Care for someone with dementia at home is a profound journey, one that calls for a unique blend of patience, knowledge, empathy, and resilience. When this caregiving takes place within the walls of a family home, the dynamics shift even further. The household transforms into both a sanctuary and a center of care, challenging caregivers to find a balance between familial warmth and medical necessity. Dementia home care is not just about managing symptoms; it’s about preserving dignity, enhancing quality of life, and maintaining a sense of normalcy in an ever-changing reality. For many who say, “I have some family members that have dementia and need support,” the desire to provide in-home memory care is deeply rooted in love. Yet without proper guidance and tools, that commitment can become overwhelming.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding the Basics of Dementia and Its Progression
Before diving into caregiving strategies, it’s essential to grasp what dementia actually entails. Dementia is not a single disease but a general term describing a range of symptoms associated with a decline in memory, reasoning, and other cognitive abilities. Alzheimer’s disease is the most common cause, though vascular dementia, Lewy body dementia, and frontotemporal dementia also fall under this umbrella. Each type progresses differently, but all eventually interfere with daily living.
Understanding how dementia unfolds over time is vital for dementia home care. Early stages might involve mild forgetfulness or confusion, while later stages often require full assistance with activities of daily living. For those caring for a parent with dementia at home, recognizing these stages helps set realistic expectations and enables proactive planning. By knowing the nature and trajectory of dementia, caregivers can tailor their approach to meet evolving needs.
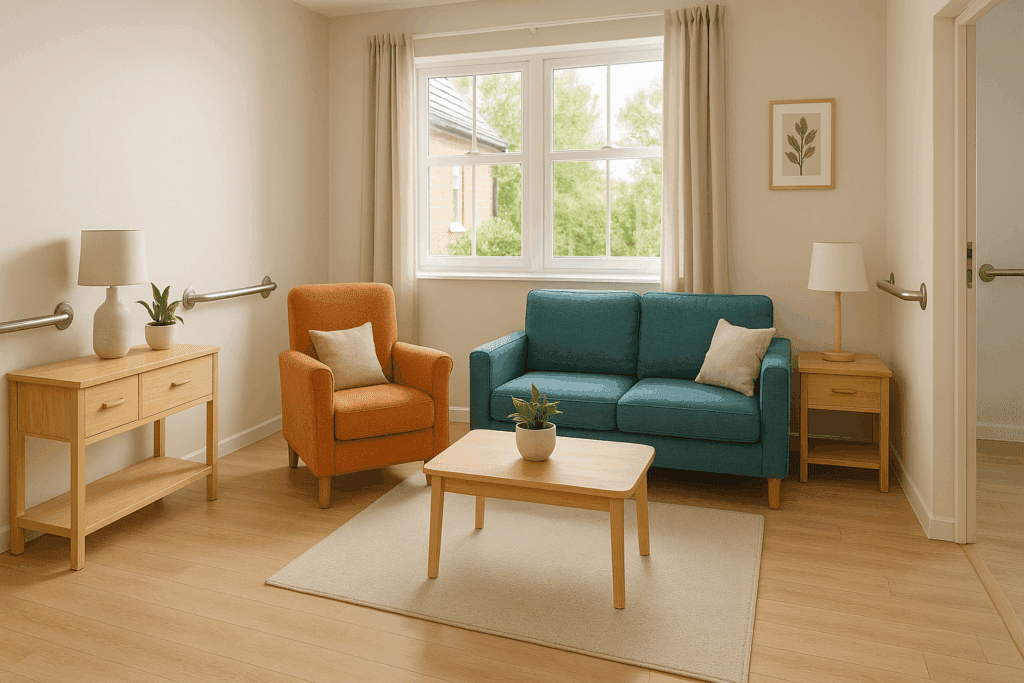
Building a Dementia-Friendly Home Environment
Transforming a family home into a safe and supportive environment is one of the foundational tasks of dementia caregiving. In-home memory care requires careful attention to environmental details. Simple changes, such as removing loose rugs, installing grab bars in bathrooms, labeling cabinets, or using contrasting colors to differentiate objects, can significantly reduce risks of injury and confusion. For individuals offering home care for dementia sufferers, these adjustments aren’t merely cosmetic—they’re safety measures that protect both patient and caregiver.
Lighting plays an often-overlooked role in dementia home care. Poor lighting can contribute to disorientation, especially in the evening hours when sundowning—a symptom in which confusion and agitation worsen—may occur. Maintaining natural light during the day and using warm, low-glare lighting at night helps support a consistent sleep-wake cycle. When caring for someone with dementia, the home must be a place that reinforces orientation and calm rather than chaos.

