Living with hip osteoarthritis can feel like navigating an invisible labyrinth. The stiffness, reduced mobility, and persistent discomfort often arrive unannounced, slowly encroaching on activities that once brought joy—a leisurely walk, gardening on a sunny afternoon, or simply rising from a chair with ease. While medication and surgical options have long been pillars of osteoarthritis management, a growing body of evidence underscores the critical importance of movement, particularly stretching, in alleviating symptoms and preserving joint function. In this comprehensive exploration, we delve into the transformative power of stretching as a cornerstone of physiotherapy for hip osteoarthritis. With guidance rooted in science and tailored for real-life application, this article provides expert insight into how targeted, low-impact hip osteoarthritis exercises can restore mobility, reduce pain, and enhance long-term quality of life.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Understanding Hip Osteoarthritis and Its Impact on Daily Life
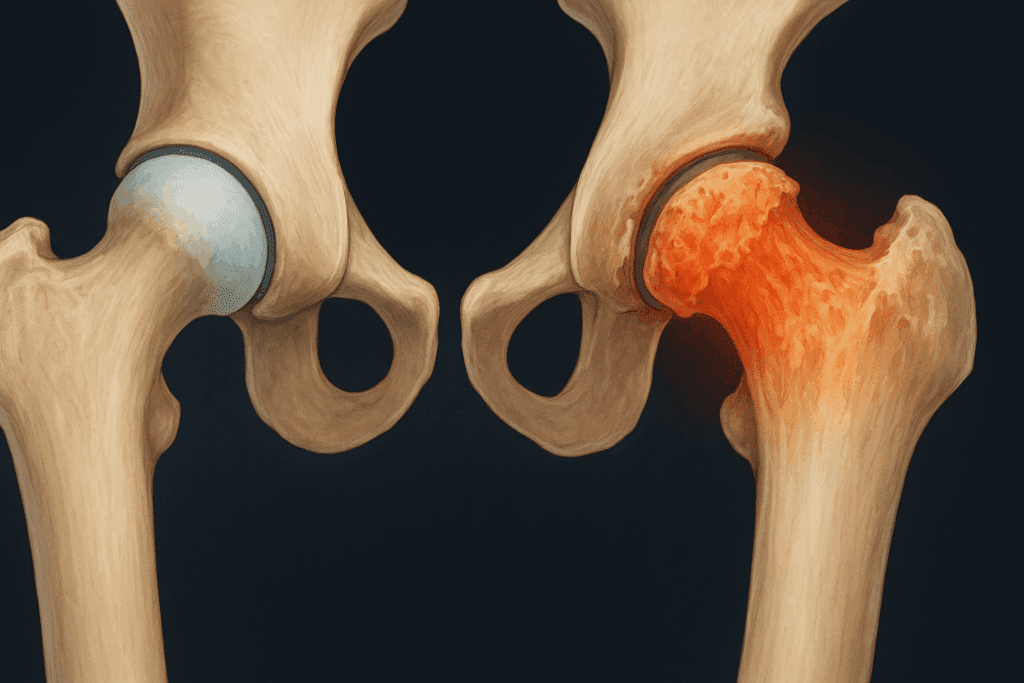
Hip osteoarthritis, a degenerative joint disease, involves the gradual breakdown of cartilage in the hip joint. Over time, this deterioration leads to increased friction between bones, resulting in inflammation, pain, and reduced range of motion. The hip, being a weight-bearing joint, is particularly susceptible to the effects of osteoarthritis. Everyday activities such as standing, walking, or climbing stairs become increasingly difficult, often causing individuals to avoid movement altogether. Unfortunately, this response only exacerbates the problem. Reduced physical activity leads to joint stiffness, muscular weakness, and further mobility limitations, perpetuating a debilitating cycle.
Physiotherapy for hip osteoarthritis offers a proactive strategy to break this cycle. By engaging in gentle, evidence-based movements that focus on flexibility, strength, and alignment, individuals can effectively manage symptoms and even slow the progression of the disease. Understanding the physiological underpinnings of osteoarthritis helps reinforce why movement—specifically stretching—is not only safe but essential in mitigating discomfort and regaining control over one’s mobility.
