For millions of individuals navigating daily life, anxiety isn’t just a mental or emotional experience—it can also manifest physically. Among the most frequently reported physical symptoms is gastrointestinal distress, particularly in the form of abdominal discomfort. But can anxiety cause stomach pain in a medically recognized way? Increasing research into the gut-brain axis is not only affirming that connection, but also reshaping how clinicians understand and treat anxiety-related somatic symptoms. This article explores the intricate physiological relationship between stress, anxiety, and digestive discomfort while providing research-backed insights into how to calm a nervous stomach and manage anxiety-induced gastrointestinal symptoms.
You may also like: How Gut Health Affects Mental Health: Exploring the Gut-Brain Connection Behind Anxiety, Mood, and Depression
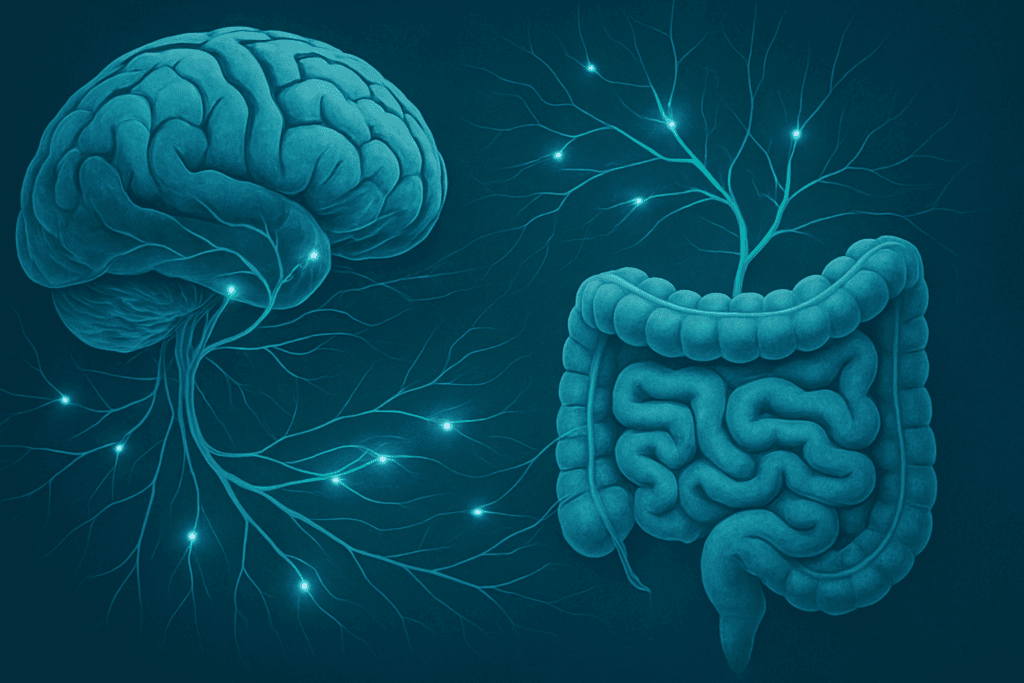
The Gut-Brain Axis: How Anxiety Impacts Digestive Health
The gut and brain are intimately connected through a bidirectional communication network often referred to as the gut-brain axis. This system involves complex interactions between the central nervous system (CNS), the enteric nervous system (ENS), the hypothalamic-pituitary-adrenal (HPA) axis, and the microbiome. The ENS, sometimes called the “second brain,” governs digestive processes and contains more than 100 million neurons. When psychological stressors activate the HPA axis, the body enters a state of heightened alert, releasing cortisol and other stress hormones that directly impact gut motility, enzyme secretion, and intestinal permeability.
This physiological cascade explains why anxiety stomach pain is such a common complaint. For individuals living with chronic anxiety, persistent activation of the stress response can lead to dysregulation in digestive processes, making them more susceptible to symptoms like cramping, bloating, nausea, and even changes in bowel habits. In clinical terms, this is known as abdominal pain with stress or anxiety abdominal pain. What makes this phenomenon more than just anecdotal is the growing body of evidence connecting anxiety to disorders like irritable bowel syndrome (IBS), functional dyspepsia, and even leaky gut.

