The human body is a deeply interconnected system, and nowhere is this more apparent than in the communication between the brain and the gut. Often called the “second brain,” the gastrointestinal system houses a vast network of neurons and is profoundly influenced by emotional and psychological states. In recent years, researchers have turned a spotlight on the intimate connection between mental stress and digestive health. As more people grapple with chronic stress and gastrointestinal issues, understanding how stress disrupts digestion has become a public health imperative. This exploration delves into the scientific underpinnings of stress and gut health, revealing how the mind-body relationship can shape digestive outcomes and overall well-being.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
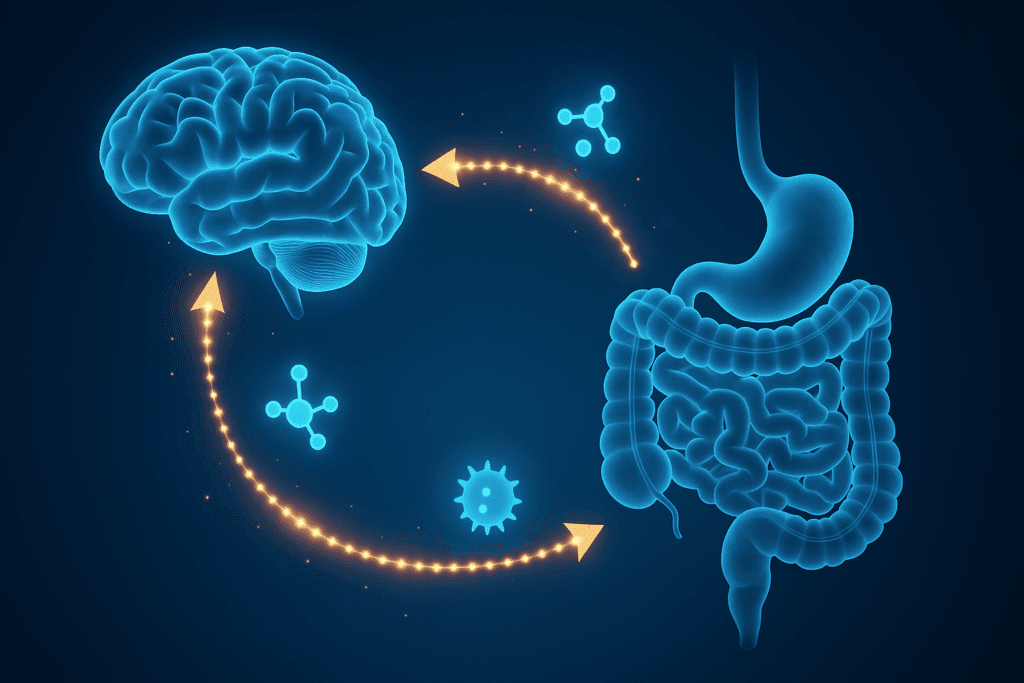
The Gut-Brain Axis: A Two-Way Street of Communication
Central to the relationship between stress and gut health is the gut-brain axis, a bidirectional communication pathway linking the central nervous system (CNS) with the enteric nervous system (ENS). This pathway facilitates the exchange of chemical signals, including hormones, neurotransmitters, and immune modulators. The gut-brain axis plays a vital role in regulating digestion, absorption, immune function, and even mood.
When a person experiences psychological stress, the brain activates the hypothalamic-pituitary-adrenal (HPA) axis, which floods the body with stress hormones such as cortisol and adrenaline. These hormones are not restricted to affecting only mood or energy levels; they also influence gastrointestinal function. Increased cortisol levels can alter gut motility, reduce mucosal blood flow, and impair the gut’s protective barrier. Consequently, what begins as a mental or emotional response can manifest physically, leading to symptoms like bloating, cramping, and altered bowel habits. This dynamic helps illuminate how stress affects the digestive system and why individuals under chronic stress often experience persistent gastrointestinal distress.
