Cognitive Behavioral Therapy (CBT) has long been celebrated as one of the most effective and evidence-based psychological interventions for a wide range of mental health conditions. Its flexibility and adaptability have allowed clinicians to develop multiple specialized forms of CBT, each fine-tuned to address the nuances of specific psychological disorders and personal needs. As our understanding of human cognition, behavior, and emotional functioning has evolved, so too have the different types of CBT. This growing diversity reflects the field’s commitment to personalized care, making CBT not just a technique, but a dynamic, evolving framework for therapeutic growth. Understanding the different types of cognitive behavioral therapy offers crucial insight into how tailored treatments can significantly enhance mental health outcomes across various populations and diagnoses.
You may also like: How Does CBT Work to Improve Relationships and Communication? Science-Backed Techniques for Getting Along with Others
The Foundation of Cognitive Behavioral Therapy
At its core, CBT is predicated on the idea that our thoughts, emotions, and behaviors are intricately interconnected. Maladaptive thinking patterns can reinforce negative emotions and lead to behaviors that perpetuate psychological distress. CBT seeks to break this cycle by helping individuals identify distorted cognitions, challenge them with evidence-based reasoning, and ultimately replace them with healthier, more constructive thought patterns. Traditional CBT, often referred to as “standard” or “generic” CBT, provides the basic structure for this process. It typically involves structured sessions, homework assignments, and the use of cognitive restructuring, behavioral experiments, and problem-solving techniques.
However, what makes CBT uniquely powerful is not just its foundational model, but its capacity for variation. Different types of CBT have emerged to meet the needs of diverse clinical populations, each maintaining the core tenets of cognitive restructuring and behavioral modification while integrating techniques specific to particular disorders or life circumstances. The refinement of these different types of cognitive behavioral therapy has made psychological care more responsive, targeted, and effective.
Behavioral Therapy Roots and the Evolution into CBT
To appreciate the various types of CBT, it helps to understand its historical roots in behavioral therapy. Early behavioral therapy focused exclusively on observable behavior, guided by principles of classical and operant conditioning. Techniques such as exposure therapy, systematic desensitization, and reinforcement schedules laid the groundwork for later cognitive models. Over time, the limitations of behaviorism—particularly its neglect of internal mental processes—prompted the integration of cognitive science, culminating in the cognitive revolution of the 1960s and 1970s. This shift gave rise to cognitive therapy, pioneered by Aaron Beck, and eventually to CBT as a comprehensive treatment model.
Today, behavioral therapy examples still abound within the CBT framework. Exposure therapy remains a cornerstone of treatment for anxiety disorders, while behavioral activation is widely used in the treatment of depression. These techniques continue to evolve as they are paired with cognitive interventions in modern forms of CBT. The synergy of cognitive and behavioral strategies underscores the strength of CBT and explains why the field has generated so many different types of CBT tailored to unique therapeutic goals.
Cognitive Therapy and Its Specializations
Cognitive therapy, as a distinct subcategory within the broader CBT umbrella, emphasizes the identification and modification of distorted thinking. While standard CBT often balances cognitive and behavioral components, some forms of cognitive therapy lean more heavily on the restructuring of thought patterns. These approaches are especially useful for individuals who struggle with pervasive cognitive distortions, such as catastrophizing, overgeneralization, and all-or-nothing thinking.
Specialized cognitive therapies have emerged to address specific mental health conditions. For example, Cognitive Therapy for Depression focuses on identifying negative automatic thoughts and underlying core beliefs that fuel depressive symptoms. Similarly, Cognitive Processing Therapy (CPT) for Post-Traumatic Stress Disorder helps clients reframe maladaptive trauma-related beliefs. These therapies show how different types of cognitive therapy can be adapted to fit the cognitive vulnerabilities of particular disorders, providing a more precise and individualized form of care.

Dialectical Behavior Therapy: A Mindful Evolution of CBT
Dialectical Behavior Therapy (DBT) represents a sophisticated evolution of CBT, particularly in its application to individuals with emotional dysregulation, self-harming behaviors, and borderline personality disorder. DBT retains the cognitive-behavioral commitment to skill-building but incorporates mindfulness, distress tolerance, interpersonal effectiveness, and emotion regulation strategies. Developed by Marsha Linehan, DBT responds to the unique therapeutic challenges of clients who experience intense emotional swings and interpersonal instability.
