Understanding Brain Trauma: What Happens After a Head Injury
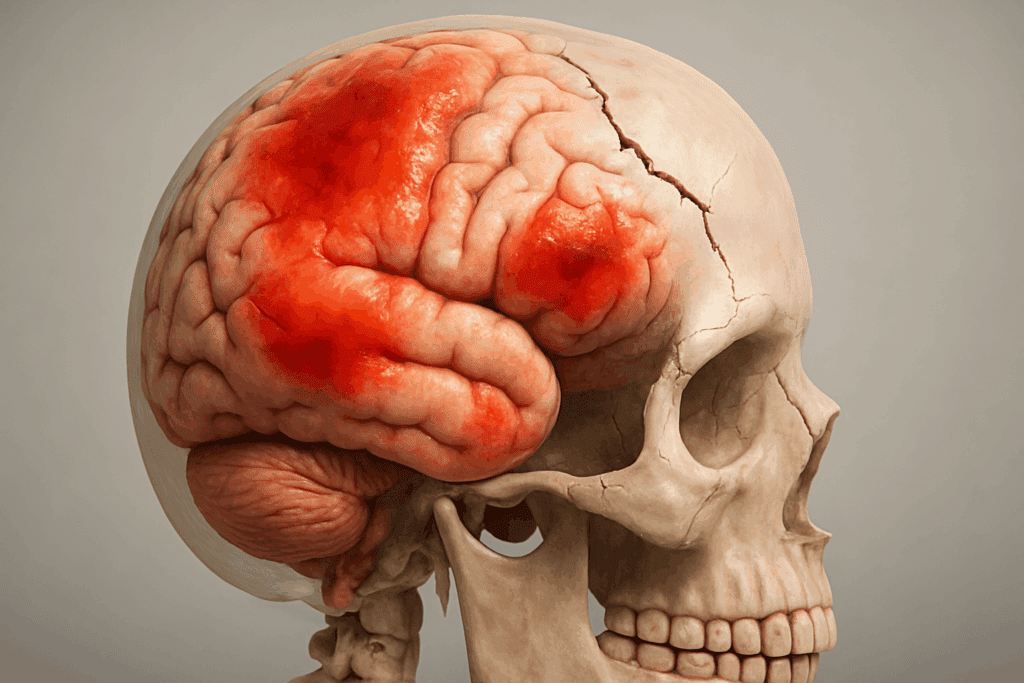
When the human brain sustains trauma—whether from a blunt force injury, fall, motor vehicle accident, or violent impact—the effects can be far-reaching and deeply disruptive. Traumatic brain injuries (TBIs) vary in severity, but even mild cases can result in long-term complications if left unaddressed. These injuries often involve not only the neural tissues themselves but also surrounding structures such as the meninges, blood vessels, and even the skull. In cases where the trauma causes a skull fracture, the injury becomes particularly complex, potentially increasing the risk of brain swelling, bleeding, and infection. Understanding the underlying damage is the first step in appreciating the significance of effective intervention. Many survivors experience immediate symptoms like loss of consciousness, confusion, headaches, or nausea. However, more insidious effects—such as memory loss, emotional instability, concentration difficulties, and mood disturbances—can surface days or weeks after the incident.
Given the brain’s central role in every aspect of physical and cognitive function, rehabilitation becomes not merely a supportive strategy but a medical necessity. When the brain’s normal operations are disrupted, the consequences ripple outward, affecting personality, behavior, decision-making, and basic self-care. This is where brain trauma rehabilitation emerges as a critical element of recovery. It provides structured and personalized interventions aimed at restoring or compensating for lost abilities. Equally important is the need for timely, comprehensive rehab for brain damage, which not only helps repair the injury’s direct consequences but also safeguards mental health. Anxiety, depression, post-traumatic stress, and emotional dysregulation frequently follow brain injuries and skull fractures, intensifying the need for integrated care that bridges physical and psychological domains.
