Hip tendonitis can be a debilitating condition, particularly for active individuals or those who rely on physical mobility for daily tasks and athletic performance. The discomfort associated with hip tendonitis not only limits movement but can also interfere with quality of life and long-term musculoskeletal health. Fortunately, early intervention with targeted hip tendonitis stretches and carefully designed hip tendonitis rehab exercises can significantly reduce pain, improve flexibility, and restore full function. This article explores the most effective, evidence-based approaches for addressing hip tendonitis through movement therapy, while applying medically accurate insights rooted in the principles of physical therapy and rehabilitation science.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Understanding Hip Tendonitis: Causes and Symptoms
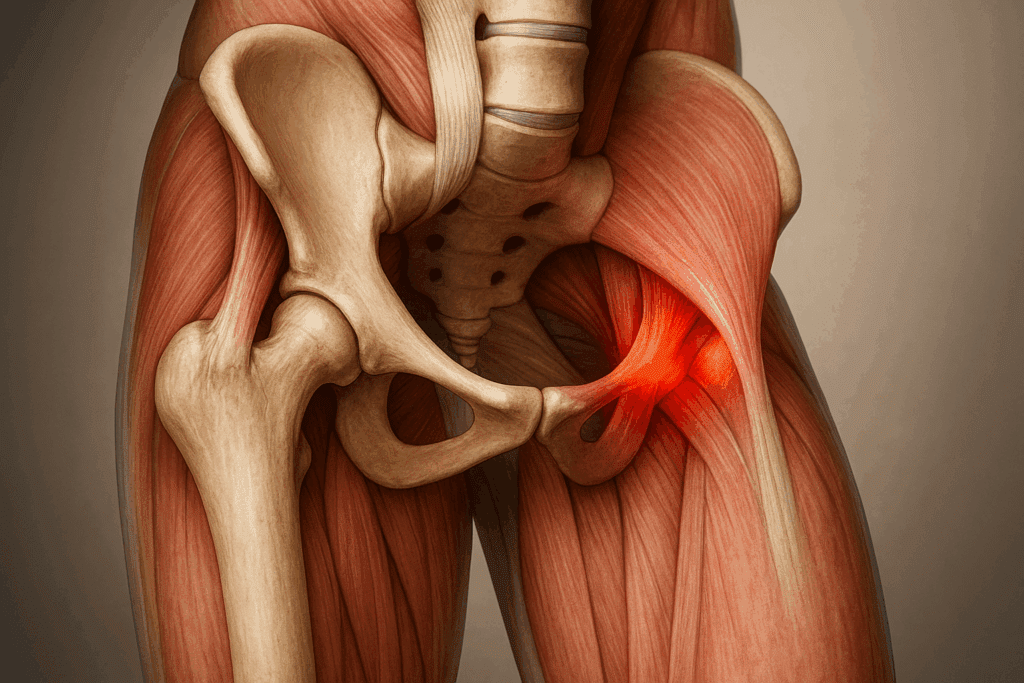
Hip tendonitis refers to the inflammation or irritation of the tendons that connect muscles to the hip bones, most commonly affecting the iliopsoas, gluteal, or adductor tendons. This condition often arises from repetitive strain, overuse, biomechanical imbalances, or inadequate recovery after exercise. Individuals who engage in high-impact sports, such as running, soccer, or dancing, are particularly susceptible. However, sedentary lifestyles marked by prolonged sitting can also contribute to tendon dysfunction due to muscular shortening and joint stiffness.
The symptoms of hip tendonitis typically include a dull, aching pain located deep within the groin or outer hip area, which may worsen with movement, especially when lifting the leg, climbing stairs, or engaging in hip-flexion activities. Swelling, tenderness to touch, and restricted range of motion are also common. Left unaddressed, chronic hip tendonitis can lead to tendon degeneration, further mobility issues, and even compensatory injuries in the knees, lower back, or opposite hip.