The Role of the Autonomic Nervous System in Digestive Function
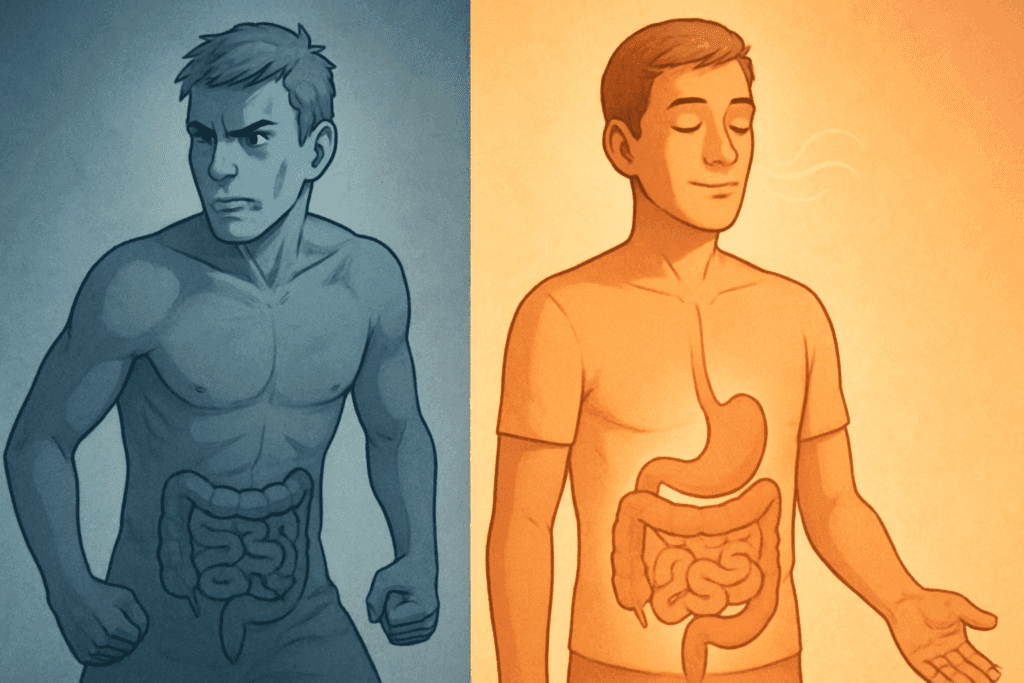
The autonomic nervous system (ANS), which regulates involuntary bodily functions, is intricately involved in digestion. It comprises two major branches: the sympathetic nervous system (SNS), responsible for the ‘fight or flight’ response, and the parasympathetic nervous system (PNS), often called the ‘rest and digest’ system. In a state of calm, the PNS promotes optimal digestion by enhancing gastric secretions, enzyme activity, and intestinal motility.
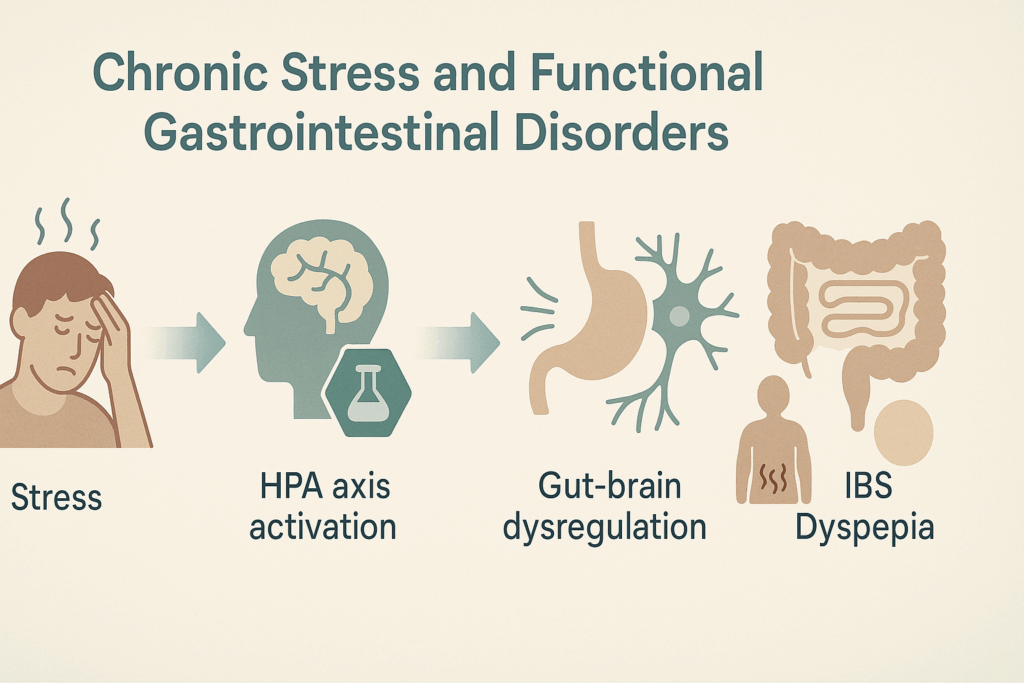
However, during periods of stress, the SNS becomes dominant, prioritizing survival responses over digestion. This shift leads to reduced blood flow to the gut, suppression of digestive enzymes, and decreased peristalsis. It becomes evident that what is responsible for slowing digestion in the nervous system is the chronic activation of the sympathetic branch. This physiological response, while adaptive in short bursts, can become maladaptive when prolonged. In the context of chronic stress, digestion is continuously compromised, often contributing to functional gastrointestinal disorders such as irritable bowel syndrome (IBS), functional dyspepsia, and even acid reflux. Understanding the role of the autonomic nervous system in this disruption underscores how stress affects the digestive system on both structural and biochemical levels.
