In recent years, there has been a surge of scientific interest in the connection between digestive health and mental well-being. The concept of a “leaky gut,” once confined to the periphery of medical discussions, has now entered the mainstream of health research, particularly in the context of anxiety and mood disorders. But can leaky gut cause anxiety, or is this merely a correlation without concrete causation? As the gut-brain axis garners increasing attention in neuroscience and gastroenterology, a clearer picture is emerging—one that suggests our emotional state is deeply intertwined with the health of our intestinal barrier.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
Understanding Leaky Gut: A Foundation for the Mind-Body Connection
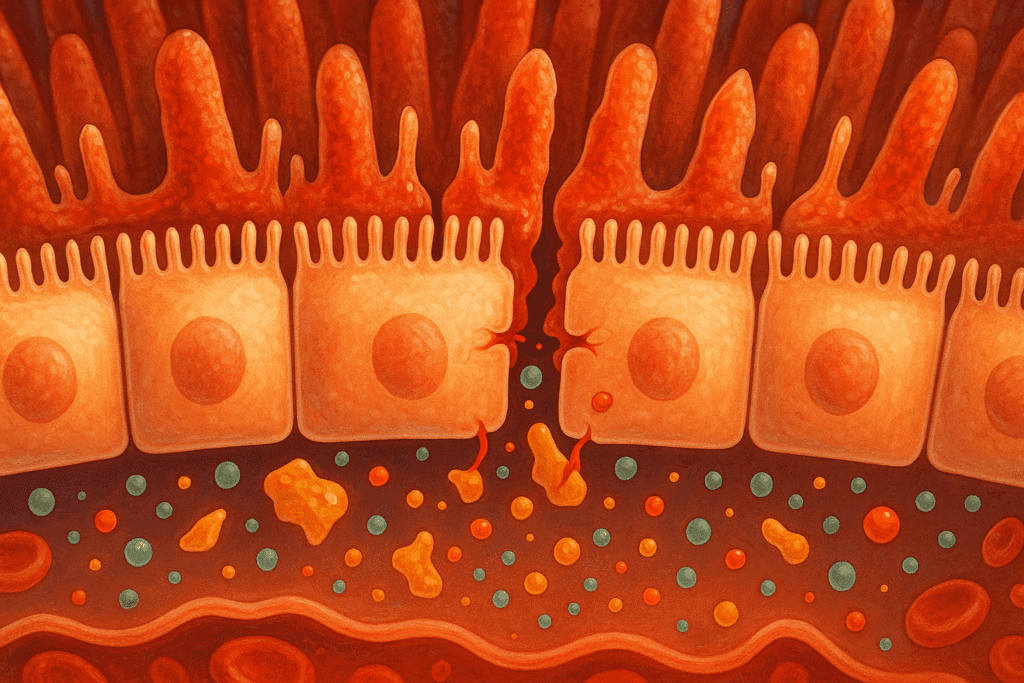
Leaky gut syndrome, also referred to in clinical literature as increased intestinal permeability, is characterized by the breakdown of the tight junctions in the intestinal lining. These junctions typically act as gatekeepers, regulating the passage of nutrients while preventing toxins, pathogens, and partially digested food particles from entering the bloodstream. When these junctions weaken or become compromised, it can lead to systemic inflammation, immune activation, and a cascade of physiological disruptions. Although leaky gut is not officially recognized as a standalone medical diagnosis by all regulatory bodies, mounting research supports its relevance in a variety of chronic conditions, including irritable bowel syndrome, autoimmune disorders, and neurological symptoms.
The idea that digestive health influences mental health is not new, but modern science has refined and validated this concept through advanced imaging, microbiome analysis, and molecular biology. The notion that leaky gut anxiety is more than a speculative connection is supported by growing evidence linking intestinal permeability to systemic inflammation and neuroinflammatory responses. This link is particularly relevant because chronic, low-grade inflammation has been strongly associated with anxiety, depression, and other mood disorders.
