Hip injuries can severely affect quality of life, limiting mobility, strength, and independence. Whether stemming from athletic strain, surgery, chronic pain, or age-related degeneration, rehabilitation is critical to restoring function. This article explores medically accurate and evidence-based hip rehabilitation exercises designed to improve flexibility, mobility, and overall recovery. Drawing on clinical principles of physical therapy for hip recovery, we present a structured, holistic understanding of hip rehab and why it matters.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
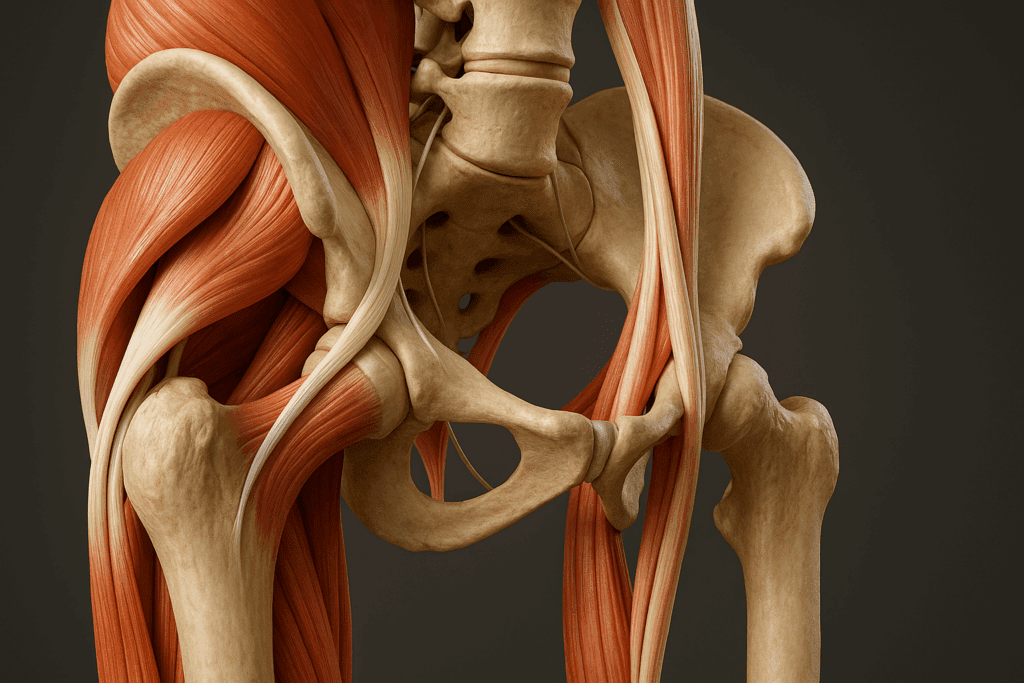
Understanding the Role of the Hip Joint in Mobility and Stability
The hip is one of the most complex and powerful joints in the body, allowing for multidirectional movement while bearing the weight of the upper body. It plays an essential role in virtually every movement pattern—from walking and standing to squatting and pivoting. When compromised, the cascading effects can alter posture, gait mechanics, and balance, contributing to secondary injuries. Hence, an effective hip rehabilitation plan must take into account not only the local joint function but also how the hip integrates with surrounding musculature and kinetic chains.
Hip rehab exercises often target a combination of strength, flexibility, and neuromuscular coordination. Weak or inhibited muscles, such as the gluteus medius or hip flexors, can destabilize the pelvis, causing compensation patterns. Furthermore, stiff hip joints or tight muscles may impede normal biomechanics, leading to altered loading in the lumbar spine or knees. This interconnectedness highlights why a comprehensive approach to hip rehabilitation is crucial.

The Role of Fascia and Myofascial Release in Hip Mobility
Fascia is a dense connective tissue that weaves through and surrounds muscles, nerves, and joints, influencing movement quality and muscle efficiency. Recent research highlights the integral role fascia plays in joint stiffness, mobility restrictions, and chronic pain—particularly in areas like the hip, which bear a high mechanical load. Fascial adhesions in the iliotibial band, tensor fasciae latae, or deep hip rotators can limit flexibility and contribute to compensatory movement patterns.
