Recovering from a hamstring injury can be a physically and mentally taxing process. Whether caused by sports, overuse, or poor posture, hamstring injuries can significantly restrict movement and disrupt daily activities. However, targeted stretching and strengthening exercises can play a vital role in restoring flexibility, preventing reinjury, and ensuring long-term muscle health. This article explores evidence-based approaches to hamstring injury stretching and exercises, drawing from sports medicine, physical therapy, and biomechanics to deliver a medically accurate, SEO-optimized, and engaging guide suitable for the Health11News audience.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Understanding Hamstring Injuries and Their Impact on Movement
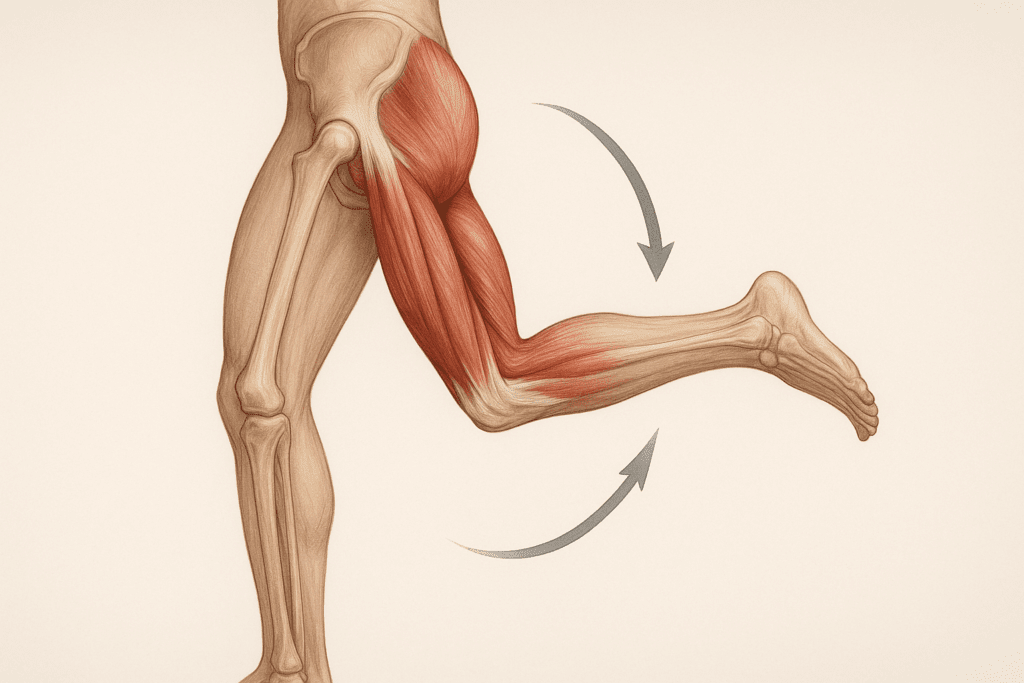
Hamstring injuries typically involve strains or tears of the muscles located at the back of the thigh. These muscles—the biceps femoris, semitendinosus, and semimembranosus—work together to bend the knee and extend the hip, making them essential for walking, running, and even sitting. When these muscles are overstretched or subjected to sudden force, they can become damaged, leading to pain, swelling, and reduced mobility. Mild strains might heal quickly with rest, while more severe injuries may require weeks or even months of rehabilitation.
Injury often occurs during high-speed activities such as sprinting, kicking, or jumping, particularly when the muscle is lengthening under tension—a process known as eccentric contraction. Repeated stress without proper conditioning can weaken the tissue, making it prone to tearing. Inadequate warm-ups, muscle imbalances, and fatigue are additional risk factors. Without proper rehabilitation, there is a high chance of reinjury, especially in the first few months following recovery. That is why a carefully structured program of hamstring injury stretching and targeted exercises is essential for a safe and complete return to function.
Why Stretching Is Crucial After a Hamstring Injury
Stretching helps realign collagen fibers as they heal, reducing the risk of scar tissue formation that can impair flexibility. More importantly, it restores the natural elasticity of the hamstring muscles, which is critical for efficient biomechanical function. However, stretching too soon or too aggressively can worsen the injury, so timing and technique are paramount. Early in recovery, stretching should be gentle and focus on pain-free range of motion. As healing progresses, more advanced flexibility exercises can be introduced under professional supervision.