Medical science has advanced considerably in understanding the brain’s plasticity—its ability to adapt, rewire, and regain function even after significant injury. Rehabilitation taps into this capacity through targeted therapies such as neuropsychological training, physical therapy, occupational therapy, and speech-language pathology. The process can be slow and nonlinear, but consistent, evidence-based rehab on skull fracture to heal underlying neural injury can dramatically enhance long-term outcomes. Importantly, a successful rehabilitation plan is not merely about mobility or memory but also about restoring emotional balance and personal independence. This holistic approach underscores the inextricable link between physical healing and psychological resilience, especially for those navigating the aftermath of traumatic brain events.
You may also like: Boost Brain Power Naturally: Evidence-Based Cognitive Training Activities and Memory Exercises That Support Long-Term Mental Health

The Role of Multidisciplinary Teams in Brain Trauma Rehabilitation
The complexity of brain trauma requires a level of care that extends far beyond the scope of any single discipline. In fact, the gold standard for effective brain trauma rehabilitation is the use of a multidisciplinary team approach. This model integrates the skills and insights of a range of professionals, including neurologists, neuropsychologists, physical therapists, occupational therapists, speech and language pathologists, rehabilitation nurses, and social workers. Each member plays a vital role in addressing the multifaceted effects of brain injury, which often intersect across physical, emotional, cognitive, and behavioral domains. By working collaboratively, these experts develop comprehensive treatment plans that reflect the unique needs and goals of each individual.
Rehab for brain damage, particularly when complicated by a skull fracture, is rarely a linear path. The presence of a fractured skull may necessitate surgical intervention, close neurological monitoring, and a cautious reintroduction of physical activities. These steps require not only medical precision but also psychological support to help patients cope with the trauma and uncertainty surrounding their recovery. In this context, neuropsychologists are crucial in assessing cognitive deficits and emotional disturbances, helping to craft interventions that re-train neural pathways or develop compensatory strategies. Simultaneously, physical and occupational therapists focus on restoring mobility, coordination, and daily functional skills, ensuring that patients can regain a sense of agency and autonomy in their everyday lives.
Communication is another domain frequently affected by traumatic brain injuries, which is where speech-language pathologists become indispensable. Whether a patient is struggling with expressive language, receptive understanding, or cognitive-linguistic deficits, these professionals design therapies that promote both verbal and non-verbal communication. This is particularly important for individuals who may not be able to fully express their emotional experiences—a common challenge in brain trauma rehabilitation. Moreover, rehabilitation nurses ensure continuity of care across settings, helping patients and their families navigate the complex landscape of medications, therapy schedules, and long-term care planning. Social workers and case managers also contribute by offering emotional support, coordinating community resources, and facilitating smooth transitions between hospital and home.
In cases where rehab on skull fracture to heal underlying damage is required, the collaboration between orthopedic and neurological specialists becomes paramount. These experts must monitor healing progress while ensuring that no secondary complications—such as infection or cerebrospinal fluid leaks—impede recovery. Mental health professionals round out the team by addressing depression, anxiety, and PTSD, which can be both a cause and consequence of injury-related disability. Together, this multidisciplinary approach ensures that patients receive not just medical treatment but holistic care that fosters healing in every dimension—physical, emotional, and psychological. Such a comprehensive model exemplifies the importance of collaboration in achieving optimal outcomes for those undergoing brain trauma rehabilitation.

How Cognitive and Emotional Recovery Go Hand in Hand
One of the most significant insights emerging from contemporary neuroscience is the recognition that cognitive and emotional recovery are deeply interdependent. While rehab for brain damage often focuses on restoring cognitive functions such as memory, attention, and executive control, these efforts are unlikely to succeed if emotional health is not concurrently addressed. The aftermath of a traumatic brain injury often involves disruptions to the brain’s limbic system, which regulates emotions, motivation, and interpersonal connections. As a result, patients may experience heightened irritability, mood swings, depression, or emotional numbness. These changes are not merely psychological reactions to trauma but are frequently rooted in physiological disruptions caused by the injury itself.