Understanding Biomechanical Patterns and Movement Dysfunction
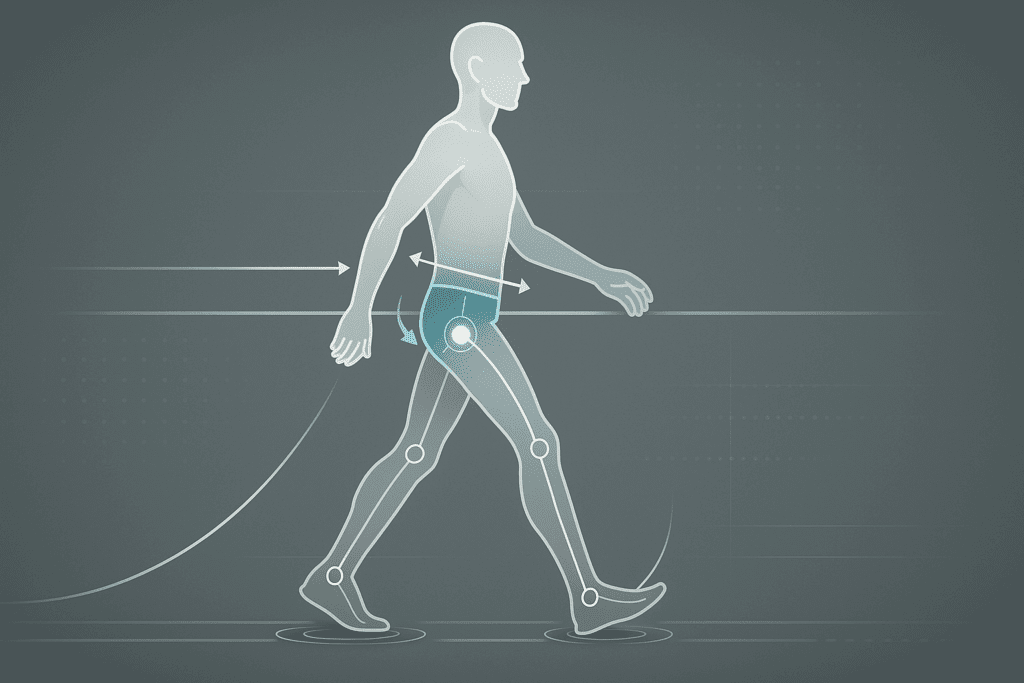
One underappreciated aspect of managing hip osteoarthritis is addressing faulty movement patterns and biomechanical dysfunctions. When the body compensates for pain or stiffness, it often recruits muscles and joints in a way that disrupts balance and symmetry. Over time, these compensations can lead to further joint strain, reduced mobility, and even injury in adjacent areas such as the knees, lower back, or ankles.
Movement analysis, conducted by physiotherapists or movement specialists, helps uncover these subtle dysfunctions. Using tools like video gait analysis, wearable motion sensors, or manual assessments, clinicians can pinpoint specific imbalances such as unequal weight distribution, pelvic tilt, or hip drop during walking. Once identified, targeted corrective exercises can be introduced to retrain neuromuscular patterns and promote efficient, joint-sparing movement.
Additionally, gait retraining is often essential. Many individuals with hip osteoarthritis subconsciously shorten their stride or avoid full hip extension due to discomfort. With guidance, they can gradually restore more natural walking mechanics, redistributing joint forces and minimizing cumulative stress.
The Role of Neuromuscular Reeducation
Neuromuscular reeducation is another critical component in advanced physiotherapy for hip osteoarthritis. This technique focuses on improving the communication between the nervous system and muscular system to enhance motor control. Through specific drills, patients can learn to activate dormant or underused muscles while inhibiting those that are compensating improperly.
One classic example is the delayed or weakened activation of the gluteus medius muscle in hip osteoarthritis. This muscle plays a central role in stabilizing the pelvis during walking, and its dysfunction contributes to gait asymmetries and increased joint loading. Exercises that reestablish gluteal control—such as isolated side-lying leg lifts or standing hip hikes—help restore proper function and relieve joint strain.
Balance training, proprioceptive drills, and dynamic coordination tasks (like single-leg stance on an unstable surface) are often employed to further reinforce neuromuscular control. These activities not only benefit hip mechanics but also improve overall safety and reduce fall risk, which is a significant concern in older adults with joint degeneration.

Fascia and Myofascial Release Techniques
Fascia, the dense connective tissue that surrounds muscles, plays a vital role in joint mobility and movement efficiency. In individuals with osteoarthritis, fascial restrictions can contribute to joint stiffness, muscle imbalance, and pain. Myofascial release techniques, whether manual or instrument-assisted, aim to relieve these restrictions and restore tissue elasticity.