What Does Anxiety Stomach Pain Feel Like?
Understanding what anxiety stomach pain feels like is essential for distinguishing it from other gastrointestinal conditions. Unlike sharp, localized pain typically caused by structural issues such as ulcers or gallstones, anxiety-related discomfort often presents as diffuse, cramping sensations. Some individuals describe it as a fluttering or tightening feeling in the upper abdomen—a condition frequently referred to as a nervous stomach or anxiety tummy pain.
Anxiety stomach ache is not uniform in its presentation. For some, it may manifest as a dull ache that intensifies during moments of heightened emotional distress. For others, it can be a persistent sense of fullness, pressure, or even mild nausea that accompanies ongoing worry or fear. These sensations are often exacerbated by anticipatory anxiety, such as before public speaking or important life events. The subjective experience may also include symptoms that mimic gastrointestinal infections, making clinical assessment more challenging. Recognizing anxiety symptoms in the stomach as distinct from other medical conditions is key to avoiding unnecessary interventions and focusing treatment on the underlying anxiety disorder.
Stomach Cramps, Anxiety Disorder, and Diagnostic Complexity
When stomach cramps occur alongside an anxiety disorder, it can be difficult for both patients and clinicians to disentangle the root cause. While stomach cramps are typically associated with infections or food intolerances, they are also well-documented features of generalized anxiety disorder (GAD) and panic disorder. These cramps can range from mildly uncomfortable to debilitating and may fluctuate in intensity throughout the day, particularly during periods of acute stress.
Clinically, stomach cramps in an anxiety disorder context are classified as functional gastrointestinal symptoms. They exist in the absence of identifiable structural or biochemical abnormalities and are thought to arise from hypersensitivity in the gut. Individuals with anxiety often have an exaggerated perception of visceral sensations, a phenomenon known as visceral hyperalgesia. This heightened sensitivity amplifies the perception of normal digestive activity, translating routine gut function into painful or distressing experiences. This is where the term anxiety abdominal pain becomes especially relevant, encompassing a wide range of somatic symptoms tied to psychological distress.
Can Stress Cause Stomach Pain? The Physiological Link
It is a medically established fact that stress can cause stomach pain. Acute stress triggers the fight-or-flight response, which reroutes blood away from the gastrointestinal tract toward muscles and vital organs. This redirection compromises digestion and slows gastric emptying, leading to bloating, indigestion, and pain. Chronic stress maintains this imbalance over time, damaging the protective mucosal lining of the stomach and increasing the risk of inflammation and hypersensitivity.
The association between stress and stomach pain is also supported by studies on inflammatory markers. Individuals under chronic stress often exhibit elevated levels of cytokines and other pro-inflammatory agents that can increase gut permeability. This leads to what is colloquially called a “leaky gut,” allowing antigens and toxins to enter the bloodstream and trigger systemic immune responses. While the concept remains debated, it illustrates how stress and stomach pain can be intimately linked at a cellular level. Stress belly pain, a term sometimes used to describe the bloating and cramping caused by anxiety, reflects this underlying pathophysiology.
Recognizing Nervous Stomach Symptoms and Triggers
A nervous stomach is more than just a metaphor—it is a legitimate physiological response to psychological stress. Common nervous stomach symptoms include churning sensations, bloating, excessive gas, acid reflux, and intermittent constipation or diarrhea. These symptoms often appear in tandem with stressful situations and can become chronic in individuals with untreated anxiety or high-stress lifestyles.
Triggers for a nervous stomach vary by individual but typically include performance anxiety, interpersonal conflict, financial worries, and health-related fears. In individuals with high trait anxiety, even minor stressors can provoke significant gastrointestinal symptoms. Environmental factors such as caffeine consumption, sleep disruption, and dietary habits can further exacerbate the condition. This makes it crucial to approach treatment from a holistic perspective, targeting both psychological and physiological contributors.
Can Anxiety Give You Gas or Other Digestive Symptoms?