Addressing these emotional challenges is crucial not only for the patient’s psychological well-being but also for the effectiveness of cognitive rehabilitation. Emotional dysregulation can hinder concentration, reduce motivation, and impair learning—all of which are essential for cognitive recovery. This is why modern approaches to brain trauma rehabilitation increasingly incorporate psychological therapies as a core component. Cognitive-behavioral therapy (CBT), mindfulness training, and supportive counseling are frequently used to help patients process their experiences, develop emotional resilience, and rebuild a sense of identity and purpose. These interventions can be particularly vital in cases involving a skull fracture, where the visual reminder of injury may exacerbate distress or contribute to feelings of vulnerability.
When embarking on rehab for skull fracture to heal not just the bone but the mind, it’s essential to consider how trauma reshapes self-perception. Many patients report feelings of alienation from their former selves, especially when cognitive impairments alter their work, relationships, or independence. The role of therapists, then, becomes one of helping individuals reconstruct their narrative—guiding them to find meaning and continuity in their post-injury lives. Moreover, family therapy can play a crucial role in this phase, as loved ones often struggle to understand the changes in behavior and personality that may accompany brain trauma. Empowering families with knowledge and strategies to support recovery creates a more stable and nurturing environment, which can significantly accelerate healing.
In addition to psychological counseling, some rehabilitation centers employ expressive therapies such as art or music therapy to foster emotional expression and neurological healing simultaneously. These modalities can help patients access emotions that are difficult to articulate, offering a powerful complement to more traditional forms of talk therapy. Integrating such therapies into a broader rehab for brain damage framework highlights the evolving understanding that recovery is not merely about symptom resolution but about restoring wholeness. Ultimately, recognizing the symbiotic relationship between emotional health and cognitive functioning allows for more personalized, compassionate, and effective rehabilitation strategies—ones that honor the full spectrum of human experience.

Rehabilitation Tools and Techniques That Accelerate Healing
The tools and techniques used in brain trauma rehabilitation are as diverse and dynamic as the patients they serve. Rehabilitation professionals employ a wide array of modalities that target different aspects of brain function, often combining traditional therapies with innovative, tech-enhanced approaches. One foundational tool in the rehab for brain damage process is neuropsychological assessment. These tests help identify specific deficits in memory, processing speed, attention, and problem-solving abilities, which then guide the formulation of individualized treatment plans. Cognitive training programs—delivered either in person or through digital platforms—are then used to strengthen these targeted areas, harnessing the brain’s neuroplasticity to rebuild connections and enhance function.
Physical and occupational therapies remain cornerstones of recovery, especially when the injury has compromised motor skills or physical coordination. Exercises are carefully designed to improve balance, strength, and flexibility, with the goal of restoring independence in everyday tasks. For individuals undergoing rehab on skull fracture to heal, these sessions must be tailored to avoid excessive strain or pressure on the healing bone. Therapists are trained to monitor patients for signs of discomfort or regression, adjusting routines as necessary to ensure safe progression. Additionally, functional electrical stimulation (FES), gait training systems, and virtual reality platforms are increasingly being integrated into physical rehabilitation, offering immersive and interactive experiences that accelerate neuro-motor recovery.
Another powerful modality in the context of brain trauma rehabilitation is speech and language therapy. Many patients experience disruptions in verbal fluency, comprehension, and communication following a brain injury. Through guided exercises and structured practice, speech therapists help patients regain the ability to express themselves clearly and engage meaningfully with others. This is particularly crucial in rebuilding social relationships and professional capabilities, both of which are integral to mental and emotional healing. Advances in assistive communication devices also provide alternative pathways for expression in patients with severe impairments, demonstrating how technology can enhance accessibility and dignity during the recovery process.