How the Gut-Brain Axis Orchestrates Emotional Stability
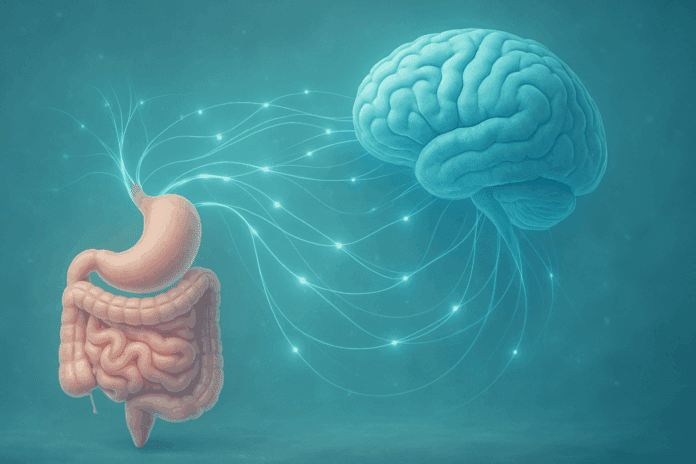
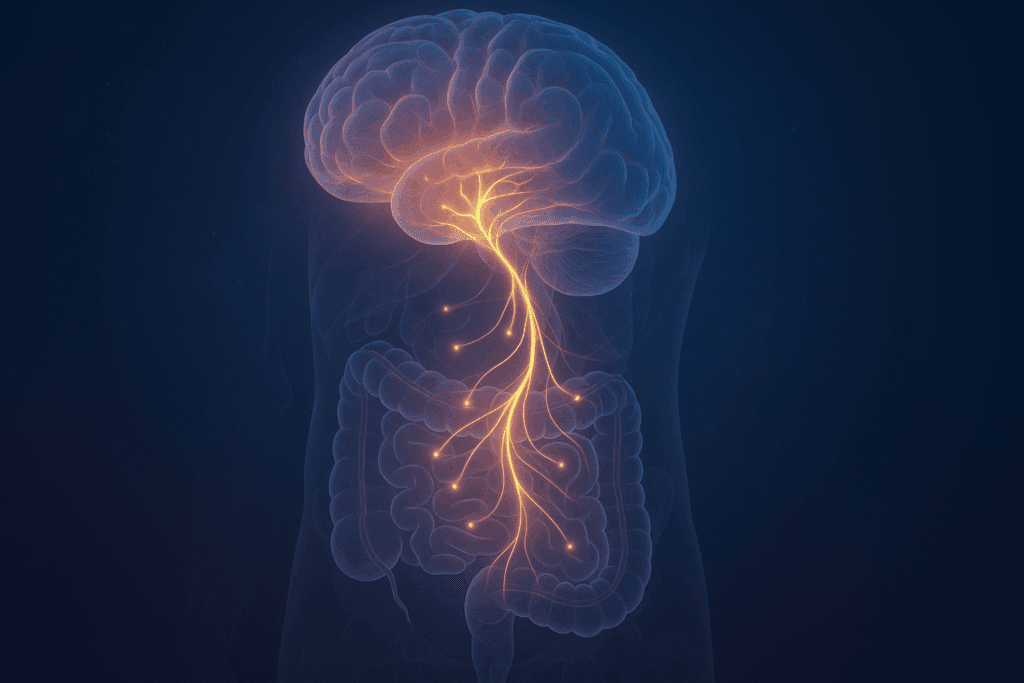
At the heart of the leaky gut-anxiety connection lies the gut-brain axis—a bidirectional communication network that links the enteric nervous system of the gastrointestinal tract with the central nervous system. This axis involves a dynamic interplay of neural, hormonal, and immunological pathways. It is through this complex system that changes in gut health can influence brain function and vice versa.
The vagus nerve plays a central role in this dialogue. Acting as a superhighway between the gut and the brain, it conveys signals related to inflammation, microbial balance, and nutrient status. When the intestinal lining is compromised, as in the case of leaky gut, immune cells begin releasing pro-inflammatory cytokines. These cytokines can travel through the bloodstream and cross the blood-brain barrier, impacting neurotransmitter function and activating brain regions involved in fear and stress responses, such as the amygdala.
Moreover, the gut microbiome—a vast and diverse ecosystem of bacteria, viruses, and fungi—also plays a critical role. Alterations in microbiome composition due to increased gut permeability can result in reduced production of short-chain fatty acids (SCFAs) like butyrate, which have anti-inflammatory properties and help maintain the integrity of the blood-brain barrier. Disruptions in these microbial ecosystems may contribute to changes in behavior and emotional regulation, further reinforcing the idea that leaky gut anxiety is a biologically plausible phenomenon.
