Understanding the Importance of Timely Brain Injury Assessment
In the aftermath of any physical trauma involving the head, timely evaluation is critical. Brain injuries can range from mild concussions to severe traumatic brain injuries (TBIs), and the potential consequences often extend far beyond the initial impact. Whether a person slips and hits their head or experiences a high-velocity sports collision, what may seem minor at first can develop into serious neurological complications if left unchecked. A comprehensive brain injury assessment can mean the difference between effective treatment and prolonged, possibly permanent, cognitive decline.
Early intervention through a traumatic brain injury test or head injury assessment is not just a medical formality; it is a cornerstone of neuroprotective care. Medical research continues to confirm that even seemingly mild concussions can lead to long-term impairments in memory, attention, and mood if not properly managed. In many cases, symptoms may not present immediately, which is why prompt evaluation is so essential. The sooner a head trauma assessment is completed, the better the chances are for mitigating risks and initiating early treatment strategies that safeguard long-term mental health.
You may also like: Boost Brain Power Naturally: Evidence-Based Cognitive Training Activities and Memory Exercises That Support Long-Term Mental Health

What Happens During a Brain Injury Assessment?
When a medical professional conducts a brain injury assessment, the process involves multiple layers of examination and testing. The initial phase usually begins with a detailed medical history, including any previous head injuries, neurological conditions, and medication use. Following this, a physical and neurological exam is conducted to evaluate sensory responses, motor skills, reflexes, and cognitive function. These indicators help determine whether a more specialized test—such as a CT scan or MRI—is warranted to assess internal damage.
Cognitive evaluations are an equally crucial component of a thorough traumatic brain injury test. Patients may be asked to perform memory tasks, problem-solving exercises, and orientation checks. These assessments help quantify the extent of cognitive impairment and guide treatment decisions. A brain trauma test, when interpreted in conjunction with neuroimaging and clinical history, allows clinicians to make informed decisions about the need for additional interventions such as rehabilitation, medication, or even head trauma surgery in more serious cases.
In emergency settings, the assessment also includes ruling out life-threatening conditions like hematomas, skull fractures, or elevated intracranial pressure. This is where urgent head injury surgery may come into play, particularly when scans reveal bleeding or swelling that requires immediate surgical relief. The thoroughness and precision of the brain injury assessment process underscore its vital role in preserving not just life but also quality of life over the long term.
Signs That You May Need a Traumatic Brain Injury Test
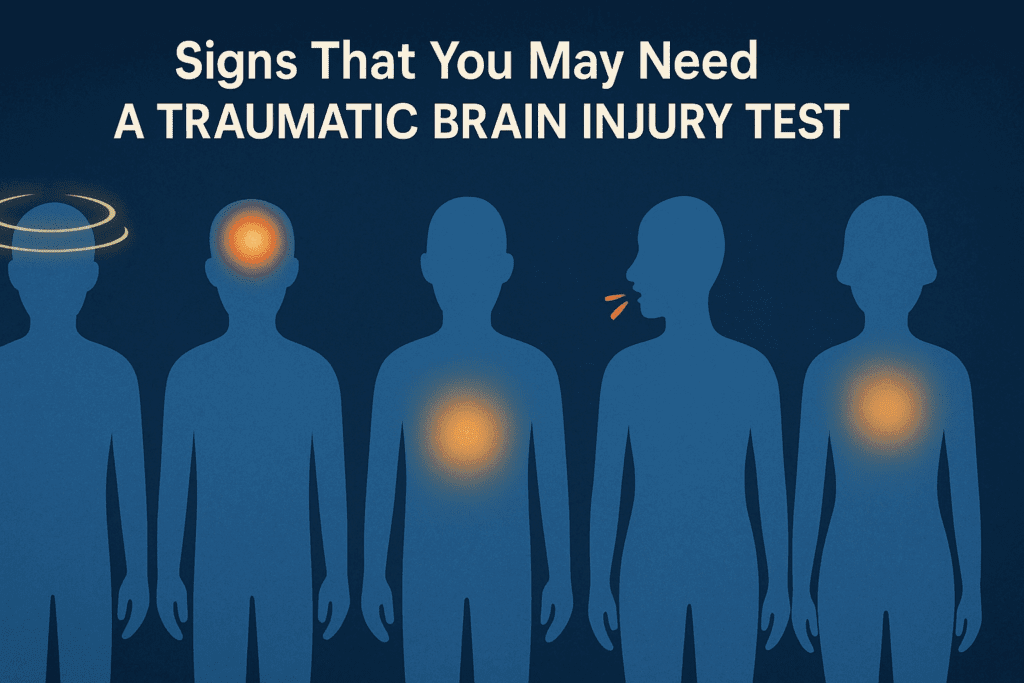
Many people mistakenly assume that if they are not knocked unconscious or visibly bleeding, a head injury is not serious. However, some of the most dangerous brain injuries are those that appear subtle at first. Warning signs can include persistent headaches, difficulty concentrating, dizziness, nausea, light sensitivity, irritability, and changes in sleep patterns. In more severe cases, symptoms such as slurred speech, repeated vomiting, confusion, or seizures may emerge.