Biofeedback and neurofeedback therapies are also gaining traction as tools for helping patients develop greater awareness and control over their physiological responses. These techniques are especially helpful for managing stress, anxiety, and emotional regulation—challenges that frequently arise after brain trauma. In rehab for brain damage that incorporates these tools, patients learn to recognize internal signals such as heart rate variability or brain wave patterns, then use techniques like deep breathing or guided visualization to modulate their responses. Over time, this can lead to greater self-regulation, improved sleep, and reduced emotional volatility. When used in tandem with more traditional rehabilitation methods, these innovative approaches can dramatically enhance the speed and quality of recovery, reaffirming the need for personalized, multifaceted treatment strategies.

Long-Term Mental Health Outcomes and Lifelong Support Strategies
While the initial phase of brain trauma rehabilitation is often intensive and highly structured, the need for support rarely ends when formal therapy concludes. In fact, many individuals face long-term challenges that require ongoing care, adaptations, and vigilance. The lingering effects of traumatic brain injuries can manifest in subtle yet persistent ways, influencing cognition, emotional regulation, and interpersonal relationships for years or even decades. For this reason, long-term support systems are essential—not only to maintain progress but to ensure continued well-being. Structured follow-up care, community support groups, vocational rehabilitation services, and ongoing therapy can provide the continuity needed to navigate the complexities of life after a brain injury.
Individuals who have undergone rehab for brain damage often report improvements in function but also express anxiety about relapse, cognitive decline, or emotional instability. These fears are not unfounded; studies show that secondary conditions such as depression, anxiety, and substance use disorders are more prevalent among TBI survivors. Recognizing this risk, many healthcare providers emphasize the importance of regular mental health screenings and proactive interventions. Cognitive-behavioral therapy, peer mentoring, and mindfulness-based stress reduction have all demonstrated efficacy in helping individuals sustain gains and build emotional resilience. These strategies also help reduce the isolation and identity disruption that often accompany the aftermath of significant neurological trauma.
The road to recovery may also be shaped by socioeconomic factors, including access to healthcare, family support, and employment opportunities. Rehab on skull fracture to heal not just the physical structure but the full person must therefore consider these broader determinants of health. Some individuals may require workplace accommodations, educational adjustments, or legal advocacy to protect their rights and ensure fair treatment. Social workers and patient navigators can play a crucial role in helping individuals and families access these resources, thereby extending the reach and impact of rehabilitation far beyond the clinical setting.
Ultimately, brain trauma rehabilitation is not a one-time intervention but a lifelong journey. Success depends not only on the quality of early care but also on the availability of sustained support. Families, caregivers, and communities must remain engaged, informed, and empathetic, offering encouragement without overstepping boundaries. Health systems, too, must rise to the challenge of integrating physical and mental health services to address the full spectrum of recovery. As our understanding of the brain continues to evolve, so too must our commitment to the individuals whose lives have been altered by injury. Only through comprehensive, compassionate, and long-term care can we fully honor the resilience and potential of those rebuilding their lives after brain trauma.
Frequently Asked Questions (FAQ) About Brain Trauma Rehabilitation
1. What are some lesser-known therapies used in brain trauma rehabilitation?
In addition to conventional approaches, several lesser-known therapies are gaining traction in brain trauma rehabilitation. For example, equine-assisted therapy has been shown to improve balance, motor skills, and emotional regulation by encouraging non-verbal interaction and sensory integration. Another promising option is hyperbaric oxygen therapy (HBOT), which uses pressurized oxygen chambers to enhance brain repair and reduce inflammation. These adjunctive treatments, when used in conjunction with standard rehab for brain damage, offer patients additional avenues for improvement that aren’t always available in traditional clinical settings. Furthermore, emerging technologies such as brain-computer interfaces (BCIs) and transcranial magnetic stimulation (TMS), are being explored to promote neuroplasticity and support long-term recovery.