Scientific Evidence Linking Leaky Gut and Anxiety Disorders
Several studies have investigated the potential link between leaky gut and anxiety, providing a growing body of empirical support. For example, research published in Psychoneuroendocrinology has demonstrated that individuals with major depressive disorder often exhibit elevated markers of gut permeability, such as zonulin and lipopolysaccharides (LPS), both of which indicate increased intestinal leakiness. These biomarkers have also been found in patients with generalized anxiety disorder, suggesting a shared inflammatory pathway that connects gut health and psychological symptoms.
Animal studies further strengthen this connection. In one landmark study, mice subjected to stress-induced leaky gut developed behaviors consistent with anxiety, including avoidance, restlessness, and heightened stress reactivity. When treated with probiotics or anti-inflammatory compounds that restored intestinal integrity, these mice exhibited a marked reduction in anxious behaviors. While human studies are more complex due to lifestyle and genetic variability, the consistency of findings across animal and clinical models lends credibility to the hypothesis that increased gut permeability can trigger anxiety-related responses.
Another compelling study published in Neurogastroenterology & Motility showed that individuals with irritable bowel syndrome—a condition commonly associated with leaky gut—had significantly higher anxiety scores compared to the general population. The same study noted that therapeutic strategies aimed at improving gut barrier function also yielded improvements in anxiety symptoms, further supporting the concept that addressing leaky gut anxiety at the source can have broad psychological benefits.
The Role of Inflammation and Neurotransmitter Dysregulation
One of the most critical mechanisms linking gut permeability and anxiety is the inflammatory cascade that follows the translocation of microbial components into the bloodstream. These components, including endotoxins like LPS, activate toll-like receptors on immune cells, triggering the release of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These cytokines not only influence systemic inflammation but also modulate brain chemistry by affecting the synthesis, release, and reuptake of key neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA).
Serotonin is particularly noteworthy in this context because a significant portion—approximately 90%—of the body’s serotonin is produced in the gut. When intestinal inflammation disrupts this production, it can lead to imbalances that manifest as anxiety or mood instability. Similarly, disruptions in GABA signaling, which normally serves to inhibit excessive neural excitation, can predispose individuals to heightened anxiety and stress sensitivity. Thus, the physiological events triggered by a leaky gut do not stay confined to the digestive tract; they ripple outward, influencing emotional states and cognitive function in profound ways.

Microbiota, Diet, and Psychological Resilience
The composition of the gut microbiome is not static. It is highly sensitive to dietary inputs, stress, medications, and environmental toxins. Emerging evidence suggests that dietary interventions that promote microbial diversity and intestinal barrier health may offer therapeutic potential for individuals experiencing leaky gut anxiety. Diets rich in prebiotic fibers, fermented foods, and polyphenol-rich plant compounds have been shown to enhance the production of SCFAs and bolster mucosal defenses.
Conversely, diets high in processed foods, sugar, and artificial additives may exacerbate intestinal permeability and microbial dysbiosis. For example, emulsifiers commonly found in packaged foods have been shown to disrupt the mucous layer that protects the gut lining. Additionally, a deficiency in critical nutrients such as zinc, vitamin D, and omega-3 fatty acids may impair the body’s ability to maintain tight junction integrity, thereby increasing susceptibility to leaky gut and its associated emotional consequences.
Interventional studies exploring the effects of probiotic supplementation have yielded promising results. Specific strains, including Lactobacillus rhamnosus and Bifidobacterium longum, have been found to reduce anxiety-like behaviors in both animal models and human participants. These findings align with the broader notion that cultivating a healthy gut microbiome may serve as a foundation for psychological resilience.