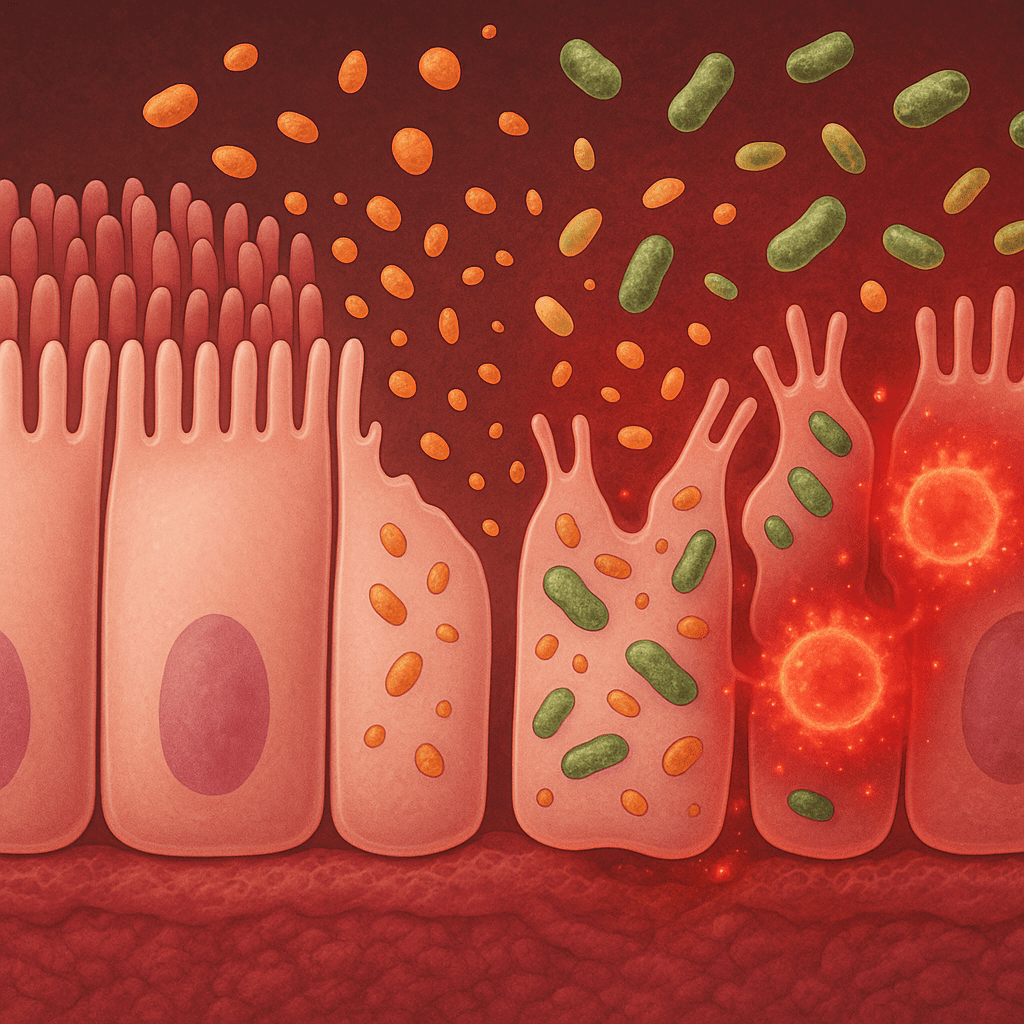
Cortisol and Gut Integrity: Breaking Down the Protective Barrier
One of the most significant ways stress impairs digestive function is through the impact of cortisol on gut permeability. Under normal conditions, the gut lining acts as a selective barrier, allowing nutrients to pass into the bloodstream while keeping harmful substances out. Stress-induced cortisol release can weaken this barrier, leading to a condition known as increased intestinal permeability, or “leaky gut.”