What sets DBT apart among the different types of CBT is its structured blend of acceptance and change. Rather than focusing solely on modifying dysfunctional thoughts, DBT teaches clients to validate their emotional experiences while also working toward behavioral change. This dual emphasis makes DBT a compelling example of how types of cognitive therapy can be enriched by philosophical and experiential components, enhancing engagement and treatment outcomes.

Acceptance and Commitment Therapy: Bridging Values and Behavior
Another prominent form of CBT that expands the traditional model is Acceptance and Commitment Therapy (ACT). ACT challenges the conventional CBT emphasis on disputing irrational beliefs. Instead, it promotes acceptance of difficult emotions and thoughts while encouraging commitment to actions aligned with personal values. ACT draws from relational frame theory and mindfulness practices, offering a unique framework that diverges from purely cognitive restructuring.
ACT is especially effective for individuals facing chronic pain, anxiety, or depression, where control strategies often exacerbate distress. By helping clients develop psychological flexibility—the ability to stay present with discomfort while acting in ways that reflect their values—ACT demonstrates how different types of cognitive behavioral therapy can adapt to the complex realities of human suffering. Its emphasis on experiential learning and values-based action distinguishes it from other types of CBT and highlights its relevance in contexts where traditional disputation techniques may fall short.
Exposure and Response Prevention: Precision Treatment for Anxiety and OCD
Exposure and Response Prevention (ERP) is a targeted CBT intervention primarily used to treat obsessive-compulsive disorder (OCD) and other anxiety-related conditions. ERP involves systematically exposing clients to anxiety-provoking stimuli while preventing the compulsive or avoidant behaviors that typically follow. This helps clients habituate to distressing thoughts or situations and reduces the reinforcing cycle of avoidance and compulsion.
ERP exemplifies the precision with which different types of CBT can be applied to specific symptom profiles. By focusing on behavioral exposure rather than cognitive disputation, ERP capitalizes on the mechanisms of extinction learning to produce lasting change. Its efficacy has been well-documented, particularly in the treatment of OCD, making it one of the most effective behavioral therapy examples in the CBT spectrum. ERP’s structured, evidence-based design highlights how different types of cognitive behavioral therapy can be rigorously tailored to address highly specific clinical needs.
Mindfulness-Based Cognitive Therapy: Integrating Awareness and Prevention
Mindfulness-Based Cognitive Therapy (MBCT) merges traditional cognitive therapy techniques with mindfulness meditation practices, creating a powerful tool for relapse prevention in recurrent depression. Originally developed by Zindel Segal, Mark Williams, and John Teasdale, MBCT teaches clients to observe their thoughts and feelings nonjudgmentally, reducing the likelihood of cognitive rumination and depressive relapse.
MBCT reflects a broader trend in which different types of CBT are integrated with contemplative traditions to enhance psychological resilience. Clients learn to decenter from negative thought patterns, cultivating a meta-awareness that interrupts automatic cognitive spirals. This blend of awareness and cognitive skill-building makes MBCT a valuable addition to the CBT landscape, especially for clients who have not responded fully to traditional approaches. The integration of mindfulness practices provides another compelling example of how different types of cognitive behavioral therapy can be adapted for long-term mental health maintenance.
Schema Therapy: Addressing Deep-Rooted Patterns
Schema Therapy takes CBT a step further by focusing on the enduring cognitive and emotional patterns, or “schemas,” that often develop early in life and shape adult functioning. These schemas can include deeply ingrained beliefs about oneself, others, and the world, often rooted in childhood experiences. Schema Therapy combines elements of cognitive, behavioral, psychodynamic, and attachment theories to address complex and treatment-resistant psychological issues.
This approach is especially beneficial for individuals with personality disorders, chronic depression, or relational difficulties that have not improved with conventional CBT. By working through core maladaptive schemas and providing corrective emotional experiences within the therapeutic relationship, Schema Therapy offers a powerful extension of CBT principles. It highlights how the different types of CBT can be expanded to address not just symptoms, but the underlying psychological structures that sustain them.