Understanding Muscle Synergies and Kinetic Chain Interplay
One of the most overlooked components in hip tendonitis recovery is the interaction between muscle groups, particularly how compensations from the surrounding musculature can affect healing. While stretching and strengthening are essential, understanding muscle synergies—how groups of muscles work together to produce movement—is key to preventing re-injury.
For instance, when the hip flexors become inflamed or weak due to tendonitis, other structures like the lumbar spine, hamstrings, and contralateral hip muscles may take over. This compensatory behavior creates dysfunctional movement patterns that often go unnoticed until they become sources of new pain or mechanical strain. Targeting muscle groups like the quadratus lumborum or the deep rotators of the hip can improve the overall biomechanical environment, reducing stress on the inflamed tendon.
Furthermore, evaluating the kinetic chain from the ground up helps identify weaknesses or misalignments in the feet, ankles, knees, and pelvis that influence hip function. Corrective exercises addressing foot pronation or knee valgus, for example, can indirectly reduce tendon loading in the hip and facilitate a smoother recovery.

The Role of Pelvic Stability and Core Conditioning
An often-underemphasized element in hip tendonitis rehab exercises is the importance of pelvic stability. The pelvis serves as the foundational base for hip function, and instability here can undermine even the most precise rehab routines. Engaging the core muscles—especially the transverse abdominis, obliques, and multifidus—improves load distribution and prevents compensatory strain on the hip tendons.
Incorporating exercises such as dead bugs, bird-dogs, and modified planks into a rehab program can create dynamic stability that supports functional movement. These exercises train the neuromuscular system to engage the right muscles at the right time, which is critical for maintaining hip alignment during walking, lifting, or transitioning between positions.
Core activation also supports respiratory efficiency and spinal posture, both of which influence the body’s ability to perform hip tendonitis stretches with proper form. A weak or disengaged core often leads to poor biomechanics that can stall progress and exacerbate symptoms.
The Psychological and Neurological Dimensions of Recovery
Chronic hip tendonitis can affect more than just the body; it can also influence mental well-being and neurological function. Pain perception is modulated by the central nervous system, and persistent pain can lead to heightened sensitivity, a condition known as central sensitization. Understanding this neurological mechanism allows for more compassionate and effective care.
Practices such as progressive muscle relaxation (PMR), meditation, and biofeedback help reduce sympathetic nervous system overactivity and promote parasympathetic healing states. Neuroplasticity, the brain’s ability to rewire pain responses, can be harnessed through cognitive-behavioral therapy (CBT), visualization exercises, and consistent physical activity performed without fear.
Movement confidence—the belief that the body is capable of safe, pain-free motion—has a significant impact on outcomes. Building this confidence through gradual exposure and positive reinforcement creates a virtuous cycle in which recovery becomes both physical and psychological.
Adapting Hip Tendonitis Protocols for Different Populations
Not all individuals experience hip tendonitis in the same way, and tailoring interventions based on age, activity level, and health status is essential. Athletes, for example, may benefit from sport-specific rehabilitation that replicates the dynamic demands of competition. Plyometric drills, agility training, and functional movement screens help ensure that return-to-play decisions are evidence-based and safe.
Older adults, on the other hand, may require gentler approaches that prioritize joint protection, bone density, and balance. Incorporating aquatic therapy or chair-based stretches allows for reduced load on the joints while still promoting flexibility and circulation. Age-related changes in tendon elasticity and joint lubrication make warm-up and cool-down procedures particularly important in this demographic.
Individuals with systemic conditions such as diabetes or rheumatoid arthritis must be closely monitored for delayed healing or altered pain responses. Collaboration with healthcare providers ensures that interventions are compatible with broader treatment plans and medications.
Environmental and Ergonomic Considerations for Recovery
The physical environment in which rehabilitation occurs plays a subtle but important role in hip tendonitis outcomes. For example, individuals who spend extended periods sitting at a desk may benefit from ergonomic assessments and interventions. Adjusting chair height, using lumbar supports, or incorporating sit-stand desks can minimize hip compression and support better posture.