When the integrity of the gut lining is compromised, larger molecules such as toxins, bacteria, and undigested food particles can pass through into the bloodstream, triggering systemic inflammation. This not only exacerbates digestive issues but may also contribute to autoimmune reactions and food sensitivities. The breakdown of this barrier further illustrates how stress affects the digestive system by creating a cascade of immune and inflammatory responses. Researchers have found correlations between chronic stress and elevated markers of inflammation in both the gut and other body systems. These findings point to the broader systemic effects that begin with stress and gut health disruption.
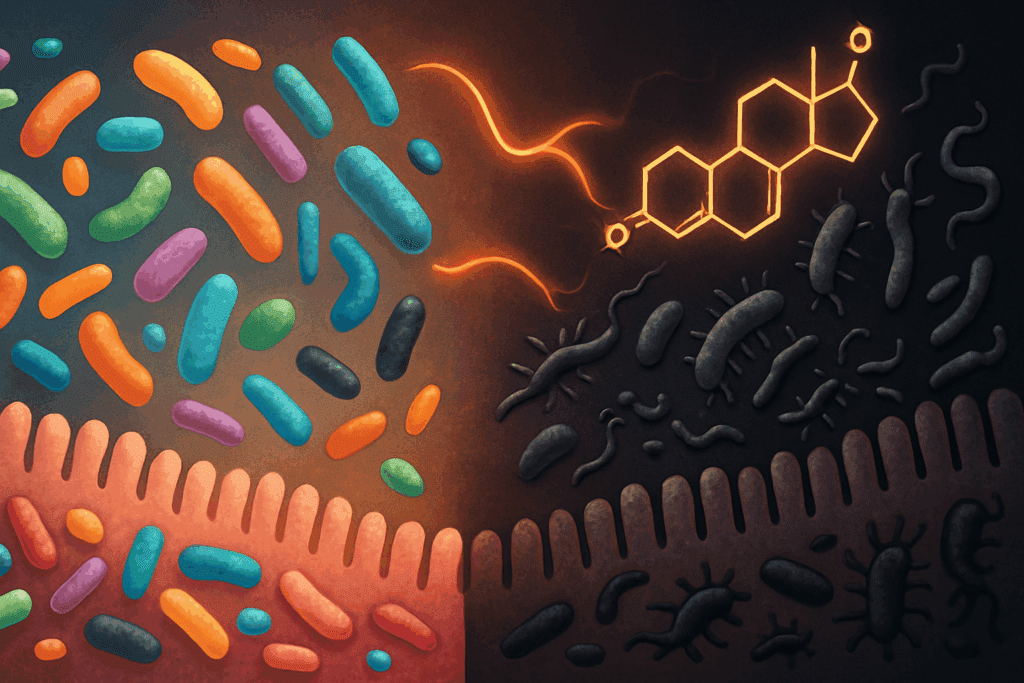
Stress, Gut Microbiota, and Dysbiosis
An often overlooked but critical component of gut health is the community of trillions of microbes that inhabit the gastrointestinal tract. These microorganisms, collectively referred to as the gut microbiota, are responsible for a host of vital functions, including digestion, vitamin synthesis, immune modulation, and mood regulation through neurotransmitter production. However, the delicate balance of the microbiota can be disturbed by psychological stress.
Stress has been shown to reduce microbial diversity and alter the composition of the gut flora, leading to a condition known as dysbiosis. Dysbiosis can impair digestion, weaken immune defenses, and increase susceptibility to infections. In animal and human studies, stress-induced dysbiosis has been linked to anxiety, depression, and exacerbation of digestive conditions such as inflammatory bowel disease (IBD). These findings reinforce the idea that stress and gut health are inseparably linked, with microbiome imbalances serving as both a consequence and contributor to digestive dysfunction. The use of probiotics, dietary interventions, and stress-reduction strategies has emerged as a promising approach to restore microbial balance and improve digestive outcomes.
Chronic Stress and Functional Gastrointestinal Disorders
Functional gastrointestinal disorders (FGIDs) represent a category of digestive conditions in which symptoms occur without identifiable structural or biochemical abnormalities. Among the most common FGIDs are IBS, functional dyspepsia, and cyclic vomiting syndrome. These disorders are frequently associated with heightened stress responses and dysregulation of the gut-brain axis.