Manual myofascial release is performed by trained therapists who apply sustained pressure to specific areas of fascial tension. Foam rolling, a self-administered version of this technique, can also be incorporated into home routines. For hip osteoarthritis, key areas often targeted include the iliotibial band, quadriceps, glutes, and lower back muscles.
Regular myofascial work enhances blood flow, reduces muscle tone, and improves movement quality. When combined with stretching and strengthening exercises for arthritic knees and hips, these techniques amplify results and support long-term joint function. Importantly, they also contribute to sensory recalibration, helping the brain reinterpret pain signals and reducing chronic discomfort.
The Science Behind Stretching and Joint Health
Stretching plays a crucial role in joint health, particularly for those with hip osteoarthritis. When muscles and connective tissues surrounding the joint are consistently stretched, they become more pliable and resilient. This increased elasticity enhances overall joint mobility, allowing for smoother and less painful movement. Moreover, stretching improves circulation to the affected area, delivering oxygen and essential nutrients while aiding in the removal of metabolic waste products that may contribute to inflammation.
Scientific research consistently supports the value of stretching as part of a comprehensive rehabilitation approach. In patients with hip osteoarthritis, studies have shown that static and dynamic stretching routines can lead to measurable improvements in flexibility, walking speed, and pain reduction. These benefits are especially pronounced when stretching is combined with strength training and aerobic conditioning, which collectively address the multifaceted nature of joint health. The key is consistency, proper technique, and a personalized plan that accounts for the individual’s range of motion, pain tolerance, and physical limitations.

Adaptive Equipment and Lifestyle Ergonomics
Integrating adaptive tools into daily routines can significantly ease the burden of hip osteoarthritis. Devices such as reachers, sock aids, and raised toilet seats reduce the need for extreme joint angles that may exacerbate pain. Using a cane or walker, when prescribed by a healthcare professional, offloads the affected joint and improves balance, particularly during flare-ups.
Beyond mobility aids, ergonomic adjustments to home and work environments can prevent unnecessary joint strain. Chairs with appropriate seat height and lumbar support, adjustable standing desks, and kitchen tools with padded grips help reduce awkward postures and repetitive stress. These lifestyle interventions are often overlooked, yet they create a critical foundation for sustaining the benefits of physiotherapy for hip osteoarthritis.
Footwear, too, plays a role in biomechanical health. Shoes with proper arch support, shock absorption, and heel stability optimize alignment and reduce hip loading. Custom orthotics may be indicated for individuals with specific gait abnormalities or leg length discrepancies that compound joint stress.
The Emerging Role of Technology in Joint Rehabilitation
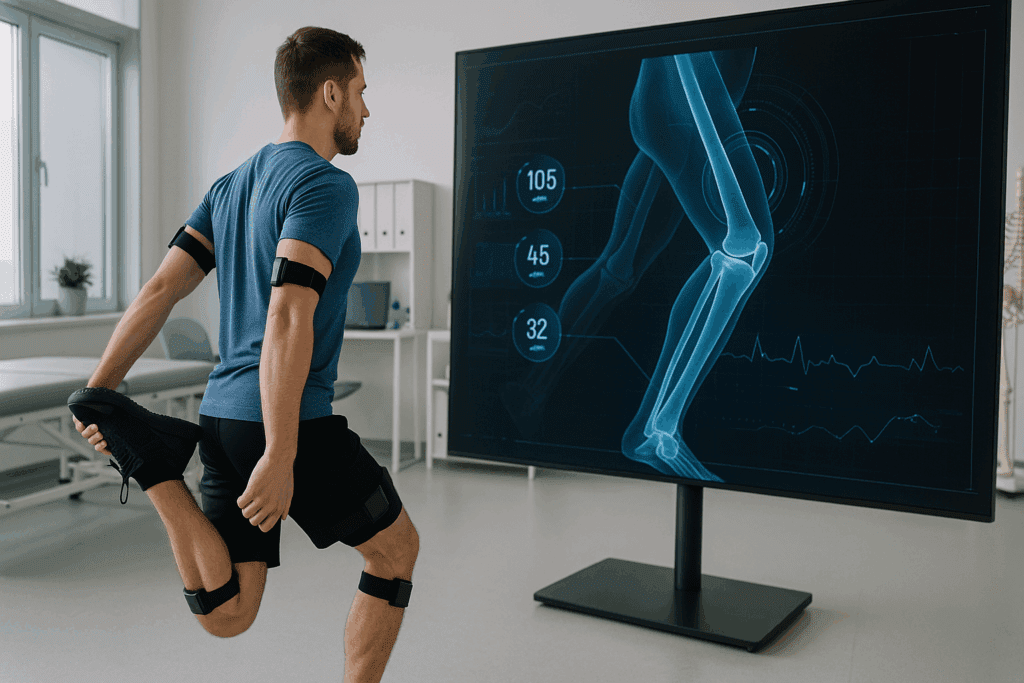
Advancements in technology are revolutionizing the way hip osteoarthritis is managed. Wearable sensors can now track joint angles, step counts, and gait patterns in real time, providing clinicians and patients with actionable feedback. Smartphone apps offer guided routines for stretching, strength training, and pain tracking, promoting accountability and convenience.