Footwear also influences hip mechanics. Supportive shoes with proper arch support and shock absorption reduce the transmission of ground reaction forces through the hip joint. In some cases, custom orthotics or heel lifts may be recommended to correct limb length discrepancies or pelvic tilt that exacerbates tendonitis.
At home, creating a space conducive to movement and stretching can foster adherence to rehabilitation routines. Simple modifications such as placing a yoga mat in a visible location, setting reminders for mobility breaks, or using stretch straps and resistance bands can promote daily engagement with therapeutic activities.
Why Stretching Matters in Hip Tendonitis Recovery
Stretching plays a critical role in hip tendonitis rehabilitation by lengthening tight muscles, enhancing joint mobility, and reducing mechanical load on the irritated tendons. A well-executed hip tendonitis stretching routine can counteract muscle imbalances that contribute to poor alignment and excessive strain. For example, tight hip flexors may pull the pelvis forward into an anterior tilt, which in turn places undue stress on the hip joint and surrounding structures.
It is essential to distinguish between passive stretching, which involves holding a muscle in an elongated position, and dynamic stretching, which involves active movement through a range of motion. Both methods have value, but for individuals in the recovery phase, static hip tendonitis stretches are often more appropriate to avoid aggravating the condition. Over time, gentle progressive stretching improves muscle elasticity, enhances circulation, and creates the optimal environment for tendon healing.

Targeted Hip Tendonitis Stretches for Pain Relief
Among the most effective hip tendonitis stretching exercises are those targeting the iliopsoas, gluteus medius, piriformis, and adductors. The kneeling hip flexor stretch, for instance, is a cornerstone of most rehabilitation protocols. In this stretch, one kneels on the affected side with the opposite foot planted in front, gently pressing the hips forward to elongate the front of the hip. This move reduces tension in the iliopsoas tendon, a common site of inflammation in hip tendonitis.
The seated figure-four stretch is another valuable option, aimed at relieving tightness in the piriformis and gluteal muscles. By sitting upright and crossing one ankle over the opposite knee, the individual gently leans forward to open the outer hip and release accumulated tension. Similarly, side-lying adductor stretches target the inner thigh, an area frequently implicated in groin-related tendonitis. Holding these stretches for 20 to 30 seconds and repeating them several times per day ensures steady improvement without exacerbating symptoms.

Designing an Effective Hip Tendonitis Rehab Exercise Program
While stretching alleviates tightness and prepares the body for movement, a comprehensive rehabilitation program must also include strengthening exercises. Hip tendonitis rehab exercises are designed to enhance muscular stability, improve neuromuscular coordination, and reduce the risk of recurrence. Effective rehab exercises focus not only on the hip joint itself but also on the core, glutes, and surrounding muscles that support pelvic alignment and load distribution.
For example, isometric exercises such as gluteal squeezes or wall sits allow the muscles to activate without dynamic joint movement, making them suitable for the early stages of recovery. These moves provide strength benefits while minimizing strain on sensitive tendons. As symptoms improve, patients can transition to isotonic movements like clamshells, leg bridges, and standing hip abductions, which introduce controlled resistance and challenge joint stabilization.
It is important that all hip tendonitis rehab exercises be performed with correct form and gradual progression. Rushing into advanced exercises without adequate foundation can backfire, leading to reinjury or chronic inflammation. A qualified physical therapist can guide individuals through the appropriate sequence and adjust intensity based on pain levels, ensuring both safety and long-term effectiveness.
The Role of Flexibility Training in Long-Term Recovery
Flexibility training, when integrated consistently into a hip tendonitis recovery plan, serves as a protective mechanism against future injuries. By improving the extensibility of muscles and connective tissues, flexibility work reduces the likelihood of mechanical overload and compensatory movement patterns. Yoga-based routines, for example, offer a gentle yet comprehensive way to address muscular imbalances while promoting mindfulness and body awareness.