Because these symptoms can evolve gradually, it’s crucial to consider a TBI assessment even if the initial incident seemed minor. Athletes, for instance, are often at risk for repetitive head injuries that cumulatively cause serious damage, even if each event seemed inconsequential. Likewise, older adults are especially vulnerable due to brain atrophy and a higher risk of falls. A comprehensive head injury assessment ensures that these risks are evaluated and addressed before they escalate.
When symptoms persist for more than a few days or worsen over time, it is imperative to seek a brain damage test. Neuropsychological testing may be used in these cases to evaluate memory, reasoning, language, and other cognitive functions. When performed early, such assessments not only inform treatment but can also serve as a baseline for monitoring recovery over time, particularly in cases where brain injury rehabilitation is required.
The Role of Imaging in Head Trauma Evaluation
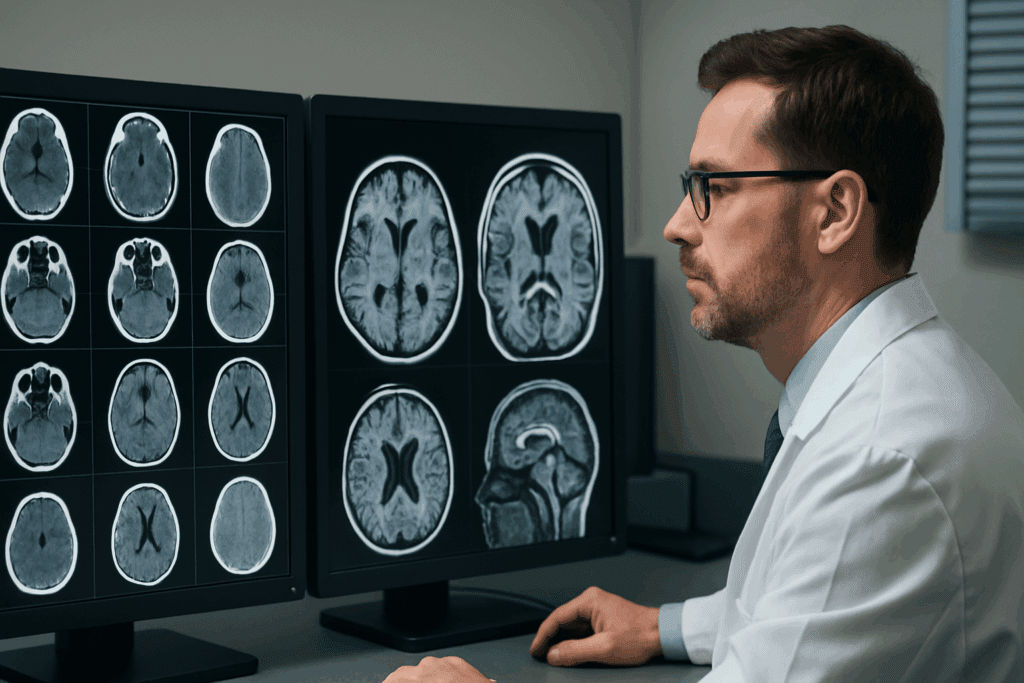
Neuroimaging plays a pivotal role in identifying structural brain injuries that may not be apparent through physical or cognitive testing alone. CT scans are commonly used in emergencies to detect bleeding, fractures, or swelling. These scans provide a quick, clear picture of potential intracranial damage that might necessitate immediate head trauma surgery or other interventions.
MRIs, while less frequently used in emergency contexts, offer more detailed information about soft tissue damage and can be crucial in diagnosing lingering symptoms that do not resolve over time. This makes MRI a valuable tool in the later stages of a head injury assessment, especially when determining the extent of diffuse axonal injury—a common and serious result of rapid acceleration or deceleration of the brain.