An often-overlooked aspect of anxiety’s impact on the gut is its ability to alter gas production and bowel habits. The question “can anxiety give you gas?” is not only valid—it is supported by emerging research. Anxiety increases aerophagia, or the swallowing of air, especially in individuals who hyperventilate or experience frequent panic attacks. This leads to an increase in intestinal gas, bloating, and even belching, contributing to the overall discomfort of an anxious stomach.
In addition to gas, anxiety can disrupt the normal microbial balance in the gut, a phenomenon known as dysbiosis. Studies have shown that individuals with chronic anxiety or depression often have lower microbial diversity and higher levels of pathogenic bacteria, which can exacerbate gastrointestinal symptoms. This microbial imbalance can result in increased fermentation of food in the colon, producing more gas and leading to further bloating and discomfort. As such, anxiety stomach issues go beyond transient discomfort—they represent a multifaceted interaction between the mind, the nervous system, and the gut microbiota.

How to Help a Nervous Stomach from Anxiety
Managing a nervous stomach begins with addressing the root cause: anxiety. Cognitive behavioral therapy (CBT) remains one of the most effective interventions, helping individuals identify and reframe maladaptive thought patterns that contribute to stress-related symptoms. CBT can be particularly helpful for patients experiencing anxiety tummy ache or chronic anxiety abdominal pain, as it combines cognitive restructuring with behavioral exposure techniques to reduce visceral sensitivity.
Mindfulness-based interventions, including meditation, breathing exercises, and progressive muscle relaxation, have also demonstrated efficacy in reducing both psychological and somatic symptoms. These techniques activate the parasympathetic nervous system, promoting a state of rest and digestion. In cases where psychological interventions alone are insufficient, pharmacological options such as selective serotonin reuptake inhibitors (SSRIs) or gut-directed antibiotics like rifaximin (for diagnosed IBS cases) may be considered. Dietary modifications, including the adoption of a low-FODMAP diet, can reduce symptoms by minimizing fermentable carbohydrates that contribute to gas and bloating. Importantly, these treatments should be guided by a healthcare professional to ensure an individualized and evidence-based approach.

Can Anxiety Cause Stomach Aches and Chronic Gastrointestinal Problems?
The relationship between chronic anxiety and persistent gastrointestinal issues is both clinically recognized and well-documented. When individuals ask, “can anxiety cause stomach aches on an ongoing basis?” the answer, increasingly, is yes. Repeated activation of the stress response system can lead to changes in gut sensitivity, motility, and inflammation, contributing to long-term conditions like IBS, functional dyspepsia, and even small intestinal bacterial overgrowth (SIBO).
Can anxiety cause stomach problems that evolve into chronic illnesses? In many cases, yes—especially when anxiety goes untreated. Chronic exposure to cortisol and other stress hormones can weaken gut immunity and increase vulnerability to gastrointestinal infections and inflammatory conditions. Over time, these physiological alterations can become self-reinforcing, where the presence of digestive symptoms further exacerbates anxiety, creating a vicious cycle. Breaking this cycle requires a combination of psychological therapy, lifestyle changes, and, when appropriate, medical or dietary intervention. This reinforces the idea that addressing anxiety is not only critical for mental well-being but also essential for maintaining long-term digestive health.
Does Stress and Anxiety Cause Stomach Pain in Children and Adolescents?
The gut-brain connection is not limited to adults. Children and adolescents are equally susceptible to stress-related gastrointestinal symptoms. Pediatric patients often lack the verbal ability to articulate emotional distress, making somatic symptoms like stomach pain one of the earliest indicators of anxiety. In school-aged children, complaints of stomach aches often correlate with academic stress, bullying, or separation anxiety.
Does stress cause stomach aches in young people in the same way it does in adults? While the underlying mechanisms are similar, children’s nervous systems are still developing, which may make them more reactive to environmental and emotional stimuli. Early intervention is crucial, as untreated anxiety in childhood is associated with a higher risk of developing functional gastrointestinal disorders later in life. Behavioral therapy, parental support, and, in some cases, pediatric psychiatric consultation are essential components of an effective treatment plan. As with adults, recognizing anxiety symptoms in the stomach can prevent unnecessary medical testing and reduce the long-term burden of both mental and physical illness.