Psychosocial Stress, Cortisol, and Gut Barrier Integrity
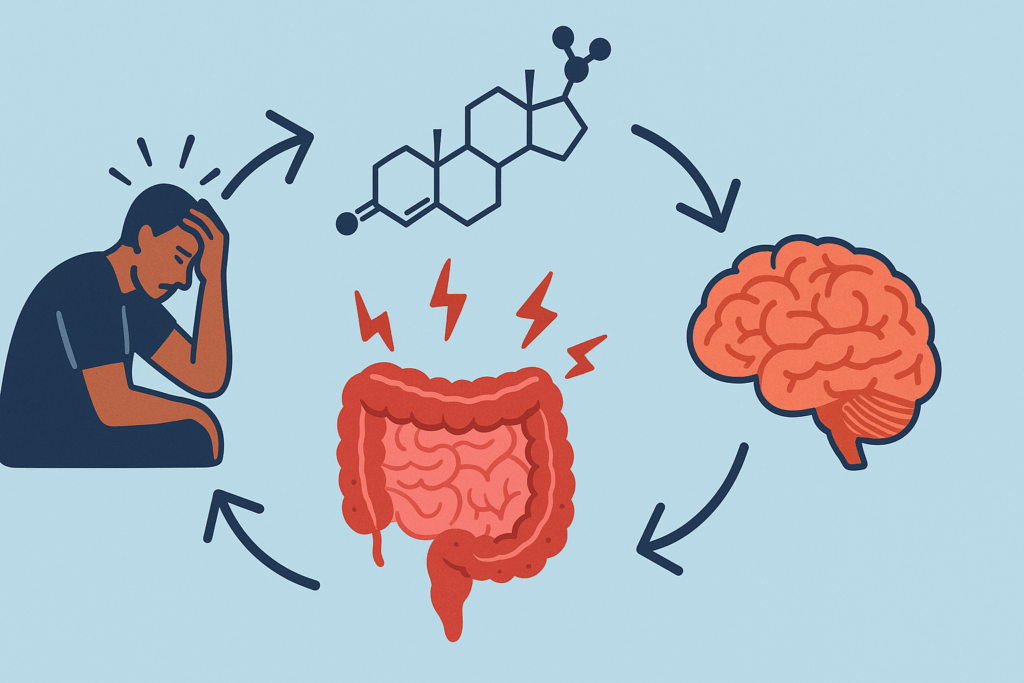
Chronic stress is a well-documented contributor to both mental health challenges and gastrointestinal dysfunction. The hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s response to stress, can disrupt intestinal homeostasis when persistently activated. Elevated cortisol levels have been shown to alter gut motility, reduce mucus secretion, and increase permeability of the epithelial lining.
This physiological state creates a feedback loop in which stress contributes to a leaky gut, which in turn heightens susceptibility to anxiety. Understanding this relationship underscores the importance of stress management strategies not only for mental well-being but also for maintaining digestive health. Techniques such as mindfulness meditation, yoga, and cognitive behavioral therapy have demonstrated efficacy in reducing both psychological stress and gastrointestinal symptoms, providing a holistic approach to managing leaky gut anxiety.
Clinical Approaches and Emerging Therapies
Given the complexity of the gut-brain connection, a multifaceted treatment approach is often required. Clinicians working with patients experiencing both gastrointestinal and psychological symptoms increasingly advocate for integrated care that addresses both domains. This may involve a combination of dietary modifications, targeted supplementation, stress reduction techniques, and when necessary, pharmacological support.
Emerging therapies include the use of precision probiotics tailored to an individual’s unique microbiome profile, as well as microbiota transplants in severe cases of dysbiosis. While these interventions are still under investigation, early trials suggest that restoring microbial balance can result in meaningful improvements in mood and cognitive function. Functional medicine practitioners may also recommend advanced diagnostic tests to assess markers of gut permeability, microbial composition, and inflammatory status to guide personalized treatment plans.
It is important to note that while addressing gut health may alleviate anxiety for some individuals, it should not replace evidence-based psychiatric care when needed. Mental health is multifactorial, and although leaky gut can be a contributing factor, it is rarely the sole cause. A comprehensive approach that incorporates psychological, nutritional, and physiological dimensions is most likely to yield lasting improvements.
Reframing the Question: Can Leaky Gut Cause Anxiety?
Rather than viewing the relationship between gut permeability and anxiety as a binary cause-and-effect scenario, it is more accurate to understand it as a dynamic interplay. Asking “can leaky gut cause anxiety” invites a nuanced discussion that takes into account the bidirectional and often cyclical nature of the gut-brain connection. While leaky gut may not cause anxiety in all cases, it clearly contributes to a physiological environment that can predispose individuals to emotional distress.
This distinction is essential for both clinical accuracy and for setting realistic expectations about treatment outcomes. A person experiencing anxiety may find that improving gut health leads to measurable relief, but this does not imply that gut dysfunction is the root of all mental health concerns. In some cases, the anxiety may have preceded gut issues, and in others, the reverse may be true. What is increasingly clear, however, is that the health of the gut and the state of the mind are deeply connected and mutually influential.
Why This Matters: Implications for Public Health and Personal Well-Being
The growing body of evidence linking intestinal permeability to mental health has significant implications not only for individual well-being but also for broader public health strategies. Recognizing the gut-brain axis as a legitimate target for intervention could shift how we approach both preventive care and chronic disease management. Schools, workplaces, and healthcare systems may benefit from educational initiatives that emphasize the importance of gut-friendly dietary habits and stress reduction techniques.