Hamstring injury stretching should emphasize gradual elongation of the muscle fibers. Passive stretching, where the limb is supported and extended without muscular effort, is often the safest starting point. Over time, transitioning to active and dynamic stretches helps prepare the muscle for functional movements. Clinical studies have shown that consistent stretching—combined with strengthening—leads to better outcomes and fewer recurrences. For optimal results, stretching must be balanced with exercises that rebuild strength and coordination in the surrounding muscles.

Best Hamstring Injury Exercises to Support Safe Recovery
While stretching is vital, rehabilitation also hinges on a comprehensive exercise plan. Strengthening exercises help restore muscular balance, reduce stress on healing tissue, and promote neuromuscular control. Initially, exercises should be isometric, focusing on contracting the muscle without changing its length. These moves activate muscle fibers without placing undue strain on the healing tissue. As strength returns, concentric and eccentric movements can be introduced to build resilience and reduce reinjury risk.
For example, a commonly recommended progression includes hamstring sets, where the muscle is gently contracted while the leg remains stationary. This can be followed by heel digs and bridges, which gently engage the posterior chain. As healing advances, more dynamic exercises such as single-leg Romanian deadlifts, resisted leg curls, and Nordic hamstring curls can be incorporated. These exercises challenge the hamstrings through their full range of motion and are especially effective in restoring strength lost during injury.
Integrating Functional Movement Patterns During Rehabilitation
One of the most overlooked aspects of hamstring injury recovery is functional movement training. Rehabilitating the hamstring in isolation is not enough; the muscle must be reintegrated into movement patterns used in everyday activities and sports. Exercises should mimic real-life tasks and promote coordination between the hamstrings and surrounding muscles, such as the glutes, calves, and core.
Lunges, squats, and step-ups are excellent examples of functional movements that engage multiple muscle groups. When performed with proper form, they enhance movement efficiency and reduce compensatory patterns that could lead to further injury. Using resistance bands or balance tools can add complexity and improve proprioception. Functional training ensures the injured area does not become a weak link in the kinetic chain, allowing for a smooth transition back to athletic or occupational demands.

The Role of Yoga and Flexibility Training in Long-Term Prevention
Yoga offers a holistic approach to hamstring rehabilitation and long-term injury prevention. Gentle poses such as downward-facing dog, seated forward fold, and supine hamstring stretches promote flexibility while encouraging body awareness and breath control. These movements facilitate gradual tissue elongation and enhance joint mobility without overstressing the muscle.
Yoga also cultivates muscular balance and symmetry, helping to correct imbalances that may have contributed to the original injury. Poses that strengthen the glutes and core—such as bridge pose, warrior series, and chair pose—support the hamstrings during dynamic movement. Incorporating yoga into a hamstring injury stretching routine provides a low-impact method to maintain flexibility, reduce tension, and build mental focus during recovery.
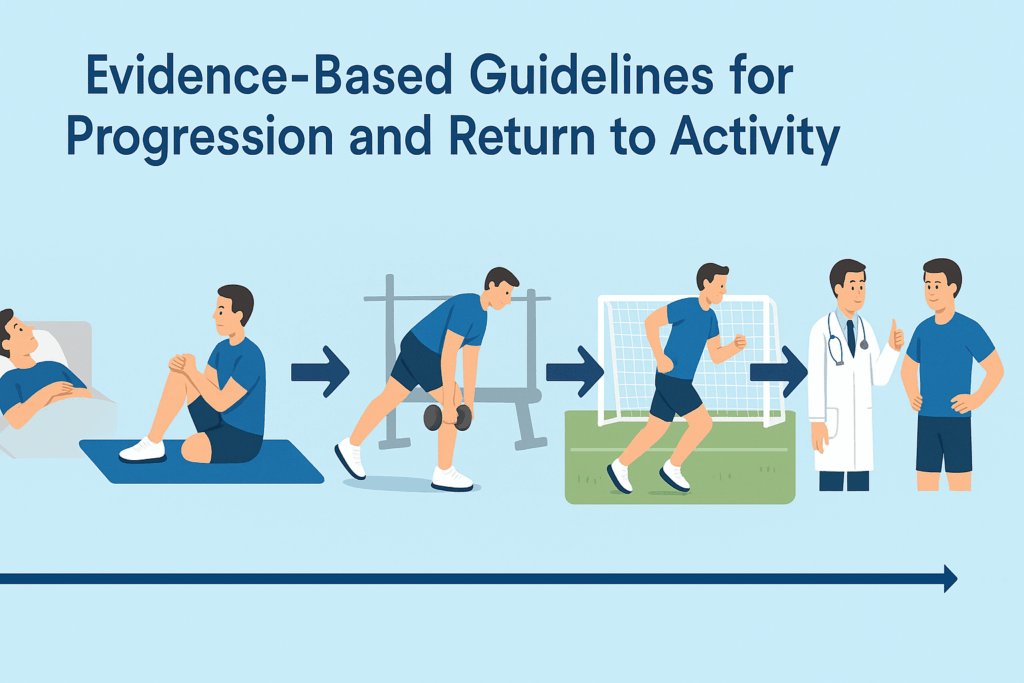
Evidence-Based Guidelines for Progression and Return to Activity
Determining when and how to progress during rehabilitation requires careful monitoring of pain, strength, and functional capacity. Research suggests that return to activity should only occur when the injured leg can perform at least 90% of the strength and flexibility of the uninjured side. This benchmark helps ensure that the muscle has healed sufficiently to withstand the forces of sport or daily activity.