It is important to understand that a brain trauma test often involves a combination of these imaging techniques alongside clinical observation. Imaging results must be interpreted in the context of the patient’s symptoms, history, and neurological exam. For instance, a normal CT scan does not rule out a concussion or mild TBI, which may still require medical management and follow-up care.

How Head Injuries Impact Long-Term Mental Health
Beyond the immediate symptoms, brain injuries can have profound and lasting effects on emotional and psychological well-being. Studies have shown that individuals who have experienced a TBI are at increased risk for depression, anxiety disorders, PTSD, and even personality changes. These issues often stem from both the physical damage to brain structures and the emotional toll of coping with cognitive impairment.
The link between head trauma and long-term mental health challenges underscores the necessity of early and thorough evaluation. A comprehensive head injury assessment provides the foundation for monitoring and managing not only physical but also emotional recovery. Mental health professionals may become integral parts of the treatment team, especially when symptoms persist or worsen after the initial injury.
One of the more insidious aspects of brain injury is the delayed onset of certain psychiatric symptoms. These may include mood swings, irritability, reduced frustration tolerance, and social withdrawal. These symptoms can easily be mistaken for unrelated mental health conditions unless there is a clear understanding of the injury’s history and progression. This highlights why a timely traumatic brain injury test can be critical for accurate diagnosis and comprehensive care.
When Head Trauma Requires Surgical Intervention
While many brain injuries can be managed with observation and rehabilitation, there are situations in which surgery becomes necessary. A head injury operation may be performed to relieve intracranial pressure, remove blood clots (hematomas), or repair skull fractures. These procedures are typically reserved for cases in which imaging shows clear structural damage or when neurological deterioration is rapid and life-threatening.
Understanding when to opt for head injury surgery requires a careful balance between clinical urgency and potential surgical risks. Neurosurgeons consider a variety of factors, including the size and location of any hemorrhage, the patient’s neurological status, and the overall health of the individual. In some cases, patients may undergo a procedure known as a craniotomy, where a portion of the skull is temporarily removed to allow the brain to swell without causing further injury.
Head trauma surgery is a serious undertaking and is usually followed by a prolonged period of recovery and rehabilitation. Postoperative care often involves collaboration among neurologists, physical therapists, occupational therapists, and mental health providers. This interdisciplinary approach ensures that both the physical and cognitive aspects of recovery are addressed holistically.
Pediatric and Geriatric Considerations in Brain Injury Assessment
Children and older adults represent two demographics with unique vulnerabilities when it comes to head trauma. In pediatric populations, brain development is still underway, meaning that even mild injuries can disrupt critical stages of cognitive and emotional maturation. A prompt and thorough brain injury assessment is essential to prevent developmental delays and learning disabilities that may result from undiagnosed injuries.
Children may not always be able to articulate their symptoms clearly, making it vital for caregivers and medical providers to be vigilant for subtle changes in behavior, attention span, or emotional regulation. Pediatricians often work alongside neurologists and developmental specialists to tailor the traumatic brain injury test process for younger patients, ensuring both accuracy and emotional sensitivity.
In geriatric populations, factors such as reduced brain volume, existing cognitive decline, and increased susceptibility to falls amplify the risk of complications following head trauma. A tbi assessment in older adults must take into account comorbid conditions such as dementia, stroke history, or cardiovascular disease. Additionally, older individuals may require longer recovery times and more intensive rehabilitation protocols, making early detection and intervention even more crucial.
Rehabilitation After a Brain Injury: What to Expect
Rehabilitation is a vital component of recovery for individuals who have sustained a significant brain injury. Following a thorough brain injury assessment, a multidisciplinary team will often develop a personalized rehabilitation plan designed to restore function and enhance quality of life. This plan may include physical therapy to improve motor function, occupational therapy to aid with daily tasks, and cognitive therapy to address deficits in memory, attention, or executive function.
Mental health support is also essential, particularly for those experiencing anxiety, depression, or adjustment disorders in the wake of a head injury. Counseling or psychiatric care can help individuals and their families navigate the emotional landscape of recovery. In many cases, support groups and community resources play a valuable role in reducing isolation and promoting social reintegration.
