Dementia is often described as a cognitive condition that robs individuals of their memory, independence, and ability to engage with the world around them. But beyond the personal and social challenges it poses, a deeper and more unsettling question frequently arises: can dementia lead to death? For those caring for loved ones with advanced cognitive decline, understanding the relationship between dementia and mortality is critical. Medical experts have increasingly emphasized that dementia is not merely a collection of memory impairments but a progressive, degenerative, and ultimately terminal condition. In recent years, public health data, clinical studies, and caregiving experiences have converged to affirm the reality that dementia can and does cause death. This article explores what it means for dementia to be a cause of death, the pathways through which it affects life expectancy, and how medical professionals evaluate its fatal potential.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding the Nature of Dementia as a Terminal Illness
The notion that dementia is a fatal disease can be difficult to reconcile, particularly because its onset is so often insidious. People may live for years with mild cognitive impairment, gradually losing the ability to manage finances, navigate social interactions, or remember recent events. Over time, however, dementia progresses beyond memory loss to affect critical neurological and physiological functions. In advanced stages, individuals may lose the ability to speak, swallow, or move independently, making them more vulnerable to complications like infections, malnutrition, and immobility.
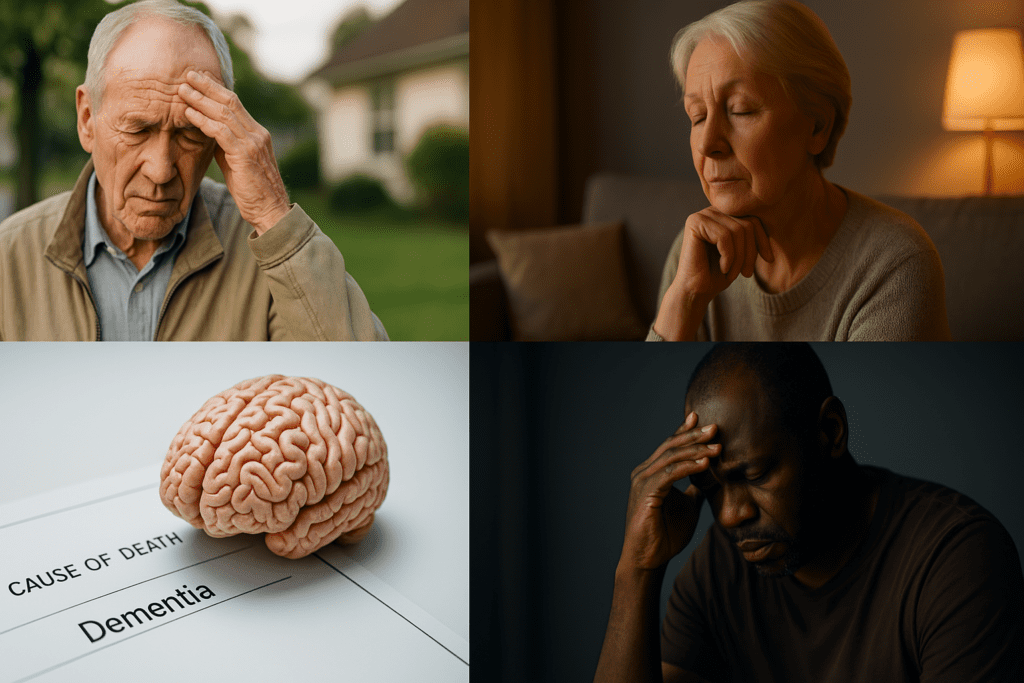
One of the most common misconceptions is that people die with dementia, not from it. While other conditions such as cardiovascular disease or pneumonia may be recorded as the immediate cause of death, dementia often underlies or accelerates these secondary events. Medical professionals are increasingly recognizing this reality, and many death certificates now list dementia as the primary cause. This shift in understanding has brought new clarity to the question: can you die from dementia? The answer, based on clinical experience and mounting evidence, is yes.
How Dementia Causes Death: Direct and Indirect Pathways
To fully grasp how dementia causes death, it’s essential to distinguish between direct and indirect pathways. Directly, the neurodegenerative process affects areas of the brain that control autonomic functions like breathing, swallowing, and heart rate. As the brain deteriorates, these vital systems can fail. In such cases, dementia cause of death is not only accurate but inevitable.
Indirectly, dementia increases susceptibility to life-threatening conditions. Aspiration pneumonia, for example, is a frequent cause of death in late-stage dementia patients who can no longer swallow properly. Similarly, individuals who are bedridden for extended periods due to cognitive decline are at high risk for pressure ulcers, infections, and deep vein thrombosis. These secondary complications are not merely unfortunate side effects; they are often the final events in a long decline triggered by dementia. Thus, when asking, does dementia lead to death, the medical answer is increasingly affirmative.