Myofascial release, whether through foam rolling, manual therapy, or tool-assisted techniques, is now a common component of advanced hip rehab. A comprehensive session might include slow, deliberate pressure on trigger points around the glutes, hip flexors, and adductors. These sessions reduce neuromuscular tension and improve hydration in connective tissues, resulting in smoother joint mechanics and enhanced performance during dynamic movement. Incorporating fascial work alongside hip rehabilitation exercises maximizes tissue readiness and restores optimal muscle recruitment patterns.
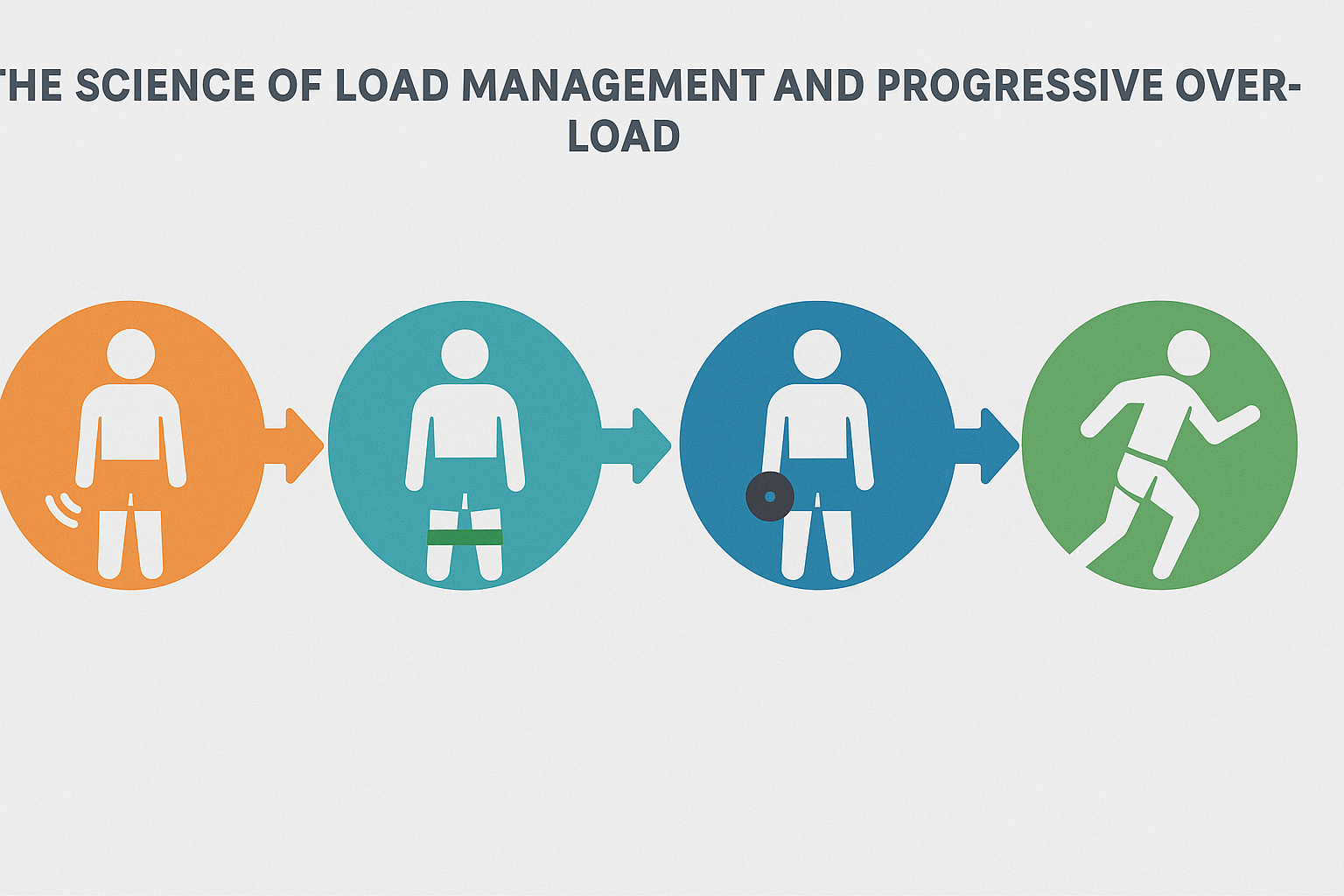
The Science of Load Management and Progressive Overload
Once basic hip strength and mobility are re-established, progressing to load-bearing exercises is essential for building resilience. This phase focuses on the principle of progressive overload—the systematic increase of stress placed on the musculoskeletal system to promote adaptive strength and endurance.