2. How can family members best support a loved one undergoing rehab for brain damage?
Family involvement is vital during rehab for brain damage, but support goes far beyond physical caregiving. Loved ones can play an important role by participating in therapy sessions, learning communication strategies, and creating a structured, low-stress home environment that fosters healing. Emotional support is equally critical, as patients often struggle with identity shifts and frustration due to slow progress. Encouraging autonomy and celebrating small victories helps sustain motivation. Moreover, family counseling can ease tension and offer coping tools, especially in long-term brain trauma rehabilitation where caregivers also face burnout. Staying involved, informed, and empathetic creates a safety net that benefits both the patient and the family.
3. Can diet and nutrition impact outcomes in brain trauma rehabilitation?
Yes, dietary support is an often overlooked component of effective brain trauma rehabilitation. Nutritional therapy can reduce inflammation, improve cognitive clarity, and support cellular repair. Nutrients like omega-3 fatty acids, antioxidants, B vitamins, and magnesium play key roles in neuroregeneration. For patients undergoing rehab on skull fracture to heal, adequate calcium and vitamin D levels also become crucial for bone repair. Integrating a brain-healthy diet into recovery plans can enhance focus, stabilize mood, and even reduce the need for certain medications. Consulting with a registered dietitian trained in neuro-nutrition can be a valuable addition to multidisciplinary care.
4. What are some signs that rehab for brain damage is plateauing, and what can be done?
Progress in rehab for brain damage often follows a non-linear path, but prolonged stagnation may signal a plateau. Signs include a lack of measurable improvements in memory, coordination, speech, or mood over several weeks. When this occurs, re-evaluation by the rehab team is essential. They may revise the treatment plan, add new modalities, or rotate therapists to spark engagement. For individuals recovering from a skull fracture, ensuring that physical healing is complete is crucial before pushing cognitive rehab further. Innovations like gamified therapy tools, new assistive technologies, or switching to community-based programs can reinvigorate progress during long-term brain trauma rehabilitation.
5. How do patients cope with identity changes during brain trauma rehabilitation?
A profound psychological aspect of brain trauma rehabilitation is the reconstruction of identity. Many patients no longer feel like the person they once were, which can lead to grief, withdrawal, or existential questioning. This emotional shift is often intensified when undergoing rehab on skull fracture to heal, as visible injuries can reinforce internal disorientation. Therapeutic journaling, narrative therapy, and participation in peer support groups help patients make sense of their evolving self-concept. Additionally, counselors often incorporate meaning-making exercises to help patients rediscover purpose post-injury. Recognizing that identity can evolve—rather than be lost—can help restore confidence and emotional well-being.
6. Are virtual rehab platforms effective for people in remote areas or with mobility limitations?
Virtual rehab platforms have significantly expanded access to brain trauma rehabilitation, particularly for individuals in rural or underserved regions. These digital tools provide interactive cognitive exercises, teletherapy sessions, and video consultations with multidisciplinary providers. While not a complete substitute for in-person therapy, they allow patients to continue rehab for brain damage without interruption. Some platforms offer specialized modules for individuals recovering from skull fractures, focusing on gentle exercises and cognitive retraining. However, for optimal results, virtual rehab should be integrated into a broader care plan, ideally supervised by professionals who can adjust therapy intensity and goals as recovery progresses.
7. What role do sleep and circadian rhythms play in brain trauma recovery?
Sleep quality has a direct impact on the success of rehab for brain damage. After a brain injury, circadian rhythms are often disrupted, leading to insomnia or fragmented sleep—both of which impair cognitive recovery. Sleep is when the brain clears waste, consolidates memories, and restores neurotransmitter balance, all of which are vital for rehabilitation. For patients undergoing rehab on skull fracture to heal, good sleep hygiene can also support bone healing and reduce inflammation. Behavioral sleep interventions, light therapy, and melatonin supplementation are among the tools that can be used to restore healthy sleep cycles and enhance the overall effectiveness of brain trauma rehabilitation.