Telehealth physiotherapy has also emerged as a viable and effective alternative to in-person sessions, particularly for those with limited mobility or transportation challenges. Through virtual consultations, therapists can observe movement, provide corrective feedback, and adjust exercise plans dynamically.
Furthermore, virtual reality (VR) rehabilitation is being explored for its ability to gamify exercise and increase engagement. VR platforms create immersive environments where patients perform therapeutic movements in response to visual and auditory cues, enhancing motivation and adherence. These tools are especially valuable for long-term adherence, a cornerstone of successful management of hip osteoarthritis.
Key Principles of Safe Stretching for Hip Osteoarthritis
Safety is paramount when designing an exercise regimen for individuals with hip osteoarthritis. Inappropriate or overly aggressive movements can worsen pain or accelerate joint degeneration. Therefore, certain guiding principles must inform every stretching session. First, always begin with a gentle warm-up. This could involve light walking or the use of a stationary bike for five to ten minutes, which helps increase blood flow and prepare the muscles for activity.
Second, focus on proper alignment and posture throughout each stretch. Misalignment places undue stress on the hip joint and may offset the benefits of the exercise. When performing hip osteoarthritis exercises, it is essential to listen to the body. Stretching should never be painful. A mild to moderate pulling sensation is normal, but sharp or intense pain is a signal to stop immediately. Third, prioritize consistency over intensity. Performing shorter, more frequent sessions will yield better long-term results than infrequent, strenuous efforts.
Additionally, use support tools as needed. Yoga blocks, chairs, or resistance bands can enhance safety and effectiveness by providing stability and enabling proper form. Finally, breathe deeply and mindfully during stretches. Controlled breathing facilitates relaxation and helps the body transition more smoothly into deeper ranges of motion, ultimately improving the effectiveness of the stretching routine.
Redefining Success and Setting Functional Goals
Traditional success metrics in osteoarthritis rehabilitation often focus on pain scores and radiographic changes. However, a more patient-centered approach emphasizes functional improvements and quality of life. For some, success may mean walking to the mailbox without assistance; for others, it may involve returning to recreational activities or traveling without fear of pain.
Collaborative goal setting helps ensure that exercise programs align with personal values and daily needs. These goals should be SMART—specific, measurable, achievable, relevant, and time-bound—and regularly reviewed. Celebrating progress, no matter how small, reinforces motivation and validates the effort required to maintain consistent practice.
Importantly, setbacks are to be expected. Flare-ups, illness, or life events can disrupt routines. Rather than viewing these interruptions as failures, patients should be encouraged to approach them with curiosity and self-compassion. This mindset fosters long-term adherence and sustains the benefits of exercises for arthritic knees and hips.

Targeted Stretches to Alleviate Hip Osteoarthritis Symptoms
Specific stretching exercises can significantly ease discomfort and restore mobility for those managing hip osteoarthritis. One foundational stretch is the seated hip external rotation. Sitting on a sturdy chair, place one ankle across the opposite knee and gently press down on the raised knee to open the hip joint. This position stretches the piriformis and surrounding muscles that often become tight with osteoarthritis. Hold the stretch for 20 to 30 seconds, ensuring the movement remains within a pain-free range.
Another effective movement is the supine hamstring stretch. Lying on the back, loop a towel or strap around one foot and gently pull the leg upward while keeping the other leg bent on the floor. This stretch targets the hamstrings and supports pelvic alignment, both of which contribute to hip joint mechanics. Similarly, the kneeling hip flexor stretch can relieve tightness in the front of the hip, a common source of pain and reduced mobility. By gently leaning forward in a lunge position with one knee on the ground, individuals can open the hip flexor while maintaining spinal alignment.