The Role of Comorbidities and Clinical Decision-Making
Dementia rarely exists in isolation. Most patients are elderly and frequently have coexisting conditions such as hypertension, diabetes, or chronic obstructive pulmonary disease. These comorbidities can complicate both diagnosis and care. When an individual with dementia develops a treatable infection or suffers a fall, healthcare professionals must weigh the potential benefits of aggressive treatment against the overall prognosis. In many cases, the presence of advanced dementia leads to a decision to prioritize comfort over curative measures.
Understanding whether will you die from dementia is not merely a theoretical inquiry but a question with immediate implications for medical management. Palliative care and hospice services often play a critical role in the final stages of dementia, focusing on symptom relief, emotional support, and dignified end-of-life experiences. Increasingly, clinicians and families alike are accepting that dementia is a deadly disease, not because it kills swiftly but because it inevitably leads to the breakdown of systems essential to survival.
Global Mortality Data: Dementia as a Leading Cause of Death
In recent decades, dementia has emerged as one of the leading causes of death globally. According to the World Health Organization, Alzheimer’s disease and other dementias are now among the top ten causes of death worldwide. In many high-income countries, dementia has surpassed heart disease and cancer as the primary cause of death in women. These statistics answer the question, can someone die from dementia, with unambiguous clarity.
The rise in dementia-related deaths is partially due to demographic shifts. As populations age and more people live into their 80s and 90s, the incidence of dementia naturally increases. However, improved awareness and diagnostic accuracy also contribute to higher reporting of dementia death on medical records. More healthcare systems are acknowledging the fatal nature of this condition, ensuring that dementia is recognized not just as a debilitating illness but also as one that shortens life.
Life Expectancy and Disease Progression in Dementia
The trajectory of dementia varies significantly depending on the subtype—whether it’s Alzheimer’s disease, vascular dementia, Lewy body dementia, or frontotemporal dementia. Each presents unique symptoms and progression patterns, yet all share one defining feature: their progression is irreversible and ultimately life-limiting. For many patients, the average life expectancy following a dementia diagnosis ranges from 4 to 8 years, though some may live as long as 20 years with proper care.
This wide range is influenced by factors such as age at diagnosis, general health, gender, and the presence of comorbidities. For instance, younger individuals diagnosed with early-onset Alzheimer’s may live longer but often face a more aggressive disease course. Conversely, older adults with multiple health issues may experience a faster decline. Regardless of these variables, the central question remains: does dementia cause death? The data and clinical experience suggest that in the absence of another primary cause, dementia alone can lead to a terminal decline.
Clinical Indicators of Terminal Dementia
Recognizing the terminal phase of dementia is essential for appropriate care planning. In advanced stages, patients typically exhibit profound cognitive impairment, inability to recognize family members, total dependence for daily activities, and frequent infections. One of the strongest predictors of near-term mortality is difficulty swallowing, which significantly increases the risk of aspiration pneumonia and nutritional deficiencies. In this context, the inquiry—can dementia cause death—becomes not only academic but deeply personal for families observing this progression.
Healthcare providers use tools like the Functional Assessment Staging Tool (FAST) to assess the severity of cognitive decline and determine when a patient enters the terminal phase. This information informs decisions about transitioning to hospice care, which can provide comfort-focused support and guidance for families. The acknowledgment that dementia is a fatal disease reframes how both medical teams and caregivers prepare for the final stages of life.

Emotional and Ethical Considerations in Dementia Death
The journey through dementia is not just a medical or biological experience; it is also a deeply emotional one. Families grappling with the slow erosion of a loved one’s personality and memory often experience what is known as anticipatory grief. They begin mourning the loss long before death arrives, making the eventual passing both a sorrow and a release. In this emotional landscape, questions like do people die from dementia carry immense weight.
Ethically, the knowledge that dementia can cause death complicates decisions about feeding tubes, resuscitation efforts, and aggressive interventions. Families and clinicians must navigate the delicate balance between prolonging life and preventing suffering. Advance directives and healthcare proxies are valuable tools that allow individuals to express their wishes before cognitive decline limits their ability to participate in medical decisions. Understanding that dementia death is a medical and emotional reality helps all parties involved prepare for the inevitable.
Public Awareness and the Language of Dementia
Despite growing awareness, many people still resist the idea that dementia can be a direct cause of death. Euphemistic phrases like “passed away due to old age” or “complications related to dementia” can obscure the truth and prevent informed conversations. To address this gap, public health campaigns are working to reframe the dialogue around dementia as a life-limiting disease.
Answering the question, can people die from dementia, involves more than citing statistics. It requires a cultural shift in how we understand, discuss, and manage the condition. Accurate language can empower families, encourage early diagnosis, and promote realistic expectations for the disease course. It also helps destigmatize the condition, allowing for better resource allocation and caregiver support. In this light, acknowledging that dementia leads to death becomes an act of advocacy.