IBS, for example, is characterized by abdominal pain, bloating, and altered bowel habits, often exacerbated by stress. Clinical studies have shown that patients with IBS have increased activation of the HPA axis and greater sensitivity to visceral pain. The question of how stress affects the digestive system is central to understanding FGIDs, as treatment often involves psychological as well as physiological interventions. Cognitive behavioral therapy (CBT), gut-directed hypnotherapy, and mindfulness-based stress reduction have demonstrated success in alleviating symptoms by addressing both the mental and somatic components of these disorders.
Dietary Responses to Stress and Their Digestive Consequences
Stress not only affects digestion physiologically but also influences dietary choices, which can, in turn, impact gut health. During periods of emotional stress, individuals often gravitate toward high-fat, high-sugar “comfort foods,” which can disrupt digestion and microbiome composition. These foods tend to slow gastric emptying and alter bile secretion, contributing to discomfort, bloating, and constipation.
Furthermore, stress-induced eating behaviors often lead to erratic meal timing, overeating, or undereating—all of which compromise digestive efficiency. Stress and gut health become further entangled when poor dietary patterns exacerbate inflammation and microbial imbalance. Long-term consumption of ultra-processed foods under stress can create a feedback loop in which gut discomfort reinforces emotional distress, and vice versa. A more mindful approach to eating, including regular meals, whole foods, and attention to hunger cues, can serve as a powerful intervention in breaking this cycle.
Mindfulness and Relaxation as Digestive Therapies
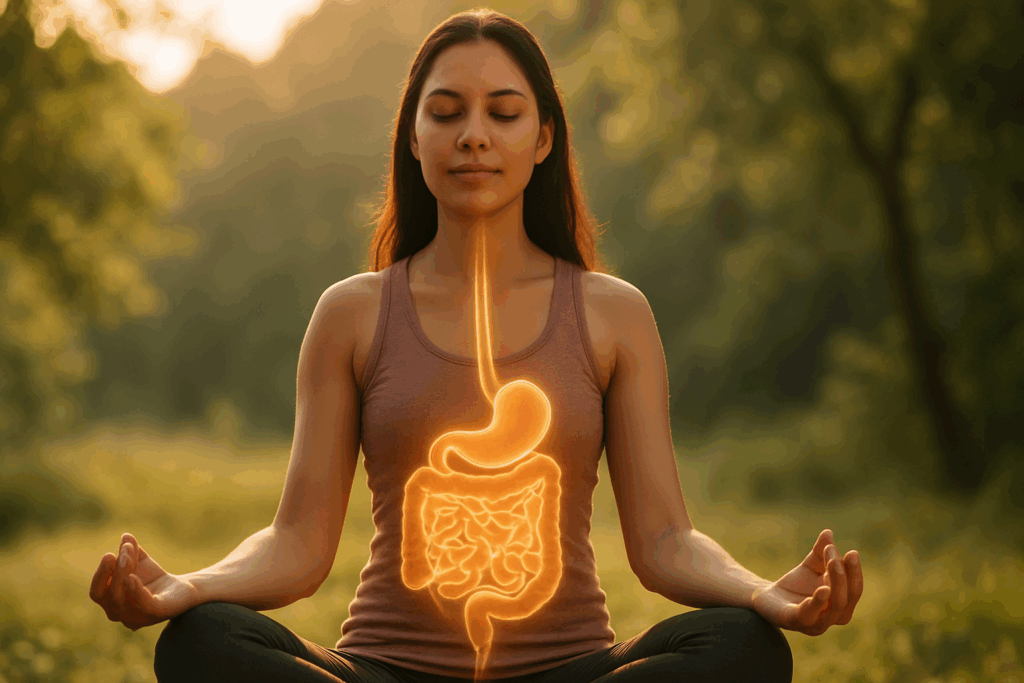
Given the profound impact of psychological states on gut function, it is no surprise that stress-reduction strategies can serve as effective treatments for digestive complaints. Mindfulness meditation, breathing exercises, progressive muscle relaxation, and yoga have all been shown to activate the parasympathetic nervous system and restore digestive function.
These practices counterbalance the ‘fight or flight’ dominance of the sympathetic nervous system, allowing the body to return to a ‘rest and digest’ state. Studies have demonstrated that regular mindfulness practice can reduce cortisol levels, improve gut motility, and alleviate symptoms in conditions such as IBS and functional dyspepsia. These outcomes not only highlight how stress affects the digestive system but also illustrate the potential for non-pharmacologic therapies to improve gut health through nervous system modulation. Incorporating even brief periods of mindfulness into daily routines can create measurable improvements in both mental and digestive well-being.