Poses such as pigeon pose, low lunge, and butterfly stretch are particularly effective for targeting hip tension and restoring balance. When practiced mindfully, these poses encourage diaphragmatic breathing, which further supports nervous system regulation and relaxation. The holistic nature of yoga also complements other therapeutic approaches by addressing psychosomatic factors like stress, anxiety, and poor posture, which can subtly contribute to hip dysfunction.
Incorporating flexibility-focused hip tendonitis stretching exercises into daily routines reinforces the gains made through rehabilitation and empowers individuals to remain proactive in their recovery journey. It also fosters a positive feedback loop in which increased mobility leads to greater physical activity, which in turn enhances musculoskeletal resilience.
The Science Behind Progressive Overload in Tendon Healing
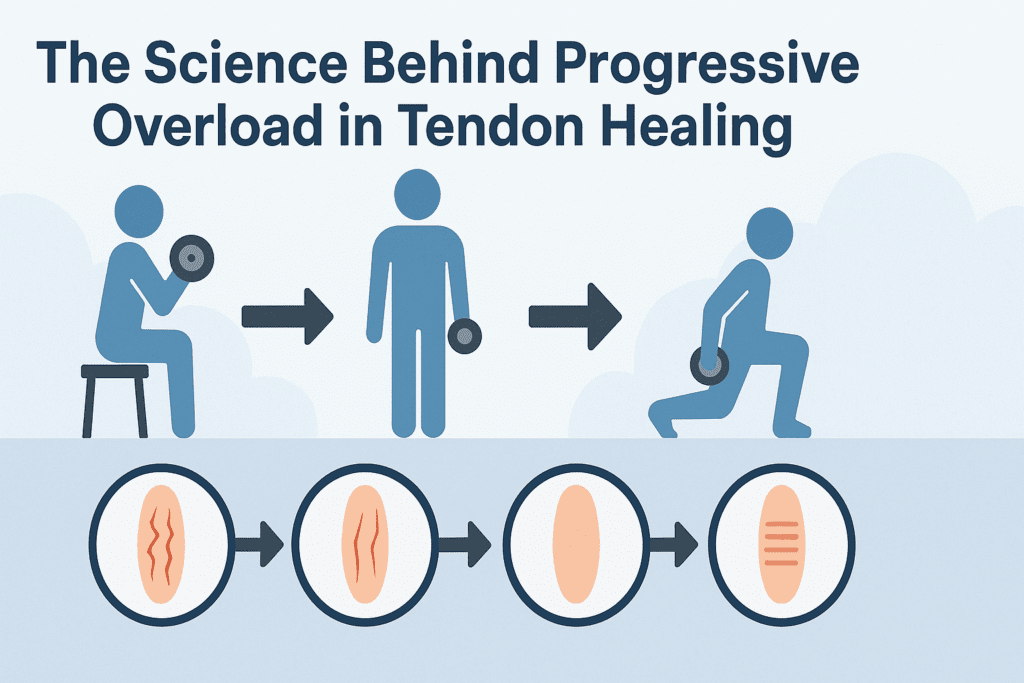
A key concept in tendon rehabilitation is progressive overload, the gradual increase in mechanical stress that stimulates tissue adaptation and repair. Unlike muscles, tendons respond more slowly to loading, requiring careful modulation of exercise intensity and frequency. In the context of hip tendonitis rehab exercises, this principle is applied by starting with low-load isometric contractions and advancing toward dynamic, weight-bearing movements as tolerated.
Research indicates that eccentric loading—in which a muscle lengthens under tension—is particularly beneficial for tendon recovery. For instance, slow, controlled lowering phases in exercises like single-leg squats or step-downs promote collagen remodeling and improve tendon tensile strength. However, these must be introduced cautiously and under professional supervision, as improper technique or premature progression can lead to setbacks.
Monitoring pain during and after exercise is essential. Mild discomfort is acceptable, but sharp or worsening pain may signal the need to modify the routine. The use of pain scales and mobility assessments can guide decision-making and ensure that the healing process stays on track without compromising tissue integrity.