Continual evaluation is key throughout the rehabilitation process. Follow-up appointments often involve repeat brain trauma tests to monitor progress and adjust treatment as necessary. By comparing new results with initial assessments, healthcare providers can refine their approach, ensuring that each stage of recovery is guided by objective data and clinical expertise.
Frequently Asked Questions: Brain Injury Assessment and Long-Term Mental Health
1. What are the long-term mental health risks of not getting a timely head trauma assessment?
Failing to undergo a prompt head trauma assessment can leave subtle brain injuries undetected, which often worsen over time. When the initial impact isn’t fully evaluated, microbleeds, diffuse axonal injuries, or mild swelling may be overlooked—conditions that can slowly erode cognitive function. Over months or years, individuals who never received a proper brain injury assessment may develop chronic issues like irritability, emotional dysregulation, or memory impairment that interfere with daily life. There’s also an elevated risk of developing mood disorders, including depression and anxiety, which are linked to untreated neural trauma. A thorough TBI assessment early on not only helps identify visible injuries but also guides ongoing mental health monitoring that could mitigate or prevent psychological consequences down the line.
2. Can a brain trauma test help differentiate between physical and psychological symptoms?
Yes, a brain trauma test plays a key role in distinguishing between symptoms directly resulting from neurological damage and those stemming from psychological stress or trauma. Head injuries often lead to overlapping symptoms like fatigue, confusion, or emotional volatility, which can easily be misattributed. By combining cognitive evaluations with imaging during a brain injury assessment, clinicians can parse out whether these experiences are due to organic brain changes or reactive emotional distress. This clarity is particularly valuable in deciding whether to prioritize medication, psychotherapy, cognitive rehab, or a multidisciplinary approach. Without a head injury assessment to establish a baseline, treatment may focus too narrowly on psychiatric symptoms while overlooking underlying structural or functional brain changes.
3. How can head injury surgery impact future cognitive performance?
Head injury surgery, while often life-saving, can affect long-term brain function in both positive and challenging ways. On the one hand, surgical interventions like hematoma evacuation or craniotomy can relieve pressure that, if left untreated, might cause permanent damage. On the other hand, recovery from head trauma surgery may involve a prolonged period of cognitive rehabilitation, especially if regions associated with memory or executive function are involved. The outcome largely depends on the timing and precision of the surgical approach, along with the patient’s baseline health and access to post-operative therapy. A complete TBI assessment before and after the procedure can help track recovery and customize interventions that optimize long-term cognitive outcomes.
4. Is a head injury operation always necessary for severe trauma?
Not always. While a head injury operation may be required in cases involving skull fractures, hemorrhage, or increased intracranial pressure, many severe TBIs can still be managed conservatively. A detailed brain injury assessment, including both imaging and neurological exams, helps determine whether surgery is the safest and most effective path. Emerging technologies such as dynamic brain monitoring and advanced MRIs are improving clinicians’ ability to assess risk and delay or avoid unnecessary head injury surgery. Additionally, in some patients, a period of intensive monitoring in a neurocritical care unit can replace immediate surgical intervention, depending on how stable the patient remains. It’s not just the injury’s severity that dictates the decision but how the brain responds over time—which a thorough head trauma assessment helps clarify.
5. What role does a brain damage test play in post-concussion syndrome diagnosis?
Post-concussion syndrome (PCS) presents a diagnostic challenge due to its blend of cognitive, emotional, and physical symptoms that can persist for weeks or months. A brain damage test is vital in ruling out structural abnormalities while also helping to identify functional disruptions that may not show up on basic scans. In PCS, patients might have normal CT or MRI findings yet still suffer from concentration issues, light sensitivity, or irritability. A TBI assessment tailored for PCS often includes neuropsychological testing, balance evaluations, and symptom tracking tools that offer a more nuanced understanding of brain function. These insights help healthcare providers develop individualized recovery plans and may inform decisions about returning to work, school, or sports.
6. Are there non-invasive alternatives to a traumatic brain injury test in children?
Yes, children often benefit from non-invasive diagnostic tools designed to minimize discomfort and radiation exposure during a traumatic brain injury test. In pediatric settings, clinicians may use advanced ultrasound techniques, eye-tracking technology, or vestibular assessments to detect signs of brain dysfunction. Pediatric brain injury assessment protocols also incorporate observational scales that evaluate behavioral and cognitive responses in age-appropriate ways. While MRI and CT scans remain essential in more severe cases, the trend is toward minimizing imaging unless necessary, particularly for mild TBIs. These alternatives still fulfill the clinical role of a standard head trauma assessment while ensuring safety and emotional comfort for younger patients.