Key indicators of readiness include the ability to walk, jog, and perform light jumps without pain or compensation. Functional tests, such as single-leg hop tests or isokinetic strength assessments, can provide objective data. Progression should follow a gradual pattern, with new exercises introduced incrementally and always within a pain-free range. Any return of discomfort signals the need to regress or modify the program.
Preventive strategies include ongoing hamstring injury exercises and regular flexibility sessions. Maintenance work is especially important during periods of high activity or when resuming intense physical training. Educating patients and athletes on proper warm-up, hydration, and sleep hygiene further supports injury prevention.
Common Mistakes to Avoid During Hamstring Rehabilitation
Despite best intentions, many individuals make critical mistakes during hamstring recovery that can delay healing or cause reinjury. One of the most frequent errors is returning to activity too soon. The absence of pain does not necessarily mean the tissue has fully healed, and premature stress can reopen partially healed fibers. Rushing the rehabilitation process, skipping essential exercises, or ignoring flexibility can undermine months of progress.
Another common issue is neglecting the surrounding muscle groups. The hamstrings do not work in isolation, and failing to strengthen the glutes, core, and hip stabilizers can lead to muscular imbalances and compensatory movements. In some cases, individuals rely solely on static stretching, overlooking the importance of eccentric and functional training. This creates an illusion of readiness without the muscular resilience needed to prevent reinjury.
Lastly, poor form and technique during exercises can compromise outcomes. Whether lifting weights or performing yoga, movement should always be deliberate and aligned. Working with a physical therapist or qualified trainer can provide essential feedback and ensure that each phase of recovery aligns with medical best practices.
Tailoring Hamstring Injury Stretching to Individual Needs
Not all hamstring injuries are the same, and rehabilitation should reflect the specific severity, location, and cause of the injury. For instance, proximal hamstring tendinopathy—a condition affecting the upper part of the muscle near the glutes—requires a different approach than a mid-belly strain. Similarly, injuries resulting from sprinting may demand more emphasis on eccentric control than those stemming from poor flexibility.
Age, fitness level, and lifestyle factors also influence recovery. An elite sprinter may need a more aggressive timeline and sport-specific training, while an older adult recovering from a slip may benefit from slower progression and balance-focused work. Listening to the body and adjusting the intensity, volume, and type of hamstring injury exercises and stretch routines is key to effective healing. Individualized plans—ideally developed in collaboration with healthcare providers—offer the best outcomes.
How to Build a Sustainable Hamstring Maintenance Program
Once an individual has successfully recovered from a hamstring injury, it is crucial to adopt long-term strategies to maintain strength and flexibility. A sustainable program includes regular stretching, particularly after workouts or long periods of sitting. Gentle hamstring injury stretching can be incorporated into warm-ups and cooldowns to preserve muscle elasticity and reduce post-exercise tightness.
Maintenance exercises should include eccentric drills such as Nordic curls or single-leg glides, which have been shown to reduce the incidence of future injuries. Foam rolling and self-myofascial release techniques can help relieve residual tension and improve blood flow. Periodic reassessments with a physical therapist or sports medicine professional ensure that the program continues to meet the evolving needs of the individual.
Additionally, paying attention to recovery practices—such as sleep, nutrition, hydration, and mental health—can enhance physical resilience. Muscle health is interconnected with overall wellness, and neglecting one aspect can create vulnerabilities. By integrating hamstring injury exercises, stretch routines, and lifestyle practices into a cohesive plan, individuals can protect themselves against future setbacks.