Avoiding Common Pitfalls in Hip Tendonitis Rehabilitation
Despite the availability of evidence-based protocols, many individuals unknowingly make errors that hinder recovery. One common mistake is neglecting the role of rest and recovery. While movement is critical, adequate downtime between sessions allows for tendon regeneration and prevents cumulative microtrauma. Overtraining, even with the best intentions, can exacerbate symptoms and delay progress.
Another frequent oversight is focusing exclusively on the site of pain rather than addressing the kinetic chain. Poor ankle mobility, weak glutes, or core instability can all contribute to dysfunctional loading patterns that strain the hips. A holistic approach that considers the interconnectedness of the body is far more effective than isolated treatment.
Lastly, ignoring posture and daily habits can undermine the benefits of targeted hip tendonitis stretches and rehab exercises. Prolonged sitting with poor lumbar support, sleeping in asymmetrical positions, or walking with an uneven gait can all perpetuate tendon stress. Awareness of these factors, along with small lifestyle adjustments, can dramatically improve recovery outcomes.
The Psychological Component of Chronic Tendon Pain
Chronic pain, including that associated with hip tendonitis, often has a psychological dimension that influences both perception and recovery. Catastrophizing—a mental state in which pain is viewed as threatening or uncontrollable—can increase muscle tension, alter movement patterns, and reduce adherence to rehabilitation programs. Conversely, positive beliefs about recovery and confidence in one’s ability to heal have been shown to improve outcomes.
Incorporating mindfulness practices such as meditation, guided imagery, or breathwork can help modulate pain perception and enhance emotional resilience. Cognitive-behavioral therapy (CBT) techniques may also be beneficial, particularly for individuals struggling with fear-avoidance behaviors that limit movement and perpetuate dysfunction. Addressing the mental and emotional aspects of recovery reinforces the mind-body connection and supports comprehensive healing.
When to Seek Professional Help for Hip Tendonitis
While many individuals can manage mild cases of hip tendonitis through at-home strategies, there are circumstances in which professional intervention becomes necessary. Persistent pain that does not respond to conservative measures, worsening symptoms despite rest, or functional limitations that interfere with daily life all warrant medical evaluation. Imaging studies such as MRI or ultrasound may be used to assess the extent of tendon damage and rule out alternative diagnoses.
A physical therapist or sports medicine physician can develop a personalized treatment plan based on the individual’s biomechanics, lifestyle, and goals. In some cases, adjunctive therapies such as dry needling, shockwave therapy, or platelet-rich plasma (PRP) injections may be recommended to accelerate healing. Collaboration between patient and provider is key to navigating the recovery journey effectively and safely.

Using Technology to Enhance Rehabilitation Outcomes
Technological tools are increasingly available to support individuals recovering from hip tendonitis. Wearable motion sensors, for example, can track gait patterns, hip angles, and range of motion in real-time. These devices provide immediate feedback on movement quality, allowing users to adjust form and avoid harmful mechanics.
Mobile apps with guided hip tendonitis stretches and rehab exercises are also gaining popularity. Many of these platforms include instructional videos, progress tracking, and personalized alerts to ensure consistency. Virtual physical therapy sessions can offer access to expert guidance regardless of location, reducing barriers to care.
Ultrasound imaging is another valuable tool for assessing tendon health. Unlike X-rays, which only visualize bones, musculoskeletal ultrasound can detect tendon thickening, tears, or fluid accumulation. These insights guide treatment adjustments and help monitor healing progress.

Planning for Relapse Prevention and Long-Term Maintenance
Successfully overcoming hip tendonitis requires more than symptom resolution—it involves adopting habits that prevent recurrence and support long-term musculoskeletal health. Once acute pain subsides, individuals should transition from rehabilitative to maintenance protocols that include regular flexibility work, cross-training, and strength conditioning.