Each of these stretches should be performed with control and attention to body cues. Over time, consistent stretching enhances joint function and reduces reliance on pain medications, offering a sustainable, empowering solution for those with hip osteoarthritis. These exercises are also an important component of broader programs addressing exercises for arthritic knees and hips, which often benefit from a shared repertoire of movements focused on flexibility and alignment.
Integrating Physiotherapy for Hip Osteoarthritis Into Daily Life
Physiotherapy for hip osteoarthritis should not be confined to a clinical setting. To maximize its benefits, therapeutic strategies must be integrated into everyday life. This begins with establishing a daily routine that includes stretching, strengthening, and low-impact cardiovascular activity. Morning sessions are particularly helpful, as joints tend to be stiff upon waking. A short, gentle routine can prepare the body for the day and prevent pain flare-ups.
Working with a licensed physiotherapist provides tailored guidance and ongoing assessment to ensure that progress is steady and safe. Physiotherapists also employ modalities such as manual therapy, ultrasound, and neuromuscular reeducation to complement exercise-based interventions. Beyond the clinic, everyday tasks present opportunities for therapeutic movement. For instance, rising from a chair without using hands can activate hip stabilizers, while taking the stairs instead of the elevator promotes functional strength and endurance.
Equally important is the creation of a supportive environment. Wearing shoes with adequate arch support, using ergonomic seating, and avoiding prolonged static positions all contribute to joint health. These small changes, when combined with regular exercises for arthritic knees and hips, form a comprehensive lifestyle approach that mitigates pain and promotes sustained independence.
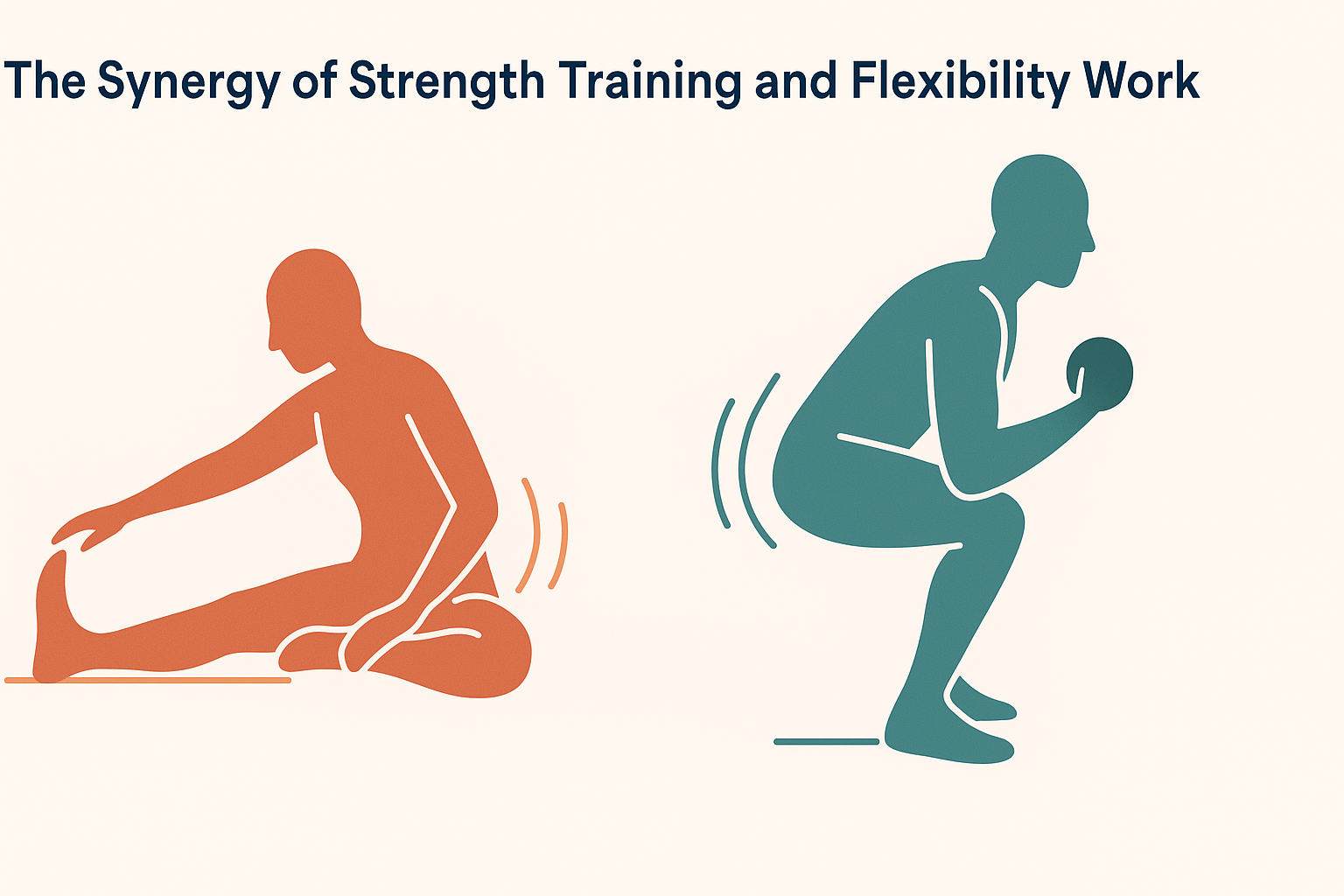
The Synergy of Strength Training and Flexibility Work
While stretching provides immediate relief and improved flexibility, it is most effective when paired with strength training. Weak muscles contribute to joint instability and increase the likelihood of injury. For individuals with hip osteoarthritis, strengthening the glutes, quadriceps, and core muscles helps stabilize the hip joint and reduce compensatory movements that can strain other areas.