In practical terms, this may involve transitioning from bilateral to unilateral exercises, introducing external weights, or increasing the complexity of movement patterns. Advanced hip rehab exercises such as weighted Bulgarian split squats, deadlifts, kettlebell swings, and step-ups with eccentric control are excellent tools for enhancing hip strength under real-world conditions. These exercises not only target the glutes, hip flexors, and abductors but also challenge trunk stability and neuromuscular control.
The PT hip framework used in performance therapy includes detailed progression criteria to prevent overuse injuries. By tracking performance metrics like time-under-tension, rate of perceived exertion (RPE), and recovery windows, practitioners can safely guide patients from rehabilitation to athletic reintegration. This meticulous approach minimizes setbacks while allowing tissues to develop tensile capacity, which is particularly critical for tendon health and long-term joint protection.

Addressing Biomechanical Imbalances with Gait Retraining
Gait abnormalities are a common aftermath of hip injuries, particularly among individuals recovering from labral tears, femoroacetabular impingement (FAI), or hip replacements. Compensatory patterns such as hip hiking, pelvic drop, or reduced stride length often persist unless specifically addressed. Gait retraining corrects these dysfunctions using biomechanical feedback and motor learning principles.
Advanced gait analysis systems can detect subtle asymmetries in stride timing, ground reaction forces, and limb loading. These insights inform corrective strategies that might include treadmill training with visual feedback, mirror drills, or metronome-paced walking. In conjunction with specific hip rehabilitation exercises, gait retraining restores natural walking mechanics, improves energy efficiency, and reduces the likelihood of reinjury.
For runners and athletes, return-to-sport protocols often emphasize high-level gait drills that simulate sport-specific demands. Sprint mechanics, change-of-direction drills, and deceleration techniques are integrated with strength training to refine hip coordination. This ensures that the joint is not only strong but also intelligent—capable of adapting to dynamic, high-speed environments.

Enhancing Core-Hip Integration for Dynamic Control
The hip does not function in isolation. It works synergistically with the core musculature to maintain postural alignment, absorb impact, and transfer forces between the upper and lower body. Weakness or delayed activation in the deep core stabilizers can lead to excessive lumbar compensation, poor pelvic control, and increased stress on the hip joint.
In advanced rehab, core-hip integration becomes a focal point. Exercises such as Pallof presses, dead bugs with hip extension, and bird dogs with band resistance challenge the anterior and posterior chains to coordinate movement. These movements promote lumbopelvic stability, ensuring that hip flexion and extension occur from a neutral spine position.
Research supports the use of dynamic neuromuscular stabilization (DNS) techniques in patients undergoing physical therapy for hip conditions. DNS emphasizes diaphragmatic breathing, intra-abdominal pressure, and segmental control—all of which are critical for efficient hip mechanics. When integrated with hip rehab exercises, core training enhances joint control during complex activities like squatting, lunging, or running.
Sport-Specific Return-to-Performance Programming
While general rehab restores daily function, athletes and highly active individuals require sport-specific reintegration to fully resume training and competition. This phase bridges traditional physical therapy for hip injuries with performance enhancement. The goal is to retrain movement under the unique demands of a given sport, ensuring that performance gains do not come at the expense of joint safety.