Planning Ahead: Legal, Medical, and Financial Preparations
Given the progressive and ultimately terminal nature of dementia, early planning is not just advisable—it is essential. Legal documents such as powers of attorney and living wills can ensure that an individual’s preferences are honored even after cognitive function declines. Financial planning can prevent unnecessary hardship and allow for better care options. Understanding that will dementia cause death shifts these discussions from hypothetical to practical.
Medical planning should also include conversations about palliative and end-of-life care. These discussions can reduce stress and prevent crisis-driven decisions when the disease reaches its final stages. Families who recognize that is dementia a deadly disease often find solace in knowing they have respected their loved one’s values and choices. The process of preparation is not just logistical but deeply compassionate.
Scientific Advances and the Hope for Change
While the outlook for dementia remains grim, ongoing research offers glimmers of hope. Advances in neuroimaging, biomarkers, and pharmacological interventions are improving our ability to detect and possibly delay the progression of dementia. Clinical trials investigating new drugs and therapeutic approaches aim to modify the disease course or alleviate symptoms.
However, even as science pushes boundaries, the current reality remains: dementia is a terminal condition for which there is no cure. Recognizing this does not diminish the importance of research but rather underscores its urgency. Every breakthrough holds the promise of reducing the number of families who must ask, does a person die from dementia, and live through the long journey to that answer.
The Caregiver Experience: Witnessing the Progression
Caregivers occupy a unique vantage point in the narrative of dementia. They see firsthand the slow unraveling of memory, identity, and autonomy. For them, the question, is dementia a fatal disease, is not abstract but part of daily life. They observe the transition from forgetfulness to dependency, from confusion to silence.
Supporting a person with dementia requires not only physical labor but emotional endurance. Caregivers often become experts in their own right, learning how to manage behavioral symptoms, coordinate medical appointments, and provide comfort. They are also the ones who bear witness to the final decline—when speech stops, when food is refused, when the eyes no longer recognize familiar faces. It is in these moments that the truth becomes undeniable: dementia can lead to death.
Why Acknowledging Dementia as a Cause of Death Matters
The reluctance to classify dementia as a terminal illness has real consequences. It can delay access to hospice care, reduce funding for research, and undermine caregiver support systems. By acknowledging that can a person die of dementia is a legitimate and frequent medical outcome, we open the door to better care models, more informed policy, and deeper compassion.
Healthcare professionals, researchers, and families must align in recognizing the full implications of dementia. Only then can we ensure that those living with the condition—and those who care for them—receive the support they need. In this way, accepting the reality that can dementia lead to death becomes not an admission of defeat but a commitment to dignity, empathy, and preparedness.
Frequently Asked Questions: Can Dementia Lead to Death? Exploring Its Role as a Cause of Death and Its Broader Impact
1. Can dementia directly cause death, or is it usually a secondary factor?
While dementia may not always be listed as the immediate cause of death, it often plays a central and direct role in the dying process. Over time, cognitive decline impairs basic neurological functions like swallowing and breathing, which can lead to complications such as aspiration pneumonia or sepsis. These medical events may be the final recorded cause, but dementia creates the underlying vulnerability that allows them to occur. So, can dementia cause death in and of itself? Yes, it absolutely can, especially in its advanced stages where cognitive impairment leads to systemic organ decline. Understanding that dementia cause of death is medically valid helps frame treatment decisions and care goals more accurately.
2. Why do some people not realize that dementia can be fatal?
Many individuals associate dementia primarily with memory loss, overlooking its systemic effects on the body. There’s a widespread misconception that people simply live with dementia until another unrelated condition causes their death. This belief leads to the common misunderstanding that you don’t die from dementia. However, medical experts increasingly affirm that dementia is not only progressive but terminal. Public health communication has lagged in clearly stating that yes, can a person die of dementia, and more often than not, they do.
3. How can families emotionally prepare for dementia death when it unfolds so slowly?
One of the most challenging aspects of dementia is its gradual erosion of identity and function. Families are often caught between hope and grief, struggling to reconcile a loved one’s physical presence with the absence of their personality. Recognizing early on that dementia can lead to death enables families to engage in advance care planning, allowing patients to express their wishes while they still have capacity. Although the trajectory may span years, knowing that dementia death is probable helps shift the focus from cure to comfort. It also allows loved ones to begin the emotional work of anticipatory grieving, which can soften the final blow.
4. Are there cases where someone with dementia dies unexpectedly?
Yes, and this is often due to complications exacerbated by the underlying cognitive decline. A person with moderate dementia who appears stable may still be at high risk for sudden infections, unnoticed injuries, or cardiac events. Since people with dementia may not communicate symptoms effectively, life-threatening issues can escalate quickly. This reality reinforces that yes, can someone die from dementia unexpectedly—particularly when preventive measures are overlooked. The apparent unpredictability of dementia death often masks the fact that the disease had already set the stage for rapid decline.