Incorporating strength exercises such as bridges, clamshells, and mini-squats enhances muscle support around the hip and knee joints. These exercises should be performed under the guidance of a healthcare provider to ensure proper technique and avoid exacerbating symptoms. Resistance bands, light weights, and bodyweight movements offer scalable options for all fitness levels. Strength training not only complements hip osteoarthritis exercises but also supports exercises for arthritic knees and hips by building resilience throughout the lower body.
Moreover, strength training has been linked to improved bone density, metabolic health, and mood regulation. For individuals managing chronic pain, these systemic benefits create a positive feedback loop that reinforces commitment to consistent movement. The integration of both stretching and strengthening into a unified program represents a gold standard in physiotherapy for hip osteoarthritis.
Community, Support, and the Power of Shared Experience
Living with hip osteoarthritis can feel isolating, particularly when movement is limited or pain is invisible to others. Joining support groups—whether online or in-person—provides a sense of belonging and shared understanding. These communities offer practical tips, emotional validation, and inspiration from others who are actively managing similar challenges.
Social engagement itself has therapeutic value. Meaningful relationships buffer against the psychological effects of chronic pain and encourage physical activity. Walking groups, gentle yoga classes, or water aerobics sessions not only improve physical health but also nourish the human need for connection.
Healthcare providers play a critical role in fostering this sense of community by referring patients to appropriate resources, encouraging group-based therapies, and validating the emotional experience of chronic joint disease. In this way, the healing process becomes not just a solitary journey, but a shared path supported by empathy, expertise, and collective wisdom.
Holistic Approaches to Managing Osteoarthritis Pain
Stretching and physiotherapy are vital components of a larger, holistic approach to managing osteoarthritis. Nutrition, stress management, sleep hygiene, and mental health all intersect with physical health outcomes. An anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and lean proteins can reduce joint swelling and support tissue repair. Hydration is also key, as dehydrated tissues are more prone to stiffness and pain.
Mind-body practices such as yoga, tai chi, and guided meditation offer dual benefits of flexibility and mental relaxation. These modalities promote body awareness and help individuals respond more calmly to discomfort. They also incorporate breathing techniques and gentle movements that are safe for arthritic joints, reinforcing the benefits of structured hip osteoarthritis exercises.
Sleep, often overlooked, is critical for cellular regeneration and pain modulation. Establishing a regular sleep routine, reducing screen time before bed, and creating a comfortable sleep environment can significantly influence pain perception and energy levels. Emotional well-being, too, deserves attention. Chronic pain is closely tied to mood disorders such as anxiety and depression. Seeking support through counseling, peer groups, or integrative medicine can empower individuals to navigate their osteoarthritis journey with resilience and hope.
Encouraging Consistency Through Motivation and Mindset
One of the most significant challenges in managing osteoarthritis is maintaining long-term consistency with an exercise regimen. Motivation often wanes when results are not immediate, or when pain persists despite early efforts. However, adopting a mindset grounded in self-compassion and long-term vision is essential. Rather than striving for perfection, individuals should aim for progress, understanding that healing is a non-linear process.