How to Stop Stomach Pain from Anxiety: A Multi-Faceted Approach
Stopping stomach pain from anxiety requires a comprehensive approach that addresses both mind and body. Psychological therapies, particularly those rooted in cognitive behavioral frameworks, help reduce the cognitive distortions that perpetuate anxiety. Exposure therapy and acceptance and commitment therapy (ACT) are particularly effective in addressing fear-based thinking, which often fuels physiological symptoms.
On the physiological side, gut-directed therapies—including probiotics, herbal remedies like peppermint oil, and even acupuncture—have shown promise in managing anxiety tummy pain. Dietary strategies such as reducing caffeine, processed sugar, and alcohol can also alleviate symptoms by minimizing gut inflammation and reducing nervous system reactivity. For individuals whose anxiety symptoms in the stomach are severe or disabling, a combination of psychiatric medication and gastroenterological intervention may be necessary. The key is to personalize treatment based on individual symptom profiles, medical history, and psychological needs. Lifestyle modifications such as regular exercise, improved sleep hygiene, and stress management techniques complete the treatment picture.
Frequently Asked Questions: Anxiety, Stress, and Stomach Pain
1. Can anxiety cause stomach pain even if I don’t feel mentally anxious?
Yes, anxiety can cause stomach pain even when you’re not consciously experiencing mental stress. This is because the body’s physiological stress responses often occur beneath conscious awareness. The nervous system may still activate the stress response, leading to changes in gut motility, muscle tension, and acid production. People often describe vague or cramping abdominal pain with stress without associating it with emotional triggers, especially if their anxiety has become chronic. So if you experience anxiety stomach pain but don’t feel particularly anxious, your body may still be reacting to underlying psychological tension.
2. What does anxiety stomach pain feel like when it lasts all day?
When anxiety stomach pain persists throughout the day, it often feels like a low-grade, gnawing ache, pressure, or tightness in the upper abdomen. Some people describe it as an ongoing queasiness or heaviness that doesn’t respond to food or rest. This type of anxiety tummy pain can become more noticeable during idle moments, such as sitting in meetings or trying to fall asleep. The pain may wax and wane but rarely resolves completely without stress management techniques. Chronic anxiety symptoms in the stomach like these can make it difficult to differentiate between psychological and physical causes of discomfort.
3. Can anxiety cause stomach aches that mimic food intolerance or IBS?
Absolutely. Anxiety can cause stomach aches and digestive changes that closely resemble irritable bowel syndrome (IBS) or food sensitivities. These include gas, bloating, diarrhea, and abdominal pain with stress. In fact, many individuals first explore dietary triggers before realizing that emotional patterns are driving the symptoms. In cases of stomach cramps anxiety disorder presentations, misdiagnosis is common until the role of chronic stress or worry is considered. Keeping a journal of both emotional states and digestive symptoms can reveal correlations that point toward an anxious stomach rather than a dietary intolerance.
4. What’s the difference between a nervous stomach and a stomach virus?
A nervous stomach and a viral stomach illness may share overlapping symptoms, but there are key differences. Nervous stomach symptoms tend to fluctuate with emotional stress and are rarely accompanied by fever, body aches, or vomiting. The discomfort is often more diffuse, and symptoms like gas or anxiety tummy ache may worsen in anticipation of stressful events. Conversely, a stomach virus usually has a sudden onset, includes systemic symptoms, and runs its course in a few days. Understanding these distinctions is essential in determining whether you’re dealing with anxiety stomach pain or an acute infection.
5. Can anxiety give you gas even without dietary triggers?
Yes, anxiety can give you gas independently of food-related factors. When you’re anxious, you may unconsciously swallow more air—a phenomenon called aerophagia—which increases intestinal gas. Additionally, stress alters gut motility and can change how food moves through your digestive tract, contributing to fermentation and gas buildup. People with anxiety stomach ache often report frequent belching or flatulence even when eating a clean diet. Therefore, if you’re struggling with gas and bloating but can’t identify a food cause, consider whether anxiety or nervous stomach symptoms might be contributing.