Neuroinflammation and the Vicious Cycle of Stress and Gut Dysfunction
Emerging research has begun to focus on the role of neuroinflammation in the context of stress and gut health. Chronic stress can lead to increased production of pro-inflammatory cytokines in the brain and gut, contributing to a feedback loop of worsening anxiety and digestive dysfunction. This inflammatory cascade can sensitize pain pathways, alter neurotransmitter function, and impair intestinal barrier integrity.
In turn, a distressed gut can send alarm signals back to the brain, perpetuating a cycle of emotional and physical discomfort. The involvement of neuroinflammation helps answer the question of what is responsible for slowing digestion in the nervous system during prolonged stress states. Understanding this bidirectional influence opens new avenues for therapeutic strategies targeting inflammation at both neurological and gastrointestinal levels. Anti-inflammatory diets, omega-3 fatty acids, and targeted microbial therapies are currently being explored for their potential to modulate this neuroimmune dialogue.
Integrative Approaches to Supporting Gut Health Under Stress
Addressing stress-related digestive issues often requires an integrative, multi-pronged approach. Conventional medical treatments such as antispasmodics, antacids, and laxatives may provide temporary relief, but they do not address the underlying stress-related mechanisms. A more sustainable approach includes combining pharmacologic options with lifestyle modifications, nutritional interventions, and psychological therapies.
Nutritional strategies to support gut health include increasing fiber intake, consuming fermented foods, and avoiding known dietary triggers. These adjustments help to stabilize the microbiome, reduce inflammation, and support gut barrier function. Simultaneously, stress management through therapy, exercise, and relaxation techniques plays a crucial role in breaking the stress-digestion cycle. As evidence continues to mount, healthcare practitioners are increasingly recognizing the importance of assessing stress and gut health together, rather than treating them as isolated concerns.
The Role of Sleep in Digestive Resilience
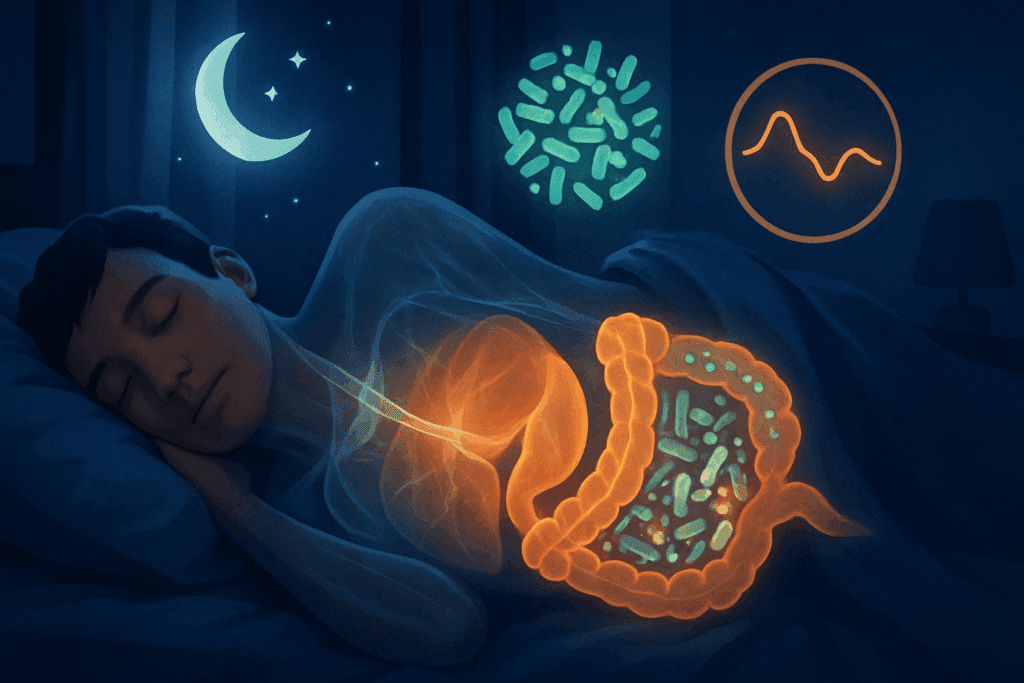
Sleep is often the missing piece in discussions about stress and gut health. Chronic sleep deprivation exacerbates both psychological stress and digestive imbalance. Poor sleep quality has been linked to altered gut microbiota, increased intestinal permeability, and heightened sensitivity to digestive discomfort. Moreover, disrupted sleep negatively impacts the body’s ability to regulate cortisol, leading to prolonged stress responses and impaired parasympathetic activation.