Setting realistic, measurable goals can reinforce a sense of accomplishment. Tracking improvements in range of motion, pain levels, or activity tolerance provides tangible evidence of progress. Celebrating small milestones, such as walking farther or completing a stretch more comfortably, builds momentum and fosters a positive feedback loop.
Social support also plays a pivotal role. Joining exercise groups, whether in-person or virtual, creates accountability and camaraderie. Sharing experiences with others who are navigating similar challenges can be deeply validating and inspiring. Ultimately, the journey through hip osteoarthritis is deeply personal, but it need not be lonely. With the right tools, mindset, and support, consistent practice of physiotherapy for hip osteoarthritis becomes a powerful act of self-care and empowerment.
The Role of Professional Guidance in Long-Term Success
Though self-directed stretching routines can offer substantial benefits, professional guidance enhances safety and outcomes. A physical therapist brings a wealth of knowledge in biomechanics, pathology, and therapeutic interventions tailored to the individual’s condition. They can identify compensatory patterns that might hinder progress or lead to secondary injuries and can adapt the program based on feedback and evolving needs.
Moreover, physiotherapists often work in multidisciplinary teams, collaborating with rheumatologists, orthopedic surgeons, dietitians, and psychologists to provide comprehensive care. This integrative approach ensures that all dimensions of the patient’s well-being are addressed, not just the physical symptoms. By regularly reassessing progress and adjusting the treatment plan, professionals ensure that stretching and other hip osteoarthritis exercises remain aligned with the individual’s functional goals and evolving condition.
Investing in professional care also instills confidence. Knowing that one’s routine is backed by science and customized by an expert removes the guesswork and anxiety that often accompany chronic conditions. For many, this confidence translates into higher adherence, better outcomes, and a more optimistic outlook on the future.
Frequently Asked Questions: Advanced Insights on Hip Osteoarthritis Exercises and Joint Health
1. How can I tell if my current routine of hip osteoarthritis exercises is helping or potentially making things worse?
Monitoring your body’s response is essential when practicing hip osteoarthritis exercises. Progress is typically indicated by a gradual increase in mobility, reduction in stiffness upon waking, and the ability to perform daily activities with greater ease. However, if pain consistently intensifies during or after your sessions, or if swelling and joint warmth occur, it may signal the need to adjust your regimen. It’s crucial to track how your body responds over several days, as delayed-onset soreness may sometimes be mistaken for injury. Consulting a physiotherapy for hip osteoarthritis specialist can help fine-tune your program based on movement patterns and functional outcomes rather than pain levels alone.
2. Are there any overlooked muscle groups that should be prioritized in hip osteoarthritis rehabilitation?
Yes, while most routines focus on primary movers like the glutes and hip flexors, deeper stabilizing muscles such as the transverse abdominis and pelvic floor often go neglected. These core muscles are vital for postural integrity and pelvic alignment, both of which significantly impact hip joint function. Engaging these areas through breathwork, pelvic tilts, and controlled isometrics can enhance the effectiveness of hip osteoarthritis exercises. When these stabilizers are weak or underactive, compensatory strain may shift to the knees or lumbar spine. Therefore, well-rounded physiotherapy for hip osteoarthritis should always integrate core stabilization and neuromuscular reeducation for comprehensive support.
3. How do exercises for arthritic knees and hips differ from those for general joint maintenance?
Exercises for arthritic knees and hips are tailored with specific limitations and inflammatory responses in mind. Unlike general fitness routines, they emphasize controlled range of motion, joint offloading, and muscle activation without excessive load. The pace, intensity, and angles used must all be adapted to avoid triggering pain. Moreover, they prioritize joint-specific neuromuscular coordination and proprioception, which are often impaired in osteoarthritis. In physiotherapy for hip osteoarthritis, for instance, exercises often start in non-weight-bearing positions and progress gradually to functional, upright movements.
4. What role does sleep posture play in the effectiveness of hip osteoarthritis exercises?
Sleep posture has a surprisingly strong influence on hip joint health and the benefits of exercise. Poor alignment during rest can negate the day’s efforts in stretching and strengthening, especially if the hip remains in a flexed or rotated position for hours. For optimal recovery, it is recommended to sleep on your back with a pillow under the knees or on the non-affected side with a cushion between the legs. This reduces pressure and supports spinal alignment, which in turn enhances the outcomes of your hip osteoarthritis exercises. Physiotherapy for hip osteoarthritis may even include sleep education as part of a comprehensive care plan.