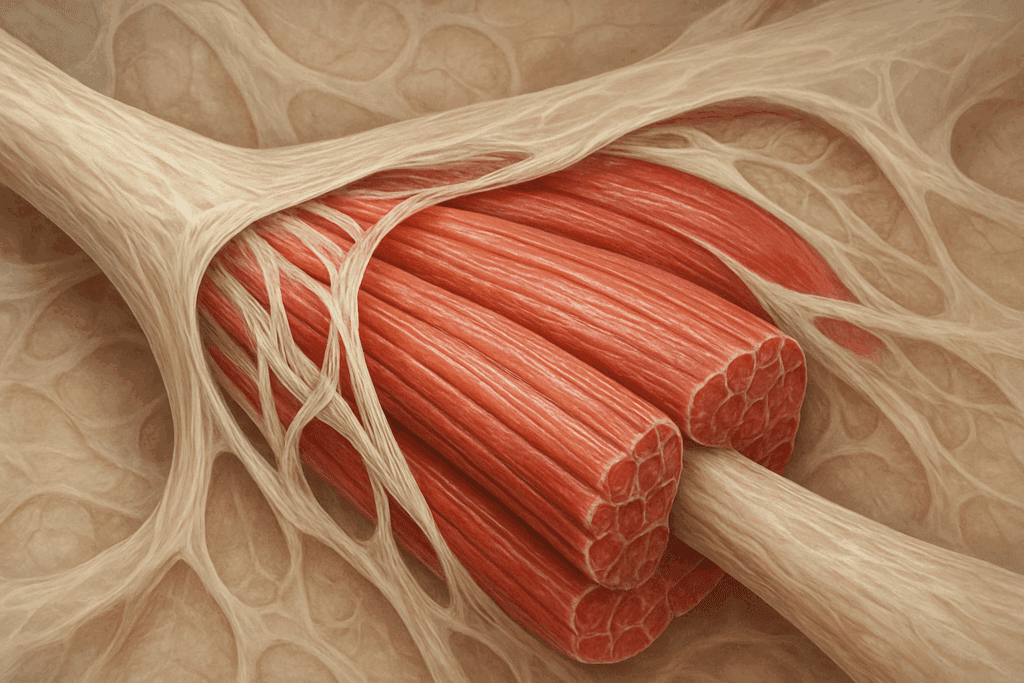
The Connective Tissue Matrix: More Than Just Muscle
Hamstring injuries don’t affect muscle tissue alone—they also involve disruption in the surrounding connective tissue matrix, including tendons, fascia, and intramuscular septa. Tendons are particularly susceptible to degeneration following strain, especially at the musculotendinous junction. In these areas, collagen fibers often become disorganized, and capillary density may decline, impeding the healing process. Understanding the biomechanics of tendons helps clarify why stretching alone is insufficient for full recovery.
Emerging research shows that myofascial connections significantly influence both injury and recovery. Fascia, the web-like connective tissue encasing muscles, transmits force across muscle groups and stores elastic energy during movement. When fascia is restricted—due to injury, inactivity, or scar tissue formation—it alters the mechanical properties of the muscle. Techniques such as myofascial release, foam rolling, and instrument-assisted soft tissue mobilization (IASTM) are increasingly incorporated into rehabilitation protocols to improve fascial glide and restore kinetic chain efficiency.
Hamstring injuries can also provoke changes in the extracellular matrix (ECM), the cellular scaffolding that supports muscle repair. ECM remodeling is essential for tissue regeneration, but excessive fibrosis can stiffen the muscle and restrict function. Targeting ECM health through hydration, anti-inflammatory nutrition, and therapeutic movement is an emerging area of interest in sports medicine.
The Science of Muscle Regeneration and Satellite Cells
Muscle repair is orchestrated by satellite cells—muscle stem cells that activate after injury to regenerate damaged fibers. When stimulated, these cells proliferate and fuse with existing muscle fibers, contributing new nuclei to support protein synthesis and repair. Satellite cell activity is highest during the initial weeks after injury and can be influenced by mechanical loading, nutritional status, and hormonal environment.
Overtraining, chronic inflammation, and nutritional deficiencies can impair satellite cell activation, prolonging recovery. For this reason, rehabilitation must include not only physical therapy but also lifestyle factors that support regenerative biology. Adequate protein intake, vitamin D sufficiency, and sleep quality all enhance the activity of these critical cells. Mechanical stimulation through eccentric loading and neuromuscular reeducation further promotes the favorable activation of satellite cells.
