Living with lower back pain can be a daily challenge, especially when it’s caused by a bulging disc. This condition, which involves the displacement of spinal disc material beyond its normal boundary, can put pressure on nearby nerves, leading to inflammation, pain, and reduced mobility. Often diagnosed as part of a broader category known as discogenic back pain, this issue affects millions of adults worldwide, particularly those engaged in physically demanding occupations or those who maintain sedentary lifestyles. Fortunately, discogenic back pain physical therapy exercises can offer meaningful relief by promoting spinal stability, improving flexibility, and reducing nerve compression. This article explores the most effective exercises for lower back pain caused by a bulging disc, guided by clinical insight and grounded in medically sound rehabilitation practices.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
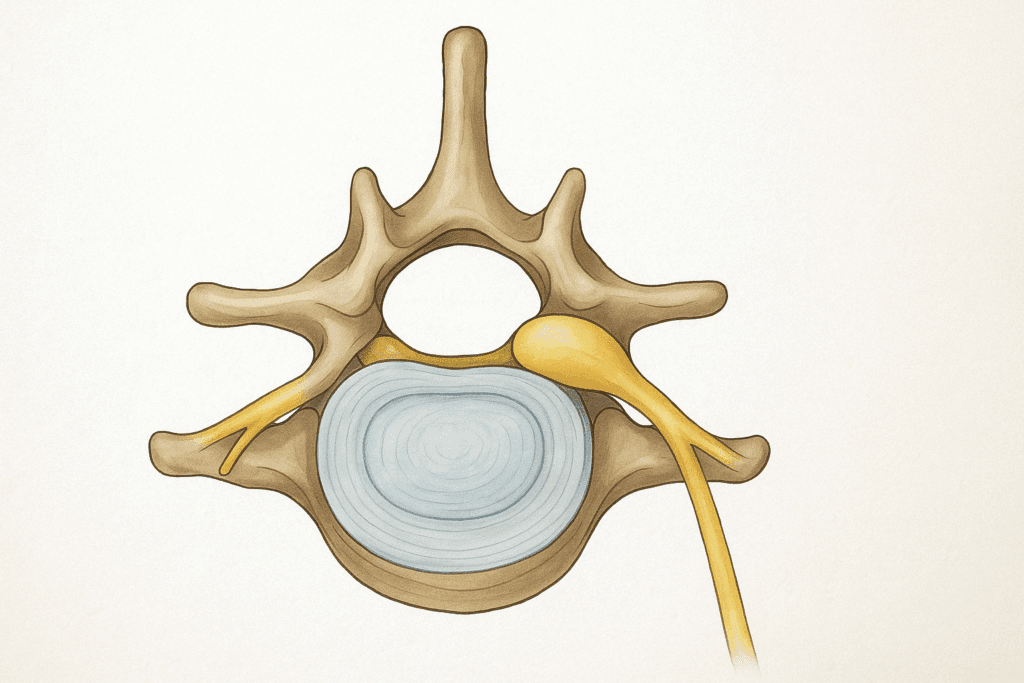
Understanding Discogenic Back Pain and Bulging Discs
To appreciate the role of exercise in managing this condition, it’s important to understand the mechanics behind a bulging disc. Each intervertebral disc functions as a cushion between vertebrae, composed of a tough outer shell called the annulus fibrosus and a gel-like center known as the nucleus pulposus. Over time, repetitive stress, poor posture, or acute injury can weaken the outer layer, causing the nucleus to protrude outward without completely rupturing. This bulging disc may impinge on nearby nerves, especially the sciatic nerve, triggering sharp, radiating pain that extends into the buttocks or legs.
Discogenic pain refers specifically to discomfort originating from the disc itself, not just the surrounding structures. It’s often confirmed through clinical tests and imaging such as MRI. Symptoms may include deep, aching pain in the lower back, aggravated by sitting, bending, or lifting. Physical therapy aims to reduce these symptoms by correcting posture, strengthening spinal muscles, and relieving mechanical stress on the affected disc. Targeted, progressive exercise is central to this goal.
The Impact of Lifestyle on Discogenic Pain Recovery
The importance of lifestyle in shaping recovery outcomes from a bulging disc cannot be overstated. Sedentary behaviors, poor diet, stress, and insufficient sleep all contribute to systemic inflammation and slow healing. These factors can also compromise the effectiveness of even the best discogenic back pain physical therapy exercises. For example, a person who diligently performs rehabilitation exercises but spends the rest of the day slouched at a desk or carrying excess abdominal weight may experience limited progress.
One key lifestyle adjustment is optimizing body weight. Excess weight, particularly around the abdomen, increases axial loading on the spine and alters lumbar curvature. This mechanical stress exacerbates the pressure on bulging discs and impairs the body’s ability to maintain a neutral posture. Nutritional strategies that emphasize anti-inflammatory foods—such as leafy greens, fatty fish, nuts, berries, and turmeric—can support tissue repair and reduce systemic pain sensitivity. Simultaneously, reducing processed sugars and refined carbohydrates helps mitigate insulin resistance, which is often linked to chronic inflammation.
Sleep hygiene is another overlooked factor. Deep sleep stages are critical for musculoskeletal recovery. Pain sufferers often experience sleep disruption, which can create a vicious cycle of fatigue, heightened pain perception, and impaired healing. Techniques such as sleep scheduling, minimizing blue light exposure in the evening, and practicing relaxation techniques can dramatically improve sleep quality and enhance the body’s regenerative capacity.
The Role of Manual Therapy and Soft Tissue Techniques
While exercises for lower back pain bulging disc recovery are fundamental, adjunctive manual therapies can provide important support in the rehabilitation process. Techniques such as myofascial release, trigger point therapy, and spinal mobilization are frequently employed by physical therapists, chiropractors, and massage therapists to reduce muscle tension, enhance circulation, and facilitate neuromuscular reeducation.
Myofascial release focuses on alleviating restrictions in the fascia—the connective tissue that surrounds muscles and organs. In patients with discogenic pain, fascial tightness often develops in compensatory patterns, leading to referred pain and functional limitations. By releasing these adhesions, therapists can reduce aberrant stress on the spine and increase the efficacy of corrective exercises.
Spinal mobilization and low-grade manipulation may help restore segmental movement and decrease protective muscle guarding. While these techniques should be used cautiously in individuals with acute disc herniation, research supports their safety and effectiveness when applied by trained professionals. Manual therapy can also improve patient compliance by reducing pain and increasing comfort during exercise sessions.
Why Exercise Matters for Bulging Disc Recovery
The rationale for using exercise in the treatment of discogenic pain lies in biomechanics and physiology. A well-structured program of discogenic back pain physical therapy exercises can restore proper alignment of the lumbar spine, improve muscular coordination, and prevent recurrence. It can also improve circulation to the affected area, enhancing the body’s natural healing response. Inactive recovery or prolonged bed rest, on the other hand, often leads to stiffness, muscle atrophy, and worsening of symptoms.
Several studies support the efficacy of physical therapy in reducing symptoms of lumbar disc herniation and bulging discs. In particular, McKenzie-based therapy, core stabilization training, and directional preference exercises have demonstrated positive outcomes in randomized clinical trials. The overarching goal is not merely to mask symptoms but to address the biomechanical root causes of the pain, which often stem from muscular imbalances or impaired movement patterns. This makes exercise a critical element in both acute management and long-term prevention.