7. How do socioeconomic factors affect access to a head injury assessment?
Access to a timely head injury assessment is often influenced by socioeconomic disparities that affect healthcare quality, insurance coverage, and proximity to medical specialists. Individuals in rural or underserved areas may not have access to neuroimaging or trained neurologists, delaying crucial steps in brain injury assessment. Moreover, financial concerns may deter some people from seeking a brain trauma test even when symptoms warrant evaluation. Community health initiatives and mobile TBI clinics are beginning to bridge this gap, offering screenings and assessments in schools, athletic facilities, and community centers. Addressing these disparities is vital to ensure that everyone has equal access to a proper head trauma assessment, especially when early intervention could prevent irreversible damage.
8. Can a TBI assessment predict the need for future head trauma surgery?
While a TBI assessment doesn’t definitively predict whether someone will need head trauma surgery, it does establish critical baselines that inform future decisions. For instance, identifying areas of vulnerability, such as mild swelling or microvascular damage, helps medical teams monitor progression more closely. Repeated head injury assessments over time can reveal trends—such as increasing intracranial pressure or declining cognition—that may warrant surgical intervention down the line. Moreover, AI-enhanced imaging and machine learning algorithms are being developed to improve predictive accuracy during brain trauma tests. These tools may one day make it possible to forecast complications earlier and tailor interventions more proactively, shifting the paradigm from reactive to preventive neurosurgery.
9. How is a head injury assessment tailored for athletes and high-risk professionals?
For athletes, military personnel, and other high-risk individuals, a head injury assessment often includes baseline cognitive testing conducted pre-season or pre-deployment. This allows for quicker, more accurate comparisons after any suspected trauma. Advanced traumatic brain injury test protocols for these groups may include impact sensor data, balance tracking, and visual-motor coordination tasks. Unlike general assessments, these are often repeated regularly—even in the absence of symptoms—to catch subtler signs of injury that might accumulate over time. Because return-to-play or return-to-duty decisions carry high stakes, specialized TBI assessments offer a more nuanced, personalized picture of brain resilience and recovery capacity, often preventing premature re-exposure to danger.
10. What innovations are shaping the future of brain injury assessment and treatment?
The field of brain injury assessment is undergoing rapid evolution thanks to wearable technology, portable neuroimaging devices, and biomarkers detectable in blood and saliva. These innovations are making it easier to perform a reliable traumatic brain injury test even outside of hospital settings, such as on sports fields or in combat zones. Researchers are exploring neuroinflammatory markers that could provide real-time data about brain health, making the brain damage test of the future faster and more precise. In surgical settings, augmented reality tools and robotic-assisted head injury operations are improving surgical outcomes and minimizing collateral damage. As AI continues to integrate with diagnostic platforms, the future of head injury assessment will likely involve faster triage, more personalized interventions, and earlier detection of subtle cognitive shifts, ultimately reducing the long-term burden of head trauma.
Conclusion: Why Early Head Injury Evaluation Matters for Lifelong Brain Health
When it comes to brain health, time is of the essence. The earlier a brain injury assessment is conducted following head trauma, the greater the chance of preventing long-term cognitive, emotional, and physical complications. Whether through a routine traumatic brain injury test, advanced imaging, or comprehensive neuropsychological evaluation, early diagnosis sets the stage for effective treatment and meaningful recovery.
Incorporating a TBI assessment into standard care after any suspected head trauma helps ensure that no signs of brain damage are overlooked. It allows clinicians to tailor treatments that may prevent the need for more invasive measures, such as head trauma surgery or emergency head injury operation, later down the line. The role of a brain damage test in this process cannot be overstated; it offers vital information that protects not only immediate health but also the brain’s resilience over a lifetime.
Given the potential for delayed symptom onset and the profound impact head injuries can have on mental health, a proactive approach is essential. Every person, whether an athlete, accident survivor, or aging adult, deserves timely access to a thorough brain injury assessment. By prioritizing early evaluation and intervention, we take an essential step toward preserving lifelong cognitive well-being and mental clarity.
Further Reading:
Diagnosis and Assessment of Traumatic Brain Injury
Evaluation of traumatic brain injury, acute
How do healthcare providers diagnose traumatic brain injury (TBI)?