Interestingly, older adults exhibit lower satellite cell density and regenerative potential compared to younger individuals. This underscores the need for age-specific rehabilitation strategies and highlights the importance of early intervention to prevent long-term muscle dysfunction. Therapies such as blood flow restriction (BFR) training, which simulates the effects of high-load strength training at lower intensities, have shown promise in enhancing muscle protein synthesis and satellite cell activation, especially in deconditioned or aging populations.
Biomechanical Risk Factors and Asymmetry in Movement
Many hamstring injuries stem not from sudden trauma alone, but from underlying biomechanical dysfunctions. Hip extension limitations, anterior pelvic tilt, and weak gluteal activation all contribute to compensatory hamstring overload. In fact, kinematic studies have shown that individuals who rely heavily on their hamstrings for hip extension—due to glute weakness—experience higher eccentric stress and are more likely to suffer recurring injuries.
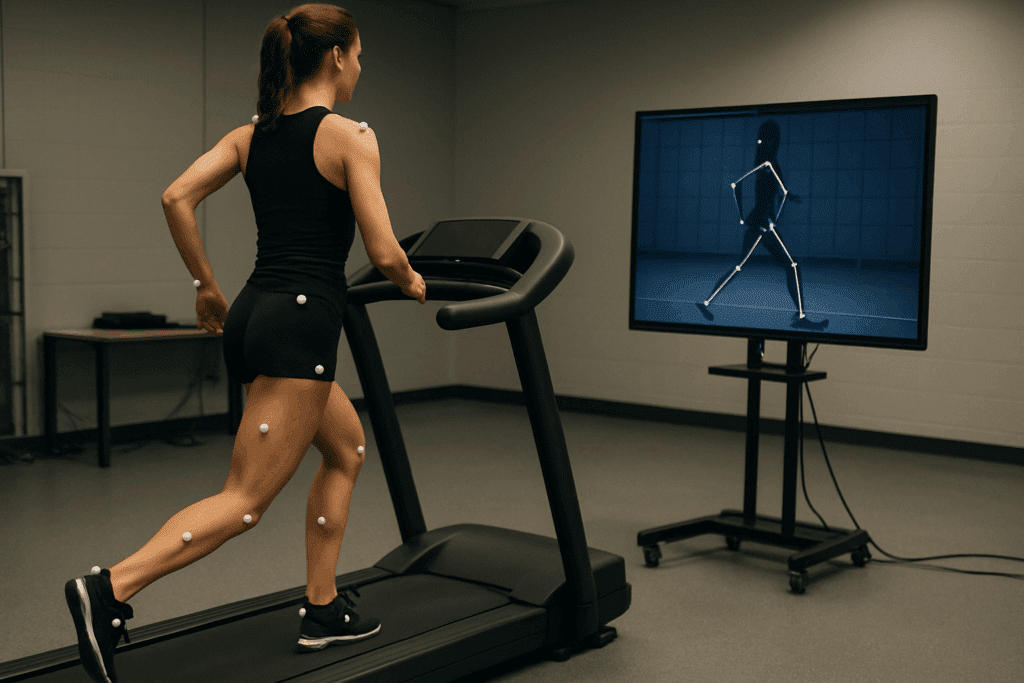
Gait analysis and video assessment can help identify movement patterns that predispose an individual to hamstring strain. Common dysfunctions include overstriding during running, limited knee drive, and excessive lumbar extension during acceleration. Addressing these issues requires more than strengthening the hamstrings—it demands a comprehensive strategy targeting the glutes, core, and spinal stabilizers.
Pelvic control is a critical yet often overlooked component. When the pelvis is unstable or anteriorly tilted, the hamstrings are placed under constant tension, especially during sprinting and deceleration. Strengthening the deep core, particularly the transverse abdominis and pelvic floor, can help neutralize pelvic posture and reduce unwanted hamstring strain.
What the Latest Research Says About Reinjury and Prevention
Scientific research on hamstring rehabilitation has advanced significantly in recent years. Studies have identified eccentric training as one of the most effective strategies for reducing reinjury rates. This form of exercise challenges the muscle as it lengthens under tension, preparing it for the specific forces experienced during sprinting and other high-intensity activities. Programs that incorporate eccentric loading—such as the Nordic hamstring protocol—have shown a dramatic reduction in hamstring injury recurrence.