For example, a soccer player may need to focus on multidirectional sprinting, lateral acceleration, and explosive hip rotation. A dancer might prioritize turnout control, single-leg balance, and extended range flexibility. Hip rehabilitation in these cases must be as individualized as the sport itself. Movement assessments, video analysis, and reactive agility drills help identify gaps in readiness and guide exercise selection.
Sport-specific programming often incorporates plyometric sequences, resisted sprint drills, and dynamic perturbation training. These techniques simulate the unpredictable nature of athletic competition and train the hip to respond reflexively. Additionally, monitoring external load (such as GPS tracking or jump count) ensures the gradual buildup of training volume, preventing re-aggravation of hip flexor strain or abductor dysfunction.
Incorporating Neurological Rehabilitation for Chronic Hip Conditions
Chronic hip pain conditions, including osteoarthritis and gluteal tendinopathy, involve more than just structural tissue damage. Central sensitization—a heightened sensitivity of the nervous system—can amplify pain signals and hinder recovery. Advanced rehab addresses this neurological component through education, desensitization protocols, and graded exposure therapy.
Graded motor imagery, mirror therapy, and tactile desensitization are tools used to retrain the brain’s representation of the hip joint. By gradually exposing the patient to movement patterns that previously triggered pain, these methods help decrease fear-avoidance behaviors and restore function. Combined with traditional hip rehab exercises, they offer a comprehensive strategy for long-standing cases.
Cognitive-behavioral strategies and pain neuroscience education are also being integrated into physical therapy for hip rehabilitation. Patients learn how stress, sleep, and emotional states influence pain processing. This biopsychosocial approach empowers patients to actively participate in their recovery and fosters long-term resilience.
Leveraging Wearable Technology and Digital Biofeedback
The integration of wearable technology and digital feedback systems is revolutionizing how hip rehab exercises are implemented and monitored. Devices such as inertial measurement units (IMUs), smart resistance bands, and motion-sensing apps provide real-time feedback on joint angles, speed, and symmetry. These insights allow clinicians to fine-tune exercises and ensure proper form even when patients are unsupervised.
For example, a patient performing hip abductor pain exercises may receive instant feedback on lateral shift or pelvic tilt, allowing them to self-correct. Over time, this enhances motor learning and accelerates neuromuscular efficiency. Moreover, remote monitoring tools expand access to care, making it easier for patients in remote areas or with mobility limitations to receive expert guidance.
Gamified rehab platforms increase engagement and adherence. Patients can track their progress, set performance goals, and visualize improvement over time. This psychological boost not only improves outcomes but also reinforces the value of consistent participation in hip rehabilitation programs.
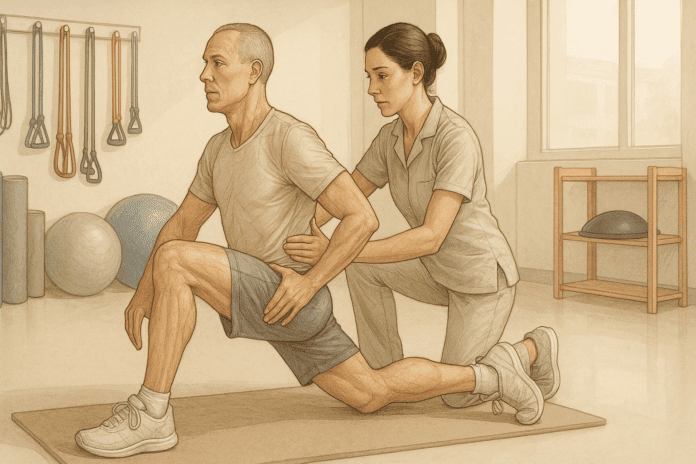
The Science of Physical Therapy for Hip Recovery
Physical therapy for hip injuries emphasizes individualized care, integrating assessment, manual therapy, and targeted movement re-education. A physical therapist typically begins with a detailed evaluation to identify deficits in range of motion, strength, and gait. Treatment plans are customized based on the patient’s diagnosis—whether it involves post-surgical recovery, hip flexor strain, bursitis, labral tears, or osteoarthritis.