Compassion-Focused Therapy: Enhancing Emotional Safety
Compassion-Focused Therapy (CFT) introduces yet another dimension to the CBT tradition by emphasizing the cultivation of self-compassion as a means of reducing shame, self-criticism, and emotional avoidance. Developed by Paul Gilbert, CFT integrates principles of evolutionary psychology, affective neuroscience, and cognitive theory to address the biopsychosocial roots of emotional suffering.
CFT is particularly effective for individuals with high levels of internalized self-judgment, often seen in trauma survivors or those with histories of neglect. By helping clients develop a compassionate inner voice and practice self-soothing techniques, CFT complements more cognitively focused types of CBT. Its emphasis on emotional warmth, safety, and validation serves as a reminder that behavioral therapy examples can be profoundly healing when they are grounded in empathy and attuned to the human need for connection.
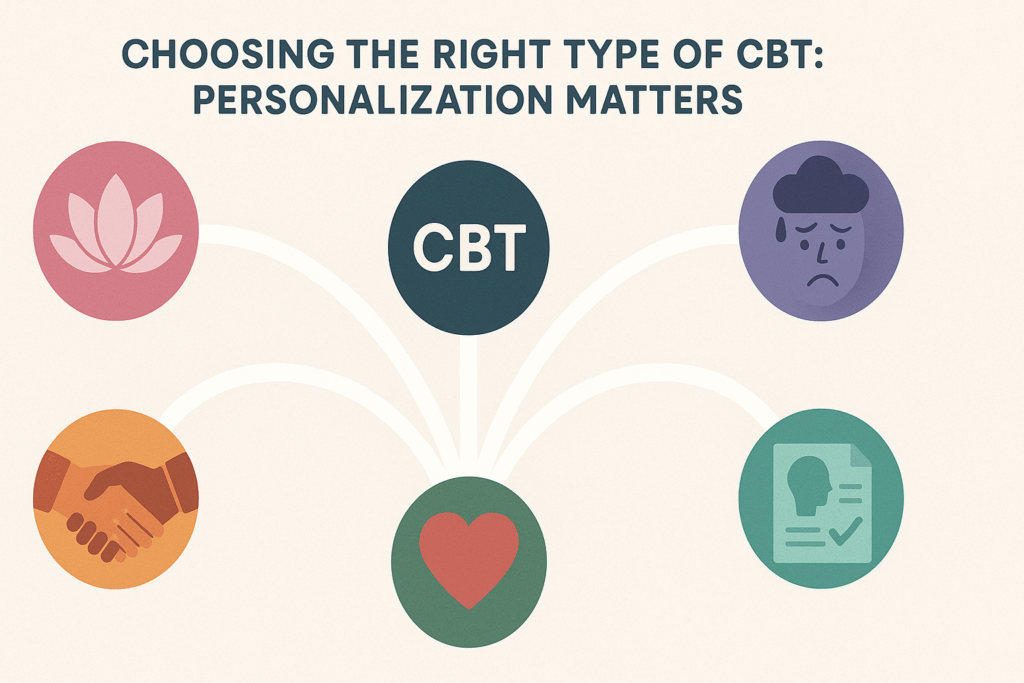
Choosing the Right Type of CBT: Personalization Matters
With so many different types of CBT available, the process of selecting the most appropriate intervention depends on a range of factors including the client’s diagnosis, therapeutic goals, personality, and cultural background. For some individuals, a standard cognitive-behavioral approach focused on distorted thinking may suffice. For others, a more experiential or values-driven model like ACT or DBT may be better suited. The clinician’s expertise and the therapeutic alliance also play a crucial role in determining which modality will yield the best results.
Importantly, these different types of cognitive behavioral therapy are not mutually exclusive. In practice, clinicians often integrate elements from multiple models to create a flexible and responsive treatment plan. This hybridization allows therapists to meet clients where they are, drawing from the rich repertoire of behavioral therapy examples to deliver care that is both scientifically grounded and deeply humane. The adaptability of CBT across contexts underscores its enduring relevance in a rapidly changing mental health landscape.