Additionally, research supports the role of neuromuscular training, which enhances coordination between the brain and muscles. Exercises that challenge balance, reaction time, and proprioception help retrain movement patterns and prevent compensatory habits that can stress the hamstrings. Combining strength, flexibility, and neuromuscular training provides a comprehensive approach that addresses the multifactorial nature of injury risk.
Technological innovations, including motion analysis, ultrasound imaging, and isokinetic testing, allow for more precise assessments and individualized care plans. These tools help clinicians monitor progress, identify deficits, and tailor rehabilitation protocols more effectively. As our understanding of biomechanics and tissue healing evolves, so too do the methods available for safe and complete hamstring recovery.
The Role of Inflammation and Systemic Healing in Hamstring Recovery
While localized inflammation is a natural part of tissue healing, chronic or excessive inflammation can impede recovery. After a hamstring strain, the body initiates an inflammatory cascade that clears damaged tissue and sets the stage for regeneration. However, if this response becomes dysregulated, it can result in prolonged pain, swelling, and limited range of motion.
Anti-inflammatory strategies should be tailored to the stage of healing. Early on, ice, compression, and elevation can help manage swelling. Later in the process, systemic interventions such as omega-3 fatty acids, curcumin, and polyphenol-rich diets may reduce chronic low-grade inflammation and support tissue repair. Overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) is discouraged, as they may blunt the natural healing cascade if taken indiscriminately during the acute phase.
Sleep also plays a crucial role in inflammation resolution. Deep sleep stages are associated with increased growth hormone release and improved tissue regeneration. Patients recovering from hamstring injuries should prioritize sleep hygiene, stress management, and recovery rituals that support their physiological healing environment.
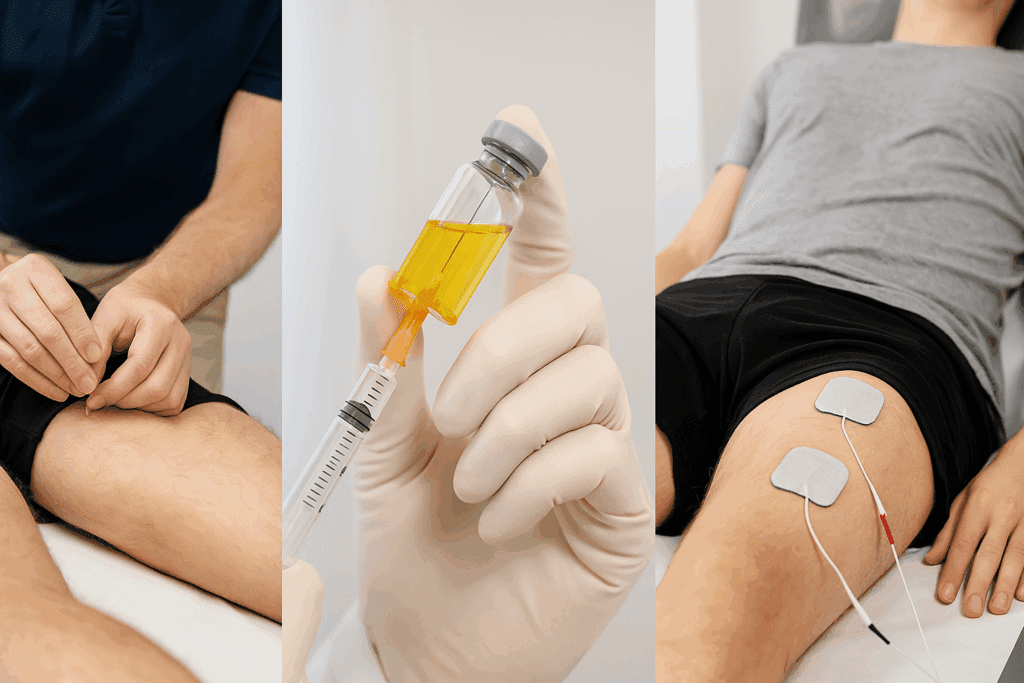
Emerging Therapies: PRP, Dry Needling, and NMES
Advanced therapies are increasingly being explored to accelerate hamstring injury recovery. Platelet-rich plasma (PRP) therapy, for instance, involves injecting concentrated growth factors derived from the patient’s own blood directly into the injury site. These growth factors stimulate tissue repair, angiogenesis, and collagen synthesis. While evidence is still emerging, early studies suggest PRP may reduce recovery time in select cases of hamstring strains, particularly grade II injuries.