5. How does the healthcare system respond to the idea that dementia is a deadly disease?
Recognition of dementia as a terminal illness is growing within the healthcare system, but implementation is still uneven. Some clinicians may still hesitate to describe dementia as fatal, especially when talking to families. Yet palliative care and hospice services are increasingly structured around the understanding that does dementia cause death is not just a theoretical concept but a clinical reality. Systems that openly acknowledge that can people die from dementia are better positioned to provide supportive, goal-concordant care. This shift is essential to ensuring dignity and quality of life in the final stages.
6. Does the type of dementia affect how likely it is to lead to death?
Absolutely. While all forms of dementia are life-limiting, certain subtypes progress more aggressively. For example, Creutzfeldt-Jakob disease and Lewy body dementia often have faster trajectories than typical Alzheimer’s disease. Vascular dementia, on the other hand, may result in more abrupt declines due to strokes. This variation underscores the reality that can dementia lead to death in different ways, depending on its origin. Knowing the subtype can help families anticipate complications and plan accordingly for a likely dementia death.
7. What are some signs that indicate a person with dementia is nearing the end of life?
Common indicators include significant weight loss, repeated infections, withdrawal from social interaction, loss of speech, and difficulty swallowing. These symptoms suggest the body is losing its ability to maintain basic functions, and that the progression has reached a critical stage. In many cases, families begin to ask questions like, does a person die from dementia now, or is this another plateau? Recognizing these signs helps caregivers and medical teams transition from curative treatments to palliative approaches. It’s also a moment to reaffirm that yes, is dementia a fatal disease and its end stage is unfolding.
8. How does cultural perception shape our understanding of dementia as a terminal illness?
In many cultures, cognitive decline is seen as a normal part of aging rather than a medical condition. This perception delays diagnosis, care planning, and honest discussions about prognosis. In some cases, even asking, will you die from dementia, is considered taboo. However, greater awareness and education are slowly changing these narratives, especially in communities where dementia rates are rising. By confronting the question—can you die from dementia—we create space for better care and cultural acceptance of aging and dying.
9. What steps can be taken to ensure dementia-related deaths are accurately recorded?
Accurate recording on death certificates is essential for research, funding, and public health policy. Clinicians must be trained to identify dementia as the underlying cause, even when another condition appears as the final trigger. When a person dies from pneumonia but had end-stage dementia, the record should reflect that dementia was a contributing or primary factor. This transparency allows for more reliable data on how often does dementia lead to death and validates it as a public health crisis. Better data can drive improvements in diagnosis, caregiver support, and long-term care funding.
10. What promising innovations are emerging in response to the fatal nature of dementia? Researchers are exploring disease-modifying treatments, biomarkers for early detection, and non-pharmacological therapies to slow cognitive decline. Artificial intelligence and wearable technologies are also being deployed to monitor behavioral and physiological changes that precede crisis points. These tools could help families and clinicians intervene earlier, possibly extending quality of life. As awareness grows that will dementia cause death if unchecked, the medical field is doubling down on both prevention and compassionate care. While a cure may still be distant, acknowledging that dementia is a deadly disease has galvanized innovation and collaboration across disciplines.
Final Reflections: Embracing the Reality of Dementia Death with Compassion and Clarity
Coming to terms with the fact that dementia can cause death is not an easy task. It challenges our understanding of illness, aging, and what it means to provide care in the face of inevitable decline. But by asking difficult questions—such as can dementia lead to death or is dementia a fatal disease—we allow ourselves to approach this condition with greater honesty and intention. These inquiries are not merely clinical but deeply human.
Recognizing dementia as a cause of death empowers families to prepare, not only logistically but emotionally. It enables healthcare providers to deliver care that honors the patient’s dignity and aligns with their values. It also contributes to a broader societal shift—one that acknowledges the true scope of dementia’s impact and responds with compassion, science, and hope. In the end, understanding that dementia death is real does not diminish life; rather, it encourages us to cherish what remains and to face the future with eyes wide open.
end-of-life dementia care, stages of dementia progression, terminal illnesses in elderly, how dementia progresses, palliative care for dementia, dementia hospice eligibility, cognitive decline and mortality, Alzheimer’s late stage symptoms, neurological diseases and death, elderly care planning, dementia patient life expectancy, impact of dementia on health, brain diseases in aging, neurological deterioration, caregiving in dementia, death from neurodegenerative disease, dementia and aspiration pneumonia, planning for dementia end-of-life, signs of terminal dementia, dementia comorbidities and risks
Further Reading:
Does having dementia affect a person’s life expectancy?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.