Modern research underscores the effectiveness of neuromuscular retraining and progressive resistance exercises in restoring hip function. These methods improve joint proprioception, enhance motor control, and reduce reinjury risk. For instance, studies have shown that tailored hip rehabilitation exercises improve not only strength but also balance and fall prevention in older adults. In athletes, PT hip protocols reduce recovery time while ensuring safe return-to-play standards.
Many physical therapists integrate modalities such as dry needling, soft tissue mobilization, and instrument-assisted release techniques to reduce inflammation and improve tissue extensibility. These interventions, combined with carefully dosed exercises, create a synergistic effect, accelerating healing without compromising tissue integrity.

Foundational Hip Rehab Exercises for Early-Stage Recovery
In the acute or early post-injury phase, the goal is to control inflammation, prevent stiffness, and initiate gentle movement. Isometric exercises form the foundation of early-stage rehabilitation, offering muscle activation without joint movement. These are crucial in maintaining neuromuscular connections while preventing atrophy.
For example, gluteal squeezes, quad sets, and static hip abductions can be performed lying down, reducing mechanical stress on the joint. Passive range of motion movements—such as assisted heel slides and gentle hip rotations—help maintain joint mobility without provoking pain. At this stage, any exercises that reproduce discomfort or sharp pain must be avoided.
One particularly beneficial technique involves the use of hydrotherapy or aquatic therapy. The buoyancy of water reduces gravitational loading, allowing individuals to practice gait re-education and dynamic movement earlier than they might on land. Physical therapy for hip recovery often includes water-based therapy as a bridge between immobility and functional movement.
Advancing to Functional Hip Rehabilitation
As inflammation subsides and range of motion improves, the rehabilitation plan must evolve to incorporate functional strengthening and dynamic stability. This phase targets not only the hip but the entire kinetic chain, focusing on movement quality and load tolerance.
Hip rehab exercises in this phase include clamshells, bridges, and standing hip abductions, all of which emphasize control and alignment. Gradual resistance is introduced using resistance bands, light weights, or bodyweight progression. Importantly, movement quality should always take precedence over volume or load. Poorly executed exercises may reinforce compensatory patterns rather than restore true function.
This is also the phase where balance and proprioceptive training are prioritized. Tools such as wobble boards, balance pads, or single-leg stance drills are integrated to train the body’s automatic stabilizers. Research indicates that incorporating these exercises improves long-term outcomes and reduces the recurrence of hip injuries, particularly in athletes and active populations.
The hip flexor strain rehab protocol PDF often referenced in clinical circles typically includes controlled lunges, low-impact cardio, and modified yoga poses. These exercises are designed to challenge the hip through its full range while respecting tissue healing timelines. A physical therapist will monitor progress and adjust the protocol as necessary, ensuring a balance between stress and recovery.
Restoring Flexibility Through Targeted Stretching and Mobility Work
Flexibility training is often misunderstood as a passive or secondary component of rehab. However, for hip rehabilitation, restoring soft tissue pliability is central to regaining full function. Muscles such as the iliopsoas, tensor fasciae latae, and adductors commonly develop tightness after injury due to disuse, guarding, or inflammation.
Gentle static stretching, active-assisted mobility work, and dynamic flow movements help lengthen shortened tissues and improve fascial glide. For instance, incorporating modified pigeon pose or a supine figure-four stretch can address posterior hip tightness, while kneeling hip flexor stretches alleviate anterior restrictions. These hip rehabilitation exercises enhance joint mechanics, allowing smoother and more coordinated motion.
In physical therapy for hip patients, stretching is often coupled with breathing and neuromuscular release techniques. This helps the central nervous system recalibrate muscle tone, reducing guarding and pain sensitivity. It also encourages full-range movement without fear of injury, which is essential in both physical and psychological recovery.

Preventative Hip Rehab: Building Resilience Before Injury Occurs
While much of hip rehabilitation focuses on post-injury or post-surgical care, there is growing recognition of its role in prevention. Prehabilitation, or “prehab,” aims to fortify the joint against future stress through strategic strengthening, mobility, and coordination training. Athletes, older adults, and even desk-bound workers can benefit from proactive hip rehab strategies.