Dry needling is another technique gaining popularity. Unlike acupuncture, which follows traditional Chinese medicine meridians, dry needling targets trigger points in muscle tissue to release tension, reduce pain, and improve neuromuscular function. When applied by a skilled practitioner, it may help deactivate chronically tight areas within the hamstrings, allowing for better muscle firing and improved range of motion.
Neuromuscular electrical stimulation (NMES) can also play a role in post-injury rehabilitation. By delivering low-voltage electrical currents to the hamstring, NMES helps stimulate contractions, preserve muscle mass, and reestablish motor unit recruitment. This technique is particularly useful in the early phases of recovery when voluntary activation is limited by pain or neural inhibition.
Recovery Timelines and the Psychological Impact of Hamstring Injury
The timeline for recovering from a hamstring injury varies widely depending on severity, age, baseline fitness, and adherence to rehabilitation. Grade I injuries may heal in 1 to 3 weeks, while Grade II and III injuries can take several months. Unfortunately, reinjury rates remain high—especially in athletes—if return-to-play criteria are not met or if biomechanical flaws remain unaddressed.
Equally important is the psychological impact of injury. Athletes recovering from hamstring strains often experience fear of reinjury, performance anxiety, and reduced confidence in their physical capabilities. This can lead to altered movement patterns, delayed healing, and even avoidance of sport. Psychological support, including sports psychology consultations or cognitive behavioral strategies, may be helpful in navigating these challenges.
Mind-body practices such as meditation, breathwork, and visualization are valuable tools for building resilience during the recovery process. These practices can modulate the stress response, improve pain perception, and enhance focus—benefits that go beyond the physical dimensions of healing. Integrating both physiological and psychological care into the rehabilitation process fosters a more complete and sustainable recovery.
Frequently Asked Questions (FAQ): Advanced Insights on Hamstring Injury Recovery
1. Can poor sleep quality really impact your recovery from a hamstring injury?
Yes, sleep quality plays a surprisingly pivotal role in hamstring recovery. During deep sleep, the body releases growth hormone and enhances protein synthesis—both of which are essential for repairing muscle tissue and reducing inflammation. Individuals who neglect sleep hygiene may experience prolonged soreness, reduced strength gains from rehabilitation, and even impaired flexibility. When incorporating hamstring injury stretching into your routine, optimizing sleep helps the tissues adapt and heal more efficiently. Additionally, improved sleep enhances cognitive performance and neuromuscular coordination, supporting better results from your hamstring injury exercises and stretch protocols.
2. How can hydration influence the effectiveness of hamstring rehabilitation?
Hydration affects everything from muscle elasticity to fascial glide. Dehydrated tissues are more prone to stiffness, making it harder to achieve effective results from hamstring injury stretching sessions. Proper fluid balance also supports blood flow, oxygen delivery, and waste removal—key elements in muscle regeneration and inflammation reduction. During rehabilitation, especially when integrating eccentric hamstring injury exercises and stretch routines, consistent hydration improves recovery response and tissue pliability. Athletes and active individuals should also consider electrolyte replenishment post-workout to maintain optimal fluid balance.
3. Are there psychological effects of hamstring injuries that influence physical recovery?
Absolutely—fear of reinjury, frustration with limitations, and anxiety about performance can significantly hinder physical healing. These mental barriers may subtly alter posture, muscle activation patterns, and even commitment to rehabilitation. For example, someone hesitant to re-engage in hamstring injury stretching may subconsciously reduce their range of motion, delaying flexibility gains. Similarly, lack of confidence can limit intensity during functional hamstring injury exercises and stretch-based drills. Incorporating sports psychology techniques, such as visualization and graded exposure therapy, can support emotional resilience and accelerate both mental and physical progress.
4. Can nutrition enhance the results of hamstring injury exercises and stretch routines?
Targeted nutrition supports muscle recovery at the cellular level. Amino acids like leucine stimulate muscle protein synthesis, while micronutrients such as magnesium and zinc aid in connective tissue repair. Antioxidant-rich foods—such as berries, leafy greens, and turmeric—can reduce chronic inflammation and facilitate collagen turnover. When following a structured plan of hamstring injury exercises and stretch sessions, a nutrient-dense diet can accelerate tissue remodeling and reduce post-exercise soreness. Tailoring macronutrient intake to match energy demands also ensures that rehabilitation progresses smoothly without compromising overall health.