Improving sleep hygiene, such as maintaining a consistent bedtime, reducing screen exposure before bed, and avoiding caffeine late in the day, can contribute to healthier digestive rhythms. When individuals prioritize rest, they support the body’s ability to recover from stress and restore digestive function. This demonstrates yet another layer in how stress affects the digestive system, underscoring the need for holistic attention to daily routines.
Frequently Asked Questions: How Stress Disrupts Digestion and Impacts Gut Health
1. Can stress-related digestive problems lead to long-term health consequences?
Yes, chronic stress-related digestive issues can have long-term health implications that go well beyond temporary discomfort. Prolonged dysregulation of the gut-brain axis may contribute to inflammation, immune dysfunction, and nutritional deficiencies. When examining how stress affects the digestive system, researchers have observed that long-term stress can alter nutrient absorption and contribute to conditions such as irritable bowel syndrome, ulcers, and even metabolic disturbances. These chronic disruptions may, in some cases, increase the risk of autoimmune responses or chronic inflammatory diseases due to persistent gut barrier breakdown. Addressing stress early is essential to protecting not only digestive health but also systemic wellness over time.
2. Are certain personalities more prone to stress-induced digestive issues?
Personality traits appear to influence how individuals experience and respond to stress, which can directly impact gastrointestinal health. People with high neuroticism, perfectionism, or chronic anxiety often exhibit heightened physiological responses to stressors, which may explain why stress and gut health are closely linked in this group. Studies suggest that individuals who ruminate or have difficulty emotionally regulating are more likely to experience gut-related symptoms under stress. Understanding how stress affects the digestive system from a psychosocial perspective highlights the importance of cognitive-behavioral strategies and resilience-building therapies. Tailoring interventions to personality types may be an emerging avenue for personalized gut-brain treatment plans.
3. How do workplace stressors specifically affect digestion?
Occupational stress is one of the most pervasive and underestimated contributors to digestive dysfunction. High-demand, low-control job environments have been strongly correlated with gastrointestinal complaints, including bloating, indigestion, and irregular bowel movements. A key factor in what is responsible for slowing digestion in the nervous system is the repeated activation of the sympathetic response during work-related pressure or conflict. Workplace stress often leads to irregular eating schedules, overconsumption of processed foods, and reduced time for rest or physical activity, all of which impair gut function. Introducing wellness programs and flexible break schedules can help mitigate these effects by giving the parasympathetic system more opportunity to facilitate digestion.
4. How does social isolation interact with stress to worsen digestive issues?
Social isolation can intensify stress and disrupt gut health in complex ways. Individuals who lack meaningful social support are more vulnerable to prolonged stress, which affects both emotional regulation and physiological function. The gut microbiome may also be influenced by social factors, as studies in both animals and humans show that isolation can reduce microbial diversity. This interaction provides further insight into how stress affects the digestive system through psychological and biological channels. Strengthening social bonds and community engagement may offer protective benefits for gut health, making social connection a surprisingly important component of digestive care.
5. Are there emerging technologies or therapies targeting the stress-digestion link?
New tools are emerging that aim to modulate the gut-brain axis using cutting-edge technology. One example is vagus nerve stimulation (VNS), which uses electrical impulses to enhance parasympathetic tone and improve digestive function. Digital therapeutics, including app-based biofeedback and virtual reality mindfulness interventions, are also showing promise in reducing the impact of stress and gut health dysfunction. Functional gastrointestinal monitoring via wearable biosensors may soon provide real-time feedback on how stress affects the digestive system. As these innovations evolve, they may transform how clinicians assess and manage stress-related digestive concerns with greater precision.
6. How does early-life stress influence digestion later in life?
Experiences of stress in childhood, including trauma or instability, can leave lasting imprints on the gut-brain axis. Early exposure to chronic stress may alter neuroendocrine signaling and microbial development during critical periods of gastrointestinal maturation. These changes can create a lifelong vulnerability to disorders where stress and gut health are intertwined, such as functional bowel syndromes or inflammatory gut conditions. Researchers continue to explore how early stress might permanently recalibrate what is responsible for slowing digestion in the nervous system later in life. Intervening early with trauma-informed care could therefore reduce the risk of future digestive dysfunction.