Frequently Asked Questions (FAQ): Advanced Insights into the Different Types of CBT
1. How do different types of CBT adapt to neurodiverse individuals, such as those with autism or ADHD?
Cognitive behavioral therapy has evolved significantly to meet the needs of neurodivergent individuals, particularly those on the autism spectrum or with ADHD. Among the different types of CBT, adaptations often include increased structure, visual aids, and emphasis on concrete thinking rather than abstract reflection. For example, CBT for ADHD may incorporate behavioral therapy examples like reward systems, environmental structuring, and impulse control techniques rooted in executive functioning frameworks. In contrast, individuals with autism may benefit from types of cognitive therapy that emphasize social stories, role-playing, and explicit emotional labeling to enhance social understanding. These tailored interventions show that different types of cognitive behavioral therapy can accommodate cognitive variance without diluting therapeutic rigor.
2. Can the types of CBT used in chronic illness management differ from those used for anxiety or depression?
Yes, different types of CBT are increasingly specialized for patients dealing with chronic illnesses like fibromyalgia, irritable bowel syndrome (IBS), or autoimmune disorders. In these cases, CBT emphasizes pain perception, fatigue management, and resilience training rather than the classic restructuring of distorted thoughts. Certain types of cognitive therapy, such as acceptance-based CBT or mindfulness-based CBT, are especially effective when medical symptoms are persistent and not fully responsive to physical treatment. Behavioral therapy examples in chronic care often include pacing techniques, goal-setting around activity levels, and stress-reduction routines designed to mitigate flare-ups. These modifications demonstrate how different types of CBT are not only psychologically versatile but also integrative with broader health management plans.
3. What role does technology play in delivering different types of cognitive behavioral therapy today?
The digital revolution has reshaped access to mental healthcare by enabling new delivery models for various types of CBT. Mobile apps, virtual reality tools, and AI-guided platforms now offer interactive modules that simulate therapist-led sessions or provide instant feedback. Some platforms specialize in niche forms of CBT, offering personalized content based on symptom tracking, making these tools excellent vehicles for implementing different types of cognitive behavioral therapy at scale. Additionally, behavioral therapy examples in digital settings include gamified exposure exercises, thought journaling via chatbots, and progress dashboards—all elements that reinforce engagement. The rise of telehealth has also allowed more people to explore different types of CBT, making therapy both more accessible and data-informed.
4. Are there different types of CBT designed for couples or families rather than individuals?
Absolutely. While CBT is traditionally associated with individual therapy, several types of CBT have been developed specifically for relational contexts. Cognitive-behavioral conjoint therapy (CBCT), for instance, integrates interpersonal dynamics with CBT principles to improve communication, reduce conflict, and build shared coping strategies. These types of cognitive therapy often include behavioral therapy examples like joint behavior contracts, structured problem-solving, and shared cognitive restructuring exercises. Different types of CBT within family therapy settings are also used for managing adolescent behavioral issues, parental burnout, and sibling conflict. These modalities reinforce that CBT is not confined to individual introspection—it can also foster emotional intelligence and accountability in interpersonal settings.
5. How do behavioral therapy examples differ across the many types of CBT used in inpatient versus outpatient settings?
Inpatient settings often rely on more intensive, structured behavioral therapy examples due to the acute nature of psychiatric or dual-diagnosis conditions. These might include round-the-clock behavior monitoring, crisis management protocols, and group-based cognitive-behavioral training. In contrast, outpatient therapy provides greater flexibility and autonomy, often utilizing types of cognitive therapy that prioritize long-term skill development and community reintegration. The different types of cognitive behavioral therapy in outpatient care may incorporate real-life exposure exercises, daily homework assignments, and collaborative treatment planning to support gradual but consistent progress. These setting-specific applications underscore the adaptability of the different types of CBT to fit both high-intensity and maintenance-based treatment goals.
6. What innovations are shaping the future of different types of cognitive behavioral therapy?
Innovations in neuroscience, AI, and psychometrics are influencing how clinicians develop and refine different types of CBT. Neurofeedback-integrated CBT is emerging as a promising technique for enhancing emotional regulation and attention through brainwave monitoring paired with cognitive restructuring. Some of the newer types of cognitive therapy are also integrating biofeedback, allowing clients to monitor physiological responses—such as heart rate variability—during exposure tasks. Furthermore, predictive analytics are being used to identify which types of CBT may yield better outcomes based on an individual’s symptom cluster, genetic profile, or psychosocial history. These developments represent a leap toward precision psychology, ensuring that different types of cognitive behavioral therapy are not only evidence-based but also data-personalized.