5. How do wearable technologies influence hamstring injury prevention and recovery?
Smart wearables can track biomechanical efficiency, muscle activation, and fatigue in real time, offering valuable insights for personalized rehab. Devices that monitor stride length, symmetry, and joint angles help identify imbalances that may not be visible to the naked eye. Integrating this data allows clinicians to fine-tune hamstring injury stretching routines and dynamically adjust exercise intensity. For instance, if an athlete’s wearable shows reduced posterior chain engagement during a run, the program can pivot to focus on glute and hamstring activation. Such tech enhances the precision of hamstring injury exercises and stretch protocols by adapting to individual movement patterns.
6. Can foam rolling be used as a substitute for hamstring injury stretching?
While foam rolling complements stretching, it should not replace it. Foam rolling works primarily on the fascia and superficial muscle layers, enhancing blood flow and reducing neural tension. However, it does not provide the controlled, progressive elongation necessary to restore full muscle length and joint range. For a comprehensive approach, foam rolling is best used prior to or after structured hamstring injury stretching sessions to enhance tissue readiness. When paired correctly, it supports improved outcomes from both hamstring injury exercises and stretch techniques, especially in reducing post-workout stiffness.
7. How does cold exposure therapy affect hamstring recovery protocols?
Cold exposure—whether through cryotherapy chambers or ice baths—can help reduce acute inflammation and alleviate soreness after intense rehabilitation sessions. However, excessive cold application may impair muscle regeneration if used immediately after strength-based hamstring injury exercises. It’s generally more effective when applied between sessions or during recovery days. Some protocols alternate cold and heat therapies to enhance circulation while managing pain. Importantly, cold exposure should not replace hamstring injury stretching but rather support it by minimizing discomfort and allowing better participation in active rehab.
8. Are there specific types of yoga that benefit hamstring injury rehabilitation more than others?
Gentle styles like restorative or Iyengar yoga are often more beneficial during early rehabilitation because they emphasize alignment, breath control, and support through props. These styles allow for sustained, low-intensity poses that complement hamstring injury stretching without risking overstretching. As recovery advances, practices like vinyasa can be introduced to enhance dynamic flexibility and neuromuscular coordination. When integrated into a routine of hamstring injury exercises and stretch therapy, yoga improves postural alignment and body awareness. This, in turn, reduces compensatory movement patterns that may increase reinjury risk.
9. How does long-term desk work influence hamstring injury recurrence?
Sedentary work contributes to shortened hip flexors and weakened glutes, placing constant passive tension on the hamstrings. Over time, this imbalance can increase the load during daily movements or workouts, making reinjury more likely. Integrating micro-mobility breaks, including short bouts of hamstring injury stretching, helps reset tissue length and activate underused muscles. Even small modifications—like sitting on a stability ball or using a standing desk—can promote better posture and hamstring alignment. For those engaged in desk work, combining these changes with hamstring injury exercises and stretch regimens ensures more sustainable recovery.
10. Are there seasonal or environmental factors that influence hamstring injury risk and recovery?
Cold temperatures reduce tissue elasticity, increasing the likelihood of muscle strains—especially in individuals who skip warm-ups. In winter or air-conditioned environments, longer preparation periods and more intensive warm-up stretches are essential before engaging in hamstring injury exercises and stretch movements. Humidity and dehydration can also impair neuromuscular performance, leading to compromised form. Outdoor athletes may benefit from adjusting session times to avoid temperature extremes and optimize tissue response. By accounting for environmental influences and adjusting hamstring injury stretching strategies accordingly, athletes and active individuals can protect against seasonal setbacks and improve recovery consistency.
Conclusion : Why Targeted Hamstring Injury Stretching and Exercises Are Essential for Long-Term Recovery and Performance
Recovering from a hamstring injury is about more than just relieving pain; it involves rebuilding the strength, flexibility, and function necessary to thrive in movement. Targeted hamstring injury stretching helps restore range of motion and prevent scar tissue formation, while progressive, functional exercises build the muscle’s capacity to withstand real-world demands. Together, these components form the foundation for long-term recovery and athletic performance.
Preventing reinjury requires ongoing attention to both the injured area and the entire kinetic chain. From dynamic warm-ups and yoga-inspired flexibility training to eccentric strength work and functional movement patterns, a well-rounded plan offers the best protection against setbacks. By listening to the body, working with professionals, and embracing a holistic approach, individuals can safely return to activity and stay there.
Ultimately, the journey from injury to full function is one of consistency, education, and patience. The right combination of hamstring injury exercises and stretch routines—executed with intention and medical guidance—can not only restore movement but elevate overall health and vitality for years to come.
Further Reading:
Hamstring Strain: Rehab Exercises