Cross-training with low-impact activities such as swimming, cycling, or elliptical training provides cardiovascular benefits without placing excessive stress on the hip. Including yoga or Pilates one to two times per week can help maintain muscle balance and proprioception.
Periodic reassessment by a physical therapist or movement specialist can identify emerging issues before they become problematic. These check-ins provide opportunities to refine technique, introduce new challenges, and reinforce proper mechanics.
Frequently Asked Questions: Advanced Insights on Hip Tendonitis Stretches and Rehab Exercises
1. What are some lesser-known benefits of incorporating hip tendonitis stretches into your daily routine?
While most people turn to hip tendonitis stretches to relieve pain and restore flexibility, these movements also offer a wide range of lesser-known benefits. Consistently performing targeted hip stretches can enhance proprioception, which is the body’s ability to sense its position in space. This improvement in joint awareness helps prevent future injuries, particularly during high-demand activities such as pivoting or lifting. Additionally, stretching facilitates better lymphatic drainage and blood flow, reducing post-exercise soreness and enhancing recovery. By integrating hip tendonitis stretches into your daily wellness routine, you’re not just managing symptoms—you’re proactively conditioning your neuromuscular system for long-term stability and coordination.
2. How can you adapt hip tendonitis rehab exercises for different fitness levels?
Hip tendonitis rehab exercises can and should be adapted to align with an individual’s current level of strength, mobility, and pain tolerance. For beginners or those in acute pain, isometric holds such as supine glute squeezes are safe yet effective in building foundational strength. Intermediate users may incorporate resistance bands to challenge hip abductors and stabilizers, while advanced individuals might integrate unilateral movements like step-ups or single-leg bridges to mimic real-world demands. These adaptations ensure that rehab exercises remain effective and appropriately scaled. By tailoring hip tendonitis rehab exercises in this manner, individuals reduce the risk of aggravating the tendon and improve adherence through attainable progression.
3. Are there psychological benefits to engaging in hip tendonitis stretching exercises?
Absolutely. Engaging in hip tendonitis stretching exercises can produce powerful psychological benefits, especially for individuals dealing with chronic discomfort or limited mobility. Stretching activates the parasympathetic nervous system, which promotes relaxation and stress reduction. Many users report decreased anxiety and improved mood after a focused stretching session. Moreover, the act of reclaiming movement and reducing pain fosters a greater sense of self-efficacy, boosting emotional resilience and commitment to healing. Over time, this psychological reinforcement becomes a valuable ally in sustaining long-term recovery and preventing fear-avoidance behaviors that can hinder rehabilitation.
4. What are the risks of neglecting hip tendonitis stretches after initial recovery?
Once symptoms subside, many individuals prematurely discontinue their hip tendonitis stretches, unaware of the long-term consequences. Unfortunately, this can lead to reduced tissue elasticity, weakened neuromuscular coordination, and increased likelihood of relapse. Tendons are notoriously slow to adapt to changes in load, and discontinuing stretching too early may disrupt the recovery trajectory. In the long run, skipping regular hip tendonitis stretching exercises can create new areas of tightness and imbalance, eventually leading to compensatory movement patterns that reintroduce pain. A maintenance routine is essential, even after functional recovery appears complete.
5. How can you make hip tendonitis rehab exercises more engaging to encourage long-term adherence?
Sustainability is crucial for the success of any rehabilitation program. To keep hip tendonitis rehab exercises engaging, consider integrating them into larger movement routines or pairing them with activities you already enjoy, such as yoga or resistance training. Using apps that offer progress tracking and visual feedback can also motivate consistency. Social support adds another dimension—exercising with a partner or in a group rehab setting introduces accountability and enjoyment. By weaving rehab into a broader fitness framework, individuals are more likely to stay committed to their hip tendonitis rehab exercises over the long term.