8. How do social reintegration programs contribute to successful long-term rehabilitation?
Social reintegration is a critical yet often neglected phase of brain trauma rehabilitation. After intensive therapy, patients may still struggle with returning to work, managing social interactions, or participating in community activities. Structured reintegration programs provide support with job coaching, adaptive skill training, and social cognition therapy. These programs are especially valuable after rehab on skull fracture to heal, as individuals may face stigma or altered self-image. Social reintegration helps reduce isolation and depression, two major barriers to long-term success in rehab for brain damage. It also fosters independence and promotes community resilience by including families and employers in the recovery process.
9. What advancements are shaping the future of brain trauma rehabilitation?
Emerging technologies are transforming the landscape of brain trauma rehabilitation. Wearable sensors, artificial intelligence, and machine learning now enable more precise tracking of motor and cognitive functions in real time. In rehab for brain damage, these tools can personalize therapy based on real-world data and user feedback. For patients in rehab on skull fracture to heal, 3D imaging is being used to monitor bone regrowth and guide safer rehabilitation. Virtual and augmented reality are also gaining popularity for creating immersive environments that challenge and train specific brain functions. As these innovations evolve, they promise more customized, efficient, and engaging rehabilitation experiences.
10. How does financial stress affect the brain trauma recovery process?
Financial concerns can significantly complicate brain trauma rehabilitation. The cost of therapies, assistive devices, medications, and missed work can place immense pressure on both patients and their families. This stress often triggers anxiety and depression, which in turn hinder cognitive and emotional recovery. During rehab for brain damage, untreated financial distress may also result in the early termination of care or avoidance of necessary treatments. For those requiring rehab on skull fracture to heal, hospital stays and surgical expenses add to the burden. Case managers and medical social workers can help families navigate insurance, apply for grants, and connect with nonprofit support programs, reducing barriers to comprehensive, long-term recovery.
Conclusion: Why Comprehensive Brain Trauma Rehabilitation Matters for Whole-Person Healing
The journey through brain trauma rehabilitation is far more than a medical process—it is a profound act of restoration, resilience, and rediscovery. Individuals who face the daunting challenge of recovering from traumatic brain injuries or skull fractures must contend with changes that extend beyond their physiology. These injuries can shake a person’s sense of identity, challenge their independence, and threaten their emotional equilibrium. In this context, rehab for brain damage becomes a lifeline—a structured yet flexible pathway that helps individuals not only reclaim lost abilities but also build new foundations for mental and emotional health. Through evidence-based interventions, the rehabilitation process empowers patients to take an active role in their recovery, transforming adversity into a catalyst for growth.
Similarly, when patients require rehab on skull fracture to heal properly, the stakes are high. Bone healing must be managed delicately to avoid complications, while underlying brain damage requires targeted therapies to restore cognitive and emotional functions. This dual focus demands a nuanced approach that acknowledges the interplay between structural healing and neuropsychological recovery. When done right, this integrated care model offers more than functional improvement—it offers hope. Patients begin to see themselves not just as survivors but as evolving individuals who can thrive in new and meaningful ways. This is the true promise of modern brain trauma rehabilitation: a commitment to whole-person healing that encompasses body, mind, and spirit.
Brain trauma rehabilitation does not end with discharge from a clinic or the completion of a therapy session. It continues in everyday choices, in the communities that surround the individual, and in the systems that support long-term well-being. The need for sustained mental health care, social reintegration, and personalized rehabilitation plans cannot be overstated. As we advance in our scientific understanding and therapeutic capabilities, we must also deepen our empathy and dedication to those navigating this complex path. By embracing comprehensive, compassionate, and evidence-based rehab for brain damage and skull fractures, we not only improve outcomes—we restore lives. In doing so, we fulfill the highest goal of healthcare: to heal not just what is broken but to nurture what makes us whole.
Further Reading:
Rehabilitation After Traumatic Brain Injury