A preventative program may include daily mobility flows, deep squatting drills, resisted side-stepping, and posterior chain activation. These exercises address common deficits in glute activation, hip flexor length, and lateral stability. By integrating these movements into a regular fitness routine, individuals create a buffer against overuse injuries, muscle imbalances, and degenerative changes.
Hip flexor strain rehab protocol PDFs designed for athletic populations often include preventative phases, featuring dynamic warm-ups, tissue priming routines, and load management strategies. Encouraging a preventative mindset shifts the narrative from rehabilitation to optimization—empowering individuals to take control of their joint health before dysfunction arises.
Managing Hip Abductor Pain with Specific Strengthening Strategies
One of the most overlooked contributors to chronic hip dysfunction is abductor weakness. The gluteus medius and minimus are essential for stabilizing the pelvis during single-leg stance and walking. When weak or inhibited, they allow excessive pelvic drop, placing strain on the lower back, IT band, and knees. This is often seen in individuals with hip abductor pain or gluteal tendinopathy.
Effective hip abductor pain exercises include side-lying leg lifts, lateral band walks, and single-leg bridges. These target the lateral hip musculature in both open and closed kinetic chain formats. Progression should be methodical, moving from low-resistance isometrics to functional dynamic drills.
A core principle of hip rehab is ensuring that these muscles are not only strong but also firing at the right time. Functional electromyographic studies reveal that delayed gluteal activation correlates with increased injury risk. Therefore, hip rehabilitation programs often incorporate drills such as step-downs and lateral hops to train timing, control, and reactive stability.
The PT hip protocols designed for patients recovering from total hip arthroplasty also emphasize abductor re-education. Given that surgical approaches may disrupt soft tissues, special attention is paid to restoring symmetrical gait and hip balance. Patients are typically instructed in home programs that combine strength, endurance, and mobility in a structured format.
The Importance of Progress Monitoring and Pain Management
A successful hip rehabilitation plan includes regular assessment checkpoints to evaluate progress, modify intensity, and address setbacks. Physical therapists use tools such as goniometers for range of motion, handheld dynamometers for strength, and motion capture analysis for gait and movement efficiency. These metrics provide objective feedback that guides clinical decision-making.
Patient education also plays a pivotal role in recovery. Understanding pain science, tissue healing timelines, and the rationale behind each exercise enhances adherence and reduces fear. Many patients mistakenly associate soreness with harm, which can lead to avoidance behaviors and delayed progress. Clear communication about normal post-exercise sensations versus warning signs helps build confidence and autonomy.
Modern hip rehabilitation protocols often incorporate evidence from pain neuroscience. This includes graded exposure, where patients are gently introduced to movements that previously caused discomfort, retraining the nervous system to tolerate them. For those recovering from more severe injuries or surgeries, such as labral repair or joint replacement, this approach fosters resilience and long-term success.
Pain management strategies, such as cryotherapy, transcutaneous electrical nerve stimulation (TENS), and mindfulness-based stress reduction, may also be integrated. These adjuncts complement the physical component of rehab, providing holistic support and improving overall quality of life.
Integrating Yoga and Mobility Training into Long-Term Hip Health
Once initial rehabilitation goals have been achieved, maintaining hip health becomes the next priority. This is where the integration of yoga, mobility training, and functional fitness can be highly effective. These practices not only promote flexibility and strength but also foster body awareness and movement efficiency.
Yoga poses such as Warrior II, Triangle, and Extended Side Angle emphasize hip opening, lateral stability, and full-body coordination. Mobility flows, combining controlled articular rotations and end-range isometrics, enhance joint health and prevent stiffness. These exercises go beyond traditional rehab by addressing neuromuscular control and movement complexity.
Patients transitioning out of formal physical therapy for hip recovery often benefit from structured group classes or personalized movement coaching. These environments provide continued stimulus, social motivation, and expert guidance. Moreover, by incorporating hip rehab exercises into regular routines, individuals reduce the risk of recurrence and promote lifelong joint health.