5. Can wearable technology be used to enhance physiotherapy for hip osteoarthritis?
Absolutely. Wearable devices such as smart bands, posture correctors, or even mobile apps that track joint angles are becoming popular adjuncts to physiotherapy for hip osteoarthritis. These technologies can offer real-time feedback on gait symmetry, movement patterns, and adherence to exercise prescriptions. They are particularly useful for home-based rehabilitation, where professional supervision is limited. By tracking progress objectively, these tools help tailor hip osteoarthritis exercises to individual needs while increasing patient engagement. Furthermore, some apps integrate reminders, video demonstrations, and pain diaries, which improve long-term adherence.
6. How do psychological factors influence the success of hip osteoarthritis exercises?
Mental and emotional resilience play a major role in rehabilitation success. Patients who experience high levels of anxiety or depression often perceive greater pain intensity and may be less consistent with exercise routines. This is where cognitive behavioral strategies or mindfulness practices can significantly support the physical aspects of care. By reframing pain not as a threat but as a manageable signal, individuals are more likely to continue their exercises for arthritic knees and hips even during flare-ups. Incorporating stress-reduction techniques into physiotherapy for hip osteoarthritis often results in better functional outcomes and improved quality of life.
7. Is it safe to perform hip osteoarthritis exercises during flare-ups?
During a flare-up, it is essential to modify but not completely halt activity. Resting entirely may worsen stiffness and prolong recovery. Gentle mobility work, such as pelvic tilts or aquatic therapy, can maintain joint function without exacerbating inflammation. Ice application post-activity and anti-inflammatory nutrition can further support healing. Adjusting the frequency, duration, or type of physiotherapy for hip osteoarthritis during these periods can prevent regression while respecting the body’s temporary limitations. The key is staying active within a pain-free range to avoid deconditioning.
8. Are there specific environmental factors that can improve or hinder the effectiveness of exercises for arthritic knees and hips?
Yes, both indoor and outdoor environments can influence joint rehabilitation. Flooring type, for instance, can impact joint loading; exercising on hard, unyielding surfaces may increase pain, whereas padded mats or carpeted areas offer more support. Ambient temperature also plays a role—warm environments tend to promote muscle elasticity and joint lubrication, improving exercise tolerance. On the other hand, cold or damp conditions can stiffen joints and limit flexibility. Physiotherapy for hip osteoarthritis often includes advice on optimizing environmental settings to ensure safer and more effective sessions.
9. What emerging trends in physiotherapy for hip osteoarthritis could redefine traditional treatment models?
Innovations like virtual reality (VR) rehabilitation, biofeedback-based neuromuscular training, and AI-powered posture analysis are reshaping physiotherapy for hip osteoarthritis. These technologies offer immersive and interactive ways to engage patients while enhancing precision in movement correction. They also allow for remote therapy options, making high-quality care more accessible. Additionally, regenerative therapies, such as platelet-rich plasma (PRP) injections, though still under investigation, are being combined with hip osteoarthritis exercises to potentially enhance tissue repair. These trends suggest a future where rehabilitation is increasingly personalized, tech-driven, and integrative.
10. How can caregivers and family members support someone engaging in exercises for arthritic knees and hips?
Caregivers play a vital role in facilitating consistent and safe exercise practices. Their involvement can range from helping set up safe exercise environments to providing gentle encouragement during daily routines. Education is key—caregivers should understand the goals and boundaries of the prescribed physiotherapy for hip osteoarthritis to avoid over-assistance or discouragement. They can also help monitor signs of fatigue or improper form, ensuring the exercises for arthritic knees and hips are executed effectively. Emotional support, such as acknowledging progress and fostering a positive mindset, further strengthens the rehabilitation process and contributes to long-term adherence.
Conclusion : Embracing Mobility Through Hip Osteoarthritis Exercises
The journey through hip osteoarthritis can be marked by moments of frustration and fatigue, but it is also rich with opportunities for empowerment, resilience, and renewed vitality. Stretching, when approached mindfully and supported by science, offers a gateway to improved flexibility, reduced pain, and a deeper connection with one’s body. More than a mechanical task, stretching becomes a ritual of self-respect, a daily affirmation that healing is possible.
By integrating physiotherapy for hip osteoarthritis into daily routines and complementing it with strength training, holistic wellness, and professional guidance, individuals reclaim agency over their health. These practices are not merely exercises for arthritic knees and hips—they are foundational tools for restoring function, maintaining independence, and living life fully in spite of arthritis. The path may be challenging, but with knowledge, consistency, and compassion, it becomes not only manageable but deeply meaningful.