7. How do different types of CBT address cultural and linguistic diversity in therapy?
Cultural competence in therapy is no longer optional, and different types of CBT have evolved to reflect this imperative. Some adaptations include language-matched therapy materials, inclusion of culturally relevant metaphors, and the restructuring of core CBT assumptions to align with communal rather than individualistic worldviews. For example, behavioral therapy examples in collectivist cultures may emphasize harmony, duty, and respect for elders rather than purely self-driven goals. Additionally, types of cognitive therapy are now being translated into multiple languages while retaining therapeutic intent, ensuring accessibility for non-native speakers. These cultural modifications ensure that different types of CBT remain effective and ethical across global populations.
8. How do the types of CBT used for children differ from those used for adults?
Pediatric CBT is often more creative and action-oriented compared to adult therapy, as it must account for developmental stage and attention span. Different types of CBT used with children typically incorporate games, art, storytelling, and physical movement to teach core skills. Behavioral therapy examples may include sticker charts for behavior reinforcement, puppet modeling for emotional expression, and role-play scenarios to teach conflict resolution. Types of cognitive therapy for younger populations often adapt cognitive distortions into age-appropriate language—for instance, calling negative automatic thoughts “brain bullies” or “worry monsters.” These playful yet evidence-based techniques illustrate how different types of cognitive behavioral therapy can be developmentally tuned without losing therapeutic impact.
9. How are different types of CBT evaluated for effectiveness in clinical practice?
Effectiveness across different types of cognitive behavioral therapy is measured through outcome-based metrics like symptom reduction, functional improvement, and quality of life indices. Randomized controlled trials (RCTs) remain the gold standard for evaluating efficacy, but ongoing feedback through client-reported outcome measures (PROMs) also plays a vital role. Moreover, some types of CBT—such as transdiagnostic or modular CBT—are gaining popularity precisely because they perform well across a spectrum of diagnoses, reducing the need for condition-specific tailoring. Behavioral therapy examples used in outcome tracking may include frequency logs for compulsions, panic diary reductions, or improvements in sleep patterns. These assessments ensure that the different types of CBT maintain scientific rigor while staying responsive to client needs.
10. Can individuals combine different types of CBT simultaneously, or should therapy follow a linear approach?
Modern practice increasingly supports the integration of different types of CBT in a fluid, non-linear fashion, especially for clients with complex or co-occurring conditions. For instance, a person managing PTSD and insomnia might benefit from combining trauma-focused CBT with CBT for sleep hygiene. Therapists often blend types of cognitive therapy, drawing from exposure, behavioral activation, and schema work depending on what a client needs in the moment. Real-world behavioral therapy examples might include journaling for insight alongside graded exposure for phobias, all within the same treatment week. This integrative model shows how different types of cognitive behavioral therapy can be harmonized to provide a comprehensive, client-centered approach without losing coherence.
Conclusion: Why Understanding the Different Types of CBT Matters for Mental Health Outcomes
In an era where mental health challenges are increasingly recognized as multifaceted and individualized, the evolution of CBT into a diverse family of specialized interventions is both timely and essential. By exploring the different types of CBT—from traditional cognitive restructuring to schema-focused and mindfulness-based approaches—we gain a deeper appreciation for how this therapeutic model has matured into a nuanced and flexible system of care. The ability to tailor cognitive behavioral therapy to specific psychological needs is not merely a technical advantage—it is a testament to the field’s ethical commitment to person-centered healing.
Whether one is seeking support for anxiety, depression, trauma, or personality disorders, understanding the types of cognitive therapy available can empower both clients and clinicians to make informed, collaborative treatment decisions. These different types of cognitive behavioral therapy are more than theoretical categories; they are living practices shaped by real-world challenges and the evolving science of human resilience. As we continue to refine our approaches and expand our understanding, CBT stands as a beacon of integrative, compassionate, and effective psychological care—a therapy that honors both the complexity of the human mind and the power of structured, intentional change.
Further Reading:
Cognitive Behavioral Therapy (CBT): What It Is & Techniques