6. Are there long-term risks if I ignore anxiety-related abdominal pain?
Yes, ignoring anxiety abdominal pain can lead to long-term consequences. Chronic stress and unaddressed anxiety can perpetuate inflammation in the gut, disrupt the microbiome, and increase the risk for functional gastrointestinal disorders like IBS or SIBO. Additionally, when left unmanaged, anxiety symptoms in the stomach can increase the risk of mental health deterioration, such as the development of panic attacks or depressive episodes. What begins as a mild anxious stomach can evolve into persistent digestive issues that require more intensive intervention. Early treatment of both the anxiety and stomach symptoms is key to preventing escalation.
7. How do hormonal cycles affect anxiety stomach symptoms in women?
Hormonal fluctuations during the menstrual cycle can significantly affect anxiety stomach symptoms. Estrogen and progesterone influence serotonin levels, gut motility, and pain sensitivity. As a result, many women experience worsened anxiety tummy pain or stomach cramps anxiety disorder patterns in the days leading up to menstruation. Some also report increased bloating, cramping, or acid reflux linked to cyclical hormonal shifts. If anxiety stomach pain seems to worsen predictably each month, tracking menstrual patterns alongside stress levels may reveal important insights and inform personalized treatment strategies.
8. Can anxiety stomach pain interfere with appetite or eating habits?
Yes, anxiety stomach pain often leads to disrupted appetite and disordered eating patterns. Some individuals feel too nauseated to eat, while others develop a fear of eating due to associations between food and stomach pain and anxiety disorder symptoms. This aversion can create a vicious cycle, where inadequate nutrition further exacerbates physical and emotional symptoms. In cases of severe anxiety abdominal pain, people may skip meals, binge eat, or adopt overly restrictive diets in an attempt to control symptoms. Addressing both the psychological and nutritional aspects is essential to restoring a healthy relationship with food.
9. Are there specific breathing techniques that help relieve anxiety tummy ache?
Targeted breathing exercises can significantly reduce anxiety tummy ache by calming the autonomic nervous system. Techniques like diaphragmatic breathing, box breathing (inhaling for 4 counts, holding for 4, exhaling for 4), and paced breathing all engage the parasympathetic system. This helps lower cortisol levels, reduce muscle tension, and improve blood flow to the digestive tract. Practicing these techniques before meals or during flare-ups can reduce abdominal pain with stress and promote digestive ease. For long-term benefit, incorporating breathwork into daily routines may prevent the buildup of stress-related stomach pain.
10. How can I explain my anxious stomach to people who don’t understand it?
Describing an anxious stomach to others can be difficult, especially when symptoms seem invisible. One helpful approach is to compare it to stage fright or motion sickness—familiar examples of stress and stomach pain working together. Emphasize that anxiety tummy pain is a genuine, physiological response to emotional stimuli, not just “in your head.” You might also mention that chronic anxiety causes changes in gut function and can feel like nausea, tightness, or pressure even in calm settings. By framing your nervous stomach symptoms within the context of the gut-brain connection, you can help others appreciate the legitimacy of your experience.
Final Thoughts on Managing Anxiety Stomach Pain and the Gut-Brain Connection
Understanding the connection between anxiety and gastrointestinal symptoms is no longer just an area of theoretical interest—it’s a clinical imperative. As research continues to reveal the deep interconnectivity between the brain and digestive system, it becomes increasingly clear that anxiety stomach pain is not only real but also treatable. Whether you’re experiencing a nervous stomach before a big event or struggling with chronic anxiety tummy ache, recognizing the gut as a central player in mental health opens the door to more effective, holistic treatment options.
The answer to “can anxiety cause stomach pain?” is a resounding yes—but with that understanding comes empowerment. By integrating psychological therapies, dietary changes, and lifestyle strategies, individuals can begin to reclaim control over their digestive and emotional well-being. From children grappling with stress belly pain to adults navigating complex anxiety disorders, the journey toward healing often begins with acknowledging the body’s role in emotional expression. With proper care, patience, and the right support system, it is entirely possible to restore balance to both the mind and the gut.
Further Reading:
Stress-related stomach pain: When to see a doctor
Do You Have a Nervous Stomach?
How to overcome anxiety and stomach issues
.