benefit muscle repair.
Dry needling and acupuncture can relieve trigger points in the hip flexor region, especially when manual therapy or stretching is insufficient. These methods modulate pain pathways and promote circulation, offering relief in stubborn cases. Similarly, modalities like electrical stimulation (e.g., TENS or NMES) provide neuromodulation and muscle re-education benefits.
Infrared therapy, pulsed electromagnetic field (PEMF) therapy, and cryotherapy chambers represent emerging technologies with growing support. These interventions reduce inflammation, improve mitochondrial function, and support cellular recovery. While not substitutes for movement-based rehab, they offer valuable support in comprehensive treatment plans.
Frequently Asked Questions: Expert Insights on Hip Flexor Pain, Stretching, and Recovery
1. Why does hip flexor pain often return even after initial treatment seems successful?
Recurrent hip flexor pain usually stems from unaddressed neuromuscular imbalances or compensatory movement patterns that persist after the pain subsides. While early-stage hip flexor treatment often focuses on rest and basic mobility work, long-term relief requires a comprehensive approach. If your rehabilitation doesn’t correct underlying issues such as poor pelvic alignment, weak glutes, or restricted hip flexion, the strain on the hip flexor muscles can resurface. A common oversight is neglecting eccentric strength training, which helps condition the muscles for deceleration and control. For those seeking how to fix hip flexor pain permanently, including advanced stabilization and proprioceptive drills may be essential to maintain results.
2. How does prolonged stress impact hip flexor muscle tension?
Chronic stress can lead to persistent muscle tension, particularly in the psoas, one of the core hip flexor muscles. The psoas connects the spine to the femur and has a strong fascial and neurological link with the diaphragm. When the body remains in a fight-or-flight state, hip flexor tension can build subtly over time, leading to sore hip flexors even without high physical exertion. Addressing symptoms of tight hip flexors in this context requires stress management techniques like breathwork, yoga, and parasympathetic-focused nervous system regulation. A holistic hip flexor treatment strategy should also include emotional and psychological support to prevent somatic tension buildup.
3. Are there occupational factors that worsen hip flexor pain when sitting or standing?
Yes, ergonomics and occupational habits significantly affect hip flexor health. Sedentary jobs or those involving extended driving lead to hip flexor pain when sitting, while jobs requiring repetitive lifting may contribute to pain in the hip flexor when lifting leg rehab protocols are needed. Inadequate lumbar support, high chairs, or frequent twisting can also lead to chronic shortening of the hip flexor muscles. Making small adjustments like incorporating standing desks, optimizing hip alignment with proper seating, and regularly changing positions can help alleviate hip flexor pain when walking or standing. Occupational therapists often recommend micro-movement routines for those who suffer from hip flexor pain while sitting for long hours.
4. How can I tell if nerve entrapment is contributing to my hip flexor symptoms?
Nerve entrapment, particularly of the femoral nerve, can mimic or exacerbate symptoms of tight hip flexors. If your discomfort includes burning, tingling, or radiating pain beyond the hip into the groin or thigh, nerve involvement may be present. Unlike muscular pain, nerve-related discomfort is often worsened by prolonged stretching or compression, such as during deep lunges or extended sitting. In these cases, how to alleviate hip flexor pain might include nerve flossing techniques rather than aggressive stretching. A picture of the hip flexor muscle’s proximity to nerves can clarify how entrapment occurs, and a physical therapist can perform clinical assessments to confirm involvement.
5. What role does hydration play in preventing hip flexor muscle strain treatment recurrence?
Hydration plays a critical yet often underestimated role in muscle elasticity, fascial glide, and tissue recovery. Dehydrated muscle fibers and fascia are more prone to micro-tearing, which can hinder how to heal a hip flexor strain effectively. Even mild dehydration can increase susceptibility to cramps, delayed onset soreness, and reduced flexibility. When devising a strategy for how to treat strained hip flexor injuries, maintaining optimal hydration levels should be part of the plan. Including electrolyte balance alongside water intake supports cellular repair and can reduce the incidence of sore hip flexors after exercise or static positions.