7. What role does gender play in stress-related digestive disorders?
Gender appears to modulate the interaction between stress and gastrointestinal function. Women are disproportionately affected by conditions like IBS, and research suggests this may be due to hormonal fluctuations and differences in pain perception and immune response. Estrogen and progesterone can influence gut motility and microbial composition, potentially intensifying the effects of stress on digestion. Gendered social roles and stress exposure may further shape how stress affects the digestive system, particularly when emotional labor and caregiving responsibilities are unequally distributed. Gender-sensitive approaches to both psychological and gastrointestinal care are critical for improving outcomes in stress-related disorders.
8. Can certain breathing techniques or movement practices improve digestion under stress?
Yes, specific physical practices like diaphragmatic breathing, Tai Chi, and gentle yoga can significantly enhance parasympathetic nervous system activity, aiding digestion. These practices help shift the autonomic balance away from the sympathetic state that is primarily what is responsible for slowing digestion in the nervous system. Controlled breathing not only reduces perceived stress but also stimulates the vagus nerve, which supports gastric secretion and intestinal movement. Integrating mindful movement into daily routines can offer immediate and long-term digestive benefits. These techniques are particularly useful for individuals who struggle with medication side effects or prefer non-pharmacological interventions.
9. How do seasonal changes in mood and stress levels affect digestion?
Shifts in daylight, temperature, and routine throughout the year can significantly affect both stress levels and gut function. Seasonal affective disorder (SAD) and reduced sunlight exposure are associated with increased cortisol production and changes in serotonin levels, which can influence the gastrointestinal tract. This cyclical fluctuation reveals how stress affects the digestive system not only during major life events but also through subtle environmental shifts. Seasonal patterns in gut microbiota composition have also been observed, which may further explain digestion variability. Addressing seasonal stressors through light therapy, dietary adjustments, and exercise can help preserve digestive resilience year-round.
10. Are there preventive strategies to protect the gut before stress becomes chronic?
Proactive care is essential to prevent long-term disruption in the gut-brain axis. This involves not only stress management techniques but also preemptive support for microbial health through prebiotics, fermented foods, and a fiber-rich diet. Regular physical activity, adequate hydration, and consistent sleep routines all help buffer the body from the worst effects of chronic stress. Understanding what is responsible for slowing digestion in the nervous system allows individuals to make informed lifestyle changes before symptoms appear. Preventive strategies serve as a frontline defense in maintaining the complex balance between stress and gut health over time.
Conclusion: Building Digestive Resilience by Managing Stress
The intricate relationship between stress and digestion reveals the remarkable sensitivity of the gut to emotional and psychological influences. From neurohormonal pathways to microbial composition and inflammatory responses, the gut mirrors the mind in more ways than previously understood. Understanding how stress affects the digestive system is essential for both clinicians and individuals seeking lasting relief from chronic gastrointestinal symptoms.
What is responsible for slowing digestion in the nervous system often comes down to the dominance of the sympathetic response during prolonged stress. Meanwhile, the disruption of gut microbiota, mucosal integrity, and enzyme function highlights the cascading impact of psychological stress on digestive efficiency. By recognizing the multifaceted nature of stress and gut health, we can begin to develop comprehensive, integrative strategies that address both the root cause and the symptoms.
Restoring digestive health in the context of stress involves more than medication; it requires an active commitment to mental well-being, mindful eating, quality sleep, and lifestyle balance. As we deepen our understanding of the gut-brain connection, we gain not only insight into human physiology but also practical tools for cultivating resilience in both mind and body. In doing so, we empower ourselves to navigate life’s stresses without sacrificing our most essential systems of nourishment and vitality.
gut-brain connection, chronic stress symptoms, nervous system and digestion, vagus nerve function, digestive health tips, intestinal permeability, leaky gut causes, gut inflammation and anxiety, microbiome and mental health, cortisol and digestion, digestive enzyme suppression, autonomic imbalance, parasympathetic activation, irritable bowel triggers, functional gut disorders, holistic digestive care, gastrointestinal stress response, neuroendocrine gut axis, mental health and digestion, natural ways to improve digestion
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out
Further Reading:
How Stress Impacts Your Digestion – And How to Fix It
Gut-Brain Connection: Discover How Stress Affects Digestion
Digestive Disorders Unveiled: The Role of Stress
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.