Establishing Daily Routines That Promote Stability
Dementia thrives on routine. For caregivers wondering how to deal with someone with dementia who seems constantly unsettled, the answer may lie in predictable daily rhythms. Routines offer structure and familiarity, reducing anxiety and making the world feel more navigable to someone whose memory is faltering. Mealtimes, bathing, medication, and bedtime should follow consistent patterns each day. While flexibility remains important, major disruptions should be minimized when possible.
Those taking on the role of caring for a parent with dementia often find that even small routines—such as a morning walk or an afternoon cup of tea—can become treasured rituals. These moments help ground the individual in a familiar flow and offer caregivers time to connect meaningfully. In fact, implementing routines is one of the most powerful dementia caregiver tips for creating emotional and cognitive stability at home.
The Importance of Effective Communication
One of the greatest challenges of how to deal with dementia is learning to communicate in ways that respect the individual’s changing cognitive abilities. Verbal skills may decline, but emotional awareness often remains sharp. How you speak matters as much as what you say. Use short, clear sentences, and always speak calmly and at eye level. Avoid quizzing the person or correcting them, as doing so may cause embarrassment or frustration.
When family members wonder how to help someone with dementia maintain dignity, communication becomes key. Redirecting rather than correcting is often more effective. For example, if your loved one insists it’s 1962, rather than confronting the falsehood, consider entering their world momentarily. This is not deception but compassion—a method of honoring their perception of reality. As part of patient teaching for dementia, caregivers should understand that communication is more about connection than correction.
Cultivating Patience with Dementia Patients
Patience is not just a virtue in dementia care—it’s a lifeline. Many caregivers struggle with how to deal with dementia patients when behaviors become repetitive, irrational, or aggressive. But it’s essential to recognize that such behaviors are not intentional acts of defiance; they are symptoms of a damaged brain. Having patience with dementia patients involves taking deep breaths, stepping away when needed, and reminding oneself that the individual is doing the best they can within the limitations of their condition.
Learning how to cope with dementia patients also requires the caregiver to develop emotional self-regulation techniques. Mindfulness, therapy, and support groups can all be invaluable tools for maintaining inner calm. A caregiver who feels grounded is better equipped to respond with empathy rather than irritation, which ultimately benefits the person with dementia. Sustaining patience is a long-term practice—one that must be renewed daily.
Nutrition and Mealtime Considerations
Feeding a person with dementia can become increasingly difficult over time. In later stages, your loved one may forget to eat, lose the ability to use utensils, or experience changes in taste and appetite. For those providing dementia home care services, adapting to these shifts without frustration is crucial. Serving finger foods, offering frequent small meals, and ensuring hydration are practical ways to support nutritional health.
Cultural food preferences and sensory experiences—such as the smell of baking bread or the sound of a sizzling skillet—can also help stimulate appetite and foster connection. Mealtimes are opportunities for comfort and ritual. Those asking how to care for people with dementia often overlook this emotional dimension of food. Eating is not just a biological necessity; it’s a deeply human experience that connects us to memory, culture, and family.
Understanding Behavioral Changes and How to Respond
As dementia progresses, behavioral changes often become more pronounced and puzzling. Loved ones may experience mood swings, paranoia, sleep disturbances, and agitation. For caregivers trying to understand how to deal with a family member with dementia, it’s helpful to view behavior as a form of communication. Rather than reacting to the behavior itself, consider what need might be going unmet. Are they hungry, tired, in pain, or overwhelmed by stimuli?
Behavioral issues may also stem from environmental triggers. Noisy rooms, unfamiliar faces, or abrupt changes in schedule can cause distress. When looking for dementia caregiver tips, understanding how to identify and remove such triggers is invaluable. It’s also essential to resist taking behaviors personally. The person you love is still there, but their ability to interact in familiar ways has shifted. Compassionate interpretation of behaviors forms the cornerstone of effective dementia care at home.
Self-Care for the Caregiver: Avoiding Burnout
Providing home health care for dementia patients can be deeply rewarding—but also physically and emotionally draining. Caregiver burnout is a serious risk and can undermine both the caregiver’s health and the quality of care provided. It’s crucial to take breaks, seek respite care when needed, and maintain connections with friends and supportive communities. Saying “I have some family members that have dementia and I need help caring for them” should never be a source of shame. In fact, reaching out is a sign of strength and foresight.