6. Can hip tendonitis stretching exercises be combined with mobility tools like foam rollers?
Yes, combining hip tendonitis stretching exercises with mobility tools such as foam rollers, massage balls, or resistance bands can greatly enhance their effectiveness. Foam rolling before stretching helps release fascial restrictions, improving muscle pliability and preparing tissues for elongation. Resistance bands add dynamic resistance and promote active engagement of opposing muscle groups during stretching, thereby improving joint integrity. These tools serve to amplify the therapeutic value of each stretch, making hip tendonitis stretches more comprehensive and impactful. When used correctly, they allow for deeper, more effective release without compromising safety.
7. How do lifestyle habits impact the success of hip tendonitis rehab exercises?
Lifestyle choices can significantly influence the effectiveness of hip tendonitis rehab exercises. Poor posture from prolonged sitting, inconsistent sleep schedules, and inadequate hydration all impair muscle recovery and contribute to tendon stiffness. On the other hand, maintaining an anti-inflammatory diet, optimizing rest cycles, and managing stress through mindfulness can enhance tissue repair. Environmental adjustments, such as using ergonomic seating or standing desks, reduce ongoing strain on the hip. In essence, your everyday habits either reinforce or counteract the benefits of your rehab routine, underscoring the importance of a holistic approach to healing.
8. What role does neuromuscular re-education play in hip tendonitis recovery?
Neuromuscular re-education is a critical yet often underemphasized component of recovery that involves retraining the body to perform correct movement patterns. After an injury, the nervous system may adopt compensatory mechanisms that avoid pain but perpetuate dysfunctional alignment. By incorporating exercises that challenge balance, coordination, and core activation, individuals can rewire these patterns. For example, closed-chain movements like standing hip circles or balance board exercises force the hip stabilizers to fire in a synchronized manner. These drills are especially valuable when paired with hip tendonitis rehab exercises, as they promote lasting improvements in motor control and movement efficiency.
9. Are there occupational strategies for integrating hip tendonitis stretches into a desk-based routine?
Yes, individuals with sedentary jobs can incorporate hip tendonitis stretches discreetly throughout the workday. Standing hip flexor stretches can be done next to a desk during short breaks, and seated figure-four stretches work well while sitting. Employers who support ergonomic wellness might even allow for movement breaks or standing desks, further facilitating recovery. Additionally, stretching apps or calendar reminders can prompt consistent implementation without requiring a gym setting. These micro-sessions ensure that hip tendonitis stretching exercises remain an accessible and ongoing part of the workday without significant disruption.
10. What future developments in rehab technology might improve outcomes for hip tendonitis?
Emerging rehabilitation technologies are set to transform how we approach conditions like hip tendonitis. Wearable biofeedback devices that monitor muscle activation and joint angles in real time are being refined to offer individualized insights into movement quality. Augmented reality (AR) and virtual reality (VR) platforms may soon guide users through hip tendonitis rehab exercises with precision cues and immersive feedback. Additionally, AI-driven apps could tailor stretching routines based on symptom tracking and progress data. These innovations promise to elevate both the personalization and effectiveness of hip tendonitis stretches and rehab interventions in the coming years.
Conclusion: Long-Term Success Through Targeted Hip Tendonitis Stretches and Rehab Exercises
The path to recovery from hip tendonitis is neither linear nor uniform, but with the right combination of evidence-based strategies, it is entirely achievable. A program that integrates hip tendonitis stretches with progressive hip tendonitis rehab exercises provides the foundation for healing, strength, and restored mobility. Flexibility training and mindful movement practices further enhance outcomes by addressing the underlying contributors to tendon overload.
By understanding the science behind tendon healing and committing to a holistic, personalized approach, individuals can reclaim their physical freedom and prevent future setbacks. Whether you are a recreational athlete, a busy professional, or someone simply striving for pain-free movement, these principles offer a roadmap to resilient hip health. With patience, consistency, and expert guidance, smart recovery becomes not only possible but sustainable for the long haul.
Further Reading:
Exercises to Help With Hip Tendonitis
Hip Tendonitis Exercises: Simple PT-Recommended Moves to Help You Feel Better and Get Moving