For those managing chronic conditions or recurring pain, such as hip flexor strain or impingement syndrome, mobility-focused practices can serve as ongoing therapy. The hip flexor strain rehab protocol PDF often includes yoga-inspired sequences to restore anterior chain length, improve posture, and build core integration—all of which are crucial for injury prevention.
Frequently Asked Questions: Expert Insights on Hip Rehabilitation and Recovery
1. What are some lesser-known techniques that enhance the effects of hip rehabilitation exercises?
One of the most underrated strategies for enhancing hip rehabilitation exercises is using proprioceptive stimulation techniques like vibration therapy and barefoot balance drills. These approaches awaken the sensory receptors in the hip and foot, improving neuromuscular control and reducing compensation patterns. When paired with traditional hip rehab exercises, proprioceptive tools help sharpen joint awareness, which is especially useful for patients with chronic instability or post-surgical deficits. Another effective method is cross-body contralateral training, where engaging the opposite limb (e.g., left arm when rehabbing the right hip) can stimulate neurological pathways to accelerate recovery. These techniques, though often overlooked, add a new dimension to physical therapy for hip dysfunction and encourage more dynamic rehabilitation outcomes.
2. How can mental health influence the success of a hip rehab program?
Mental health significantly impacts physical recovery, especially during long or painful hip rehabilitation journeys. Anxiety, depression, or fear-avoidance beliefs can lead patients to underperform during hip rehab exercises or drop out of therapy prematurely. Integrating mindfulness-based stress reduction (MBSR) or guided imagery can improve mental resilience and reduce perceived pain during movement. Emotional support also plays a vital role in adherence; patients who receive encouragement from their support networks tend to be more consistent with physical therapy for hip recovery. A comprehensive PT hip program should consider both psychological and physiological variables to ensure optimal healing and long-term adherence.
3. Are there specific modifications for hip rehab exercises during pregnancy?
Pregnancy introduces biomechanical changes that may require tailored modifications to hip rehab exercises. As the center of gravity shifts and hormonal changes loosen ligaments, it’s important to avoid positions that overstretch the hip flexors or stress the pelvis. Lateral band walks, supported squats, and side-lying hip abductor pain exercises can safely activate critical stabilizers without placing excessive strain on the joints. Prenatal physical therapy for hip pain often emphasizes pelvic alignment, diaphragmatic breathing, and gentle mobility work rather than high-load strengthening. Consulting a therapist with prenatal expertise ensures the hip rehabilitation program is both safe and effective throughout pregnancy.
4. Can wearable tech meaningfully improve outcomes in hip rehabilitation?
Wearable devices are increasingly valuable in hip rehabilitation, offering real-time feedback and long-term tracking for patients and clinicians. Tools like smart resistance bands, motion sensors, and gait analysis wearables provide insights into range of motion, speed, symmetry, and joint angles. For example, a patient performing hip abductor pain exercises can instantly adjust their form based on visual or auditory feedback. These devices also promote adherence, especially when paired with app-based reminders and gamified progress tracking. By integrating wearables with hip rehabilitation exercises, therapists can deliver personalized, data-informed care that empowers patients to progress safely at home.
5. How do cultural or lifestyle factors influence adherence to physical therapy for hip recovery?
Cultural beliefs and lifestyle habits profoundly affect how individuals perceive and engage with physical therapy for hip recovery. In some cultures, rest is emphasized over activity during illness or injury, which may conflict with the progressive loading required for successful hip rehab. Time constraints, caregiving responsibilities, and work-related pressures can also limit participation in scheduled sessions or at-home programs. Therapists who acknowledge these variables can adapt hip rehabilitation exercises to align with the patient’s routines—offering shorter routines, home-based alternatives, or culturally sensitive education. Addressing these factors can significantly enhance outcomes by improving compliance and building trust.