Caregivers must learn to prioritize their own well-being. Regular exercise, sleep, proper nutrition, and emotional outlets—such as journaling or counseling—are not luxuries but necessities. Remember that taking care of yourself is not a distraction from your caregiving role; it is an essential component of it. A well-supported caregiver is a more capable one, and those receiving care benefit as a result.
Navigating Legal, Financial, and Medical Responsibilities
The responsibilities of dementia home care extend far beyond daily routines and emotional support. Legal, financial, and medical planning must also be addressed. Powers of attorney, advance directives, and guardianship may need to be established early in the disease process. Delaying these conversations can create confusion or conflict later. For those asking how to deal with a person with dementia in a long-term context, proactive legal planning is essential.
Medical care coordination is another critical aspect. Regular doctor visits, medication management, and collaboration with specialists require ongoing attention. Keeping detailed notes and developing a relationship with a primary care provider or neurologist can streamline care. Some families may also need to explore home health care for dementia services, including visiting nurses or occupational therapists who specialize in memory care. These professionals can help manage complex needs while allowing the individual to remain at home.
When and How to Seek Outside Help
While many families begin by taking care of a parent with dementia independently, there often comes a time when additional help is needed. This decision is highly personal and may involve emotions of guilt, grief, and relief all at once. If safety becomes an issue or if caregiving demands exceed what one person can manage, it may be time to consider home care for dementia sufferers through licensed agencies. In-home aides, respite care providers, and adult day programs can supplement the care you provide and prevent burnout.
Selecting the right support team requires research and trust. Look for dementia home care services that offer staff trained specifically in memory care. Ask about continuity of care, caregiver-to-patient ratios, and emergency protocols. Engaging professional support does not mean you’re giving up—it means you’re ensuring the highest standard of care, both for your loved one and yourself. Asking, “How can I help someone with dementia when I’m overwhelmed?” is a powerful moment of clarity, not a failure.
Connecting with the Person Behind the Diagnosis
Even as cognitive function declines, emotional memory often remains intact. A familiar song, a cherished photograph, or the scent of a favorite flower can stir recognition and joy. For those seeking insight into how to help a person with dementia retain a sense of identity, these emotional touchpoints are invaluable. They help us connect with the person beneath the disease, reminding both caregiver and patient of their enduring humanity.
Finding moments of joy amid hardship is possible. Dance in the living room. Sing old lullabies. Look through photo albums. Celebrate birthdays. These moments need not be elaborate to be meaningful. When asking how to help dementia patients feel loved and seen, the answer is often found in the smallest acts of shared presence.
Recognizing the Limitations of Home-Based Dementia Care
While many families want to continue caring for a parent with dementia at home for as long as possible, there may come a point when home care alone is no longer sufficient. Wandering, aggressive behavior, or complex medical needs can make the home environment unsafe despite your best efforts. Knowing when to transition to assisted living or memory care facilities requires honest reflection and input from healthcare professionals.
Acknowledging this stage is not a betrayal—it’s a continuation of loving, responsible care. The question is no longer just “how do you care for a person with dementia,” but “how do you ensure they continue to receive the care they need?” Sometimes the best way to care for someone is to know when to seek the resources and professionals who can provide the next level of support.
Final Reflections: Providing Meaningful Dementia Home Care with Empathy and Expertise
Caring for someone with dementia at home is both a privilege and a profound responsibility. It challenges us to dig deeper into our reserves of compassion, flexibility, and courage. Whether you’re just beginning this journey or have been navigating it for years, it’s important to remember that you are not alone. There is a growing body of knowledge, services, and community networks available to support you in this role.
Every time you ask yourself how to care for someone with dementia or seek out dementia caregiver tips, you reaffirm your dedication to dignified, person-centered care. By transforming your home into a safe haven, maintaining patience with dementia patients, and seeking help when needed, you are upholding the values of empathy and excellence. Providing in-home memory care is not only possible—it can be a source of deep connection and love.
The more we talk openly about dementia home care, the better prepared we become as a society to meet this growing challenge with compassion and competence. Whether you are caring for someone with dementia or offering support to others in that role, know that your efforts matter. With the right information, tools, and support, home truly can be a place where memory and meaning endure.
Further Reading:
Tips for Caregivers and Families of People With Dementia
10 Tips for Dementia Caregivers: Expert Advice From Clinicians