On a personal level, understanding the potential role of leaky gut anxiety empowers individuals to take proactive steps toward improving their emotional resilience. Whether through mindful eating, reducing exposure to gut-disrupting chemicals, or incorporating relaxation practices into daily life, small changes can yield meaningful improvements in both gut integrity and mental equilibrium. The integration of these practices into everyday routines reflects a growing awareness that mental health cannot be fully disentangled from physical health.
Looking Ahead: Where Research and Medicine Are Headed
As research continues to evolve, future studies will likely focus on refining diagnostic criteria for leaky gut, identifying reliable biomarkers, and exploring personalized treatment protocols that address the gut-brain axis in a targeted manner. Advances in microbiome sequencing, metabolomics, and neuroimaging are already providing more sophisticated tools for unraveling the complexities of this relationship.
There is also growing interest in understanding how early-life events—such as birth mode, antibiotic exposure, and childhood nutrition—shape the gut-brain axis and influence long-term mental health outcomes. By identifying key windows of vulnerability and opportunity, researchers may develop preventive interventions that support gut and brain development from infancy through adulthood. This integrative perspective holds promise for reshaping how we understand, treat, and ultimately prevent conditions related to both gut permeability and psychological distress.
Frequently Asked Questions: Leaky Gut and Anxiety
1. How long does it typically take for anxiety symptoms to improve after addressing leaky gut?
While every individual is different, many people report experiencing noticeable improvements in anxiety symptoms within four to eight weeks of beginning a gut-healing protocol. However, this timeline depends on factors such as the severity of intestinal permeability, existing nutrient deficiencies, stress levels, and how consistently dietary and lifestyle changes are implemented. It’s also important to remember that while some people with leaky gut anxiety experience rapid relief, others may require more comprehensive treatment, including psychological support. Incorporating practices like meditation, sleep hygiene, and microbiome diversity can significantly enhance results. The question of whether leaky gut causes anxiety is often better framed in terms of complex, multifactorial relationships that unfold gradually, not overnight.
2. Can leaky gut anxiety persist even after gut permeability has improved?
Yes, it’s possible for anxiety symptoms to continue even after intestinal permeability has been reduced. This is because the relationship between leaky gut and anxiety involves feedback loops in the nervous and immune systems that may take time to reset. Chronic anxiety can become conditioned in the brain, independent of the original physiological triggers. Therefore, even after the gut has begun to heal, ongoing psychological support may be necessary to address lingering emotional patterns. Recognizing this can help set realistic expectations for those exploring whether or not leaky gut causes anxiety in their specific situation.
3. Are certain personality traits or psychological profiles more susceptible to leaky gut anxiety?
Emerging research suggests that individuals with high trait anxiety, perfectionism, or a heightened stress response may be more vulnerable to developing gut-related inflammation. These psychological traits often correlate with elevated cortisol levels, which can impair gut barrier function and alter microbiome composition. When this physiological vulnerability is coupled with stress-inducing thought patterns, the risk of developing leaky gut anxiety increases. Moreover, people with a history of trauma or chronic emotional suppression may have preexisting dysregulation in the gut-brain axis. While personality alone doesn’t determine whether leaky gut causes anxiety, it can certainly amplify the underlying risk factors.
4. Can addressing leaky gut reduce reliance on psychiatric medications for anxiety?
In some cases, improving gut health has allowed patients to reduce their dependence on anti-anxiety medications under medical supervision. However, this is never a one-size-fits-all approach. Individuals exploring whether leaky gut causes anxiety often need to work collaboratively with both gastroenterologists and mental health professionals. When gut restoration is paired with cognitive therapy or mindfulness-based interventions, it can create a powerful synergy that supports tapering strategies. Still, any changes to psychiatric medication should be done gradually and always under the guidance of a licensed provider.
5. How do environmental toxins contribute to leaky gut anxiety?
Environmental toxins such as pesticides, heavy metals, and endocrine disruptors can compromise the intestinal barrier and alter the gut microbiome. These substances may not only increase permeability but also trigger systemic inflammation that affects the central nervous system. This kind of toxic burden can intensify the connection between leaky gut and anxiety, especially in individuals with genetic vulnerabilities in detoxification pathways. Water quality, household chemicals, and even certain beauty products can serve as hidden sources of gut irritants. Recognizing and minimizing these exposures is an often overlooked step in managing leaky gut anxiety.