6. Is it possible to overtrain during a hip flexor strain rehab protocol, and what are the warning signs?
Yes, overtraining during a hip flexor strain rehab protocol can stall recovery and increase injury risk. Common warning signs include prolonged soreness, worsening tightness, increased joint instability, and disrupted sleep patterns. Patients may assume that more intensity equals faster healing, but this often backfires, especially in tendon-related conditions where gradual loading is essential. A well-designed hip flexor strain rehab protocol PDF outlines rest intervals, intensity levels, and progression timelines to prevent overtraining. Monitoring fatigue levels and using tools like the Borg scale for perceived exertion can help maintain balance between challenge and recovery.
7. What is the role of nutrition in accelerating hip rehabilitation?
Nutrition supports every stage of the healing process, yet it is often neglected in standard PT hip programs. Amino acids from protein facilitate muscle repair, while micronutrients like magnesium and vitamin D support nerve function and bone remodeling. Omega-3 fatty acids reduce systemic inflammation, aiding in joint recovery and reducing pain associated with hip rehab exercises. Collagen supplementation, particularly when paired with loading exercises, has been shown to improve tendon structure in chronic cases. Integrating dietary support into physical therapy for hip recovery can enhance tissue healing, improve energy levels, and promote more consistent rehab performance.
8. Can older adults safely engage in advanced hip rehab exercises?
Absolutely, but with age-appropriate considerations. Advanced hip rehab exercises like step-ups, resistance-based bridges, and single-leg balance work can be safely adapted for older adults by modifying intensity and volume. Functional strength training is particularly important in this population to prevent falls and preserve independence. When progressing exercises, it’s crucial to monitor for signs of fatigue or altered gait that may signal poor movement quality. Physical therapy for hip function in older adults should also include cognitive-motor challenges to improve coordination and confidence. With professional oversight, older adults can achieve remarkable gains in flexibility, strength, and mobility through structured hip rehabilitation.
9. How does sleep quality affect the success of a hip rehabilitation program?
Sleep is a cornerstone of recovery, and its disruption can significantly impede the benefits of hip rehabilitation. Poor sleep diminishes hormone levels critical for tissue repair, reduces pain tolerance, and impairs cognitive function necessary for learning new motor patterns. Patients undergoing intensive hip rehab exercises who lack restorative sleep often experience plateaued progress or increased sensitivity to discomfort. Strategies such as sleep hygiene education, relaxation techniques, and nutritional support (e.g., magnesium, tryptophan-rich foods) should be integrated into PT hip protocols. A well-rested body responds more effectively to the adaptive stress of physical therapy for hip recovery.
10. What emerging innovations are shaping the future of hip rehabilitation?
The future of hip rehabilitation is being reshaped by innovations in regenerative medicine, virtual reality, and AI-driven therapy planning. Platelet-rich plasma (PRP) injections and stem cell therapies show promise in regenerating damaged hip tissues when paired with structured hip rehab exercises. Virtual reality platforms are being used to gamify movement, improving motivation and range of motion in patients recovering from surgeries or chronic injuries. Artificial intelligence tools now assist clinicians in creating predictive, personalized PT hip programs that adjust in real-time based on patient performance. These advancements suggest that physical therapy for hip conditions is entering an era of hyper-personalized, tech-enhanced recovery.
Conclusion: Elevating Recovery with Strategic Hip Rehabilitation Exercises
Restoring hip health after injury requires a multifaceted and evidence-informed approach. Science-backed hip rehabilitation exercises are not just about regaining motion but about rebuilding confidence, coordination, and long-term resilience. By leveraging principles from physical therapy for hip function, mobility training, and neuromuscular science, individuals can return to activity with greater efficiency and reduced risk of reinjury.
Incorporating exercises from the hip flexor strain rehab protocol PDF, strengthening routines for hip abductor pain, and general PT hip strategies ensures comprehensive care that addresses all components of the kinetic chain. From early-stage healing to advanced athletic performance, hip rehab exercises lay the foundation for functional movement and pain-free living.
Ultimately, the goal is to transform rehabilitation into a lifestyle that prioritizes flexibility, strength, and conscious movement. Whether recovering from surgery or preventing future issues, the journey through hip rehabilitation offers a valuable opportunity to deepen body awareness and optimize physical health. In doing so, we not only restore function but empower individuals to move through life with strength and confidence.