6. How does age influence hip flexor treatment and recovery protocols?
Age-related changes in connective tissue elasticity, muscle mass, and neuromuscular control can influence both the presentation and recovery from hip flexor injuries. Older adults may experience more severe hip flexor pain when walking or transitioning from sitting to standing due to reduced joint lubrication and sarcopenia. How to fix a hip flexor injury in this population often requires lower-load, higher-repetition strength work combined with balance training and fall prevention strategies. Additionally, chronic hip flexor pain treatment in aging populations should account for bone density, comorbidities like arthritis, and slower tissue regeneration rates. Personalized care from a physiotherapist familiar with geriatric exercise science can make recovery more efficient.
7. Can footwear affect symptoms of tight hip flexors or hip flexor pain when walking?
Absolutely. Footwear alters ground reaction forces, gait mechanics, and pelvic stability, all of which influence hip function. Wearing high heels or poorly cushioned shoes can tilt the pelvis anteriorly, increasing the activation demand on the hip flexor muscles. This can lead to overuse, especially in those prone to symptoms of tight hip flexors or recurring pain in hip flexor when lifting leg rehab is underway. Flat, flexible shoes with good arch support help restore natural hip flexion mechanics and reduce undue strain. As part of a comprehensive approach to how to treat hip flexor pain, evaluating your walking and running shoes may offer a surprising improvement in symptoms.
8. What should I do when I injure my hip flexor during sport but don’t feel pain until later?
Delayed onset of pain is common in minor hip flexor strains, especially during dynamic sports where adrenaline masks discomfort. If you suspect injury due to tightness, instability, or loss of range of motion, initiate early-phase hip flexor muscle strain treatment even in the absence of severe pain. Ice application, isometric holds, and rest from high-intensity activity can prevent worsening. Many athletes delay seeking care, leading to chronic hip flexor pain treatment being required weeks later. Understanding what to do for a hurt hip flexor in the hours following trauma can minimize downtime and support a smoother rehabilitation journey.
9. Why does running sometimes aggravate my hip flexor more than weightlifting?
Running places cyclical, high-repetition demand on the hip flexor muscles, especially during the swing phase of the gait cycle. In contrast, weightlifting movements like squats or deadlifts emphasize the posterior chain and involve more static hip flexion positions rather than dynamic hip flexor loading. Therefore, running hip flexor pain is often linked to poor gait mechanics, inadequate warm-up, or overtraining. How to help hip flexor strain in this context may involve stride re-education, cadence adjustments, and post-run recovery work like foam rolling. Runners frequently benefit from alternating terrain, varying training volume, and incorporating cross-training to reduce repetitive stress.
10. Is imaging necessary to diagnose a hip flexor injury or is clinical assessment enough?
In most cases, a detailed clinical assessment by a licensed physical therapist or sports medicine professional is sufficient to identify hip flexor injuries. Manual muscle tests, palpation, and movement analysis can reveal whether hip flexion mechanics are impaired or if specific hip flexor muscles are overactive. However, when symptoms persist despite conservative care, imaging like ultrasound or MRI can help rule out complex issues such as labral tears, tendinopathy, or avulsion fractures. If you’re unsure where your hip flexor pain originates or if you’re questioning how to heal a hurt hip flexor with limited progress, advanced diagnostics may offer the clarity needed to refine your plan.
Conclusion: Reclaiming Mobility and Comfort Through Hip Flexor Treatment
Reclaiming comfort and mobility starts with understanding the complex role of the hip flexor muscles in daily movement. Whether you’re facing hip flexor pain when sitting, tightness during walking, or soreness after activity, expert-backed mobility work can offer a viable path toward healing. From recognizing the symptoms of tight hip flexors to applying targeted stretching and strength training, the journey to recovery is both proactive and empowering.
By learning how to fix hip flexor pain through structured rehabilitation, individuals can restore function and prevent recurrence. The integration of postural awareness, ergonomic strategies, and holistic recovery habits forms a complete framework for lasting results. Whether addressing acute strain or seeking chronic hip flexor pain treatment, consistency and informed action are the keys to sustainable progress.
Ultimately, knowing how to treat hip flexor pain equips you not only to alleviate current discomfort but to prevent future issues. Empowered by knowledge and guided by evidence-based practices, you can confidently take charge of your health and movement. From stretching routines to strength drills, each step taken toward recovery brings you closer to freedom of movement and a more active, pain-free life.