6. Are there specific diets that have been shown to improve both leaky gut and anxiety?
Yes, diets such as the Mediterranean diet, low-FODMAP, and the specific carbohydrate diet (SCD) have shown promise in improving gut integrity and reducing inflammation. These diets emphasize whole foods, fiber, fermented products, and healthy fats, which support microbiota diversity and mucosal healing. When followed consistently, these dietary approaches can reduce the neuroinflammatory load associated with leaky gut anxiety. However, personal tolerance should guide dietary choices, as even healthy foods can cause symptoms if improperly matched to the individual. Working with a registered dietitian or functional medicine practitioner can help customize a plan that supports both digestive and emotional health.
7. Can children or adolescents experience leaky gut anxiety?
Absolutely. In fact, children may be particularly vulnerable due to the developmental sensitivity of both their gut lining and nervous system. Factors like early antibiotic exposure, processed foods, and chronic stress at school or home can compromise gut health during critical periods. In some children, symptoms of leaky gut anxiety may manifest as behavioral challenges, attention deficits, or sleep disturbances rather than classic worry or panic. Pediatricians and child psychologists increasingly recognize the need to explore gut-brain interactions in cases of unexplained emotional or cognitive symptoms. Proactive nutritional and emotional support can have profound long-term benefits for young individuals.
8. How does sleep quality interact with the relationship between leaky gut and anxiety?
Sleep is a critical mediator in the bidirectional relationship between gut health and mental well-being. Poor sleep increases gut permeability and inflammation, while a disrupted microbiome can interfere with melatonin and serotonin production—both essential for restful sleep. This creates a vicious cycle in which leaky gut anxiety is amplified by poor sleep hygiene and circadian rhythm disturbances. Interventions that support sleep quality, such as reducing screen time, optimizing sleep environment, and practicing relaxation techniques before bed, can break this cycle. Incorporating targeted nutrients like magnesium glycinate and glycine may also support both gut and sleep health.
9. What role does movement or exercise play in managing leaky gut anxiety?
Moderate physical activity has been shown to enhance microbial diversity and reduce systemic inflammation, making it a powerful ally in treating leaky gut anxiety. Exercise also stimulates the vagus nerve, which enhances communication between the gut and brain and improves resilience to stress. However, intense or prolonged physical exertion may temporarily increase intestinal permeability in some individuals, especially endurance athletes. The key is finding a sustainable movement practice—such as walking, yoga, or swimming—that promotes gut integrity while supporting emotional regulation. Incorporating mindful movement into daily life can serve as a bridge between physical and psychological healing.
10. Are there any emerging therapies for addressing the root causes of leaky gut anxiety?
Several innovative approaches are being explored to address the deeper mechanisms of leaky gut anxiety. Fecal microbiota transplantation (FMT), for instance, has shown early promise in restoring microbial diversity in treatment-resistant cases. Peptide therapies, such as BPC-157, are also being investigated for their ability to regenerate the gut lining and reduce inflammation. Personalized probiotic formulations based on stool testing are becoming increasingly accessible, offering targeted support based on individual microbiome profiles. These cutting-edge treatments highlight a future where understanding whether leaky gut causes anxiety can lead to truly personalized, integrative care. While many of these therapies remain experimental, they underscore the rapid evolution of gut-brain science.
The Takeaway: Connecting the Dots Between Gut Health and Anxiety
In answering the question “can leaky gut cause anxiety,” the most responsible and evidence-based response is this: leaky gut may not directly cause anxiety in all individuals, but it can significantly contribute to the biological environment that makes anxiety more likely to occur and persist. This understanding reframes the gut-brain connection as a vital, actionable area for intervention.
By exploring the scientific underpinnings of this relationship—ranging from microbiota and inflammation to diet and stress—we not only enhance our grasp of human physiology but also uncover new paths to healing. The implications for mental health care are profound. Integrating digestive health into mental wellness strategies offers a more holistic, nuanced, and ultimately more compassionate model of care. In doing so, we acknowledge the intricate, inseparable connection between body and mind—one that deserves our continued curiosity, respect, and thoughtful attention.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out
Further Reading:
The Connection Between Leaky Gut and Anxiety
Exploring the Link Between the Gut Microbiome and Anxiety
The role of microbiota-gut-brain axis in neuropsychiatric and neurological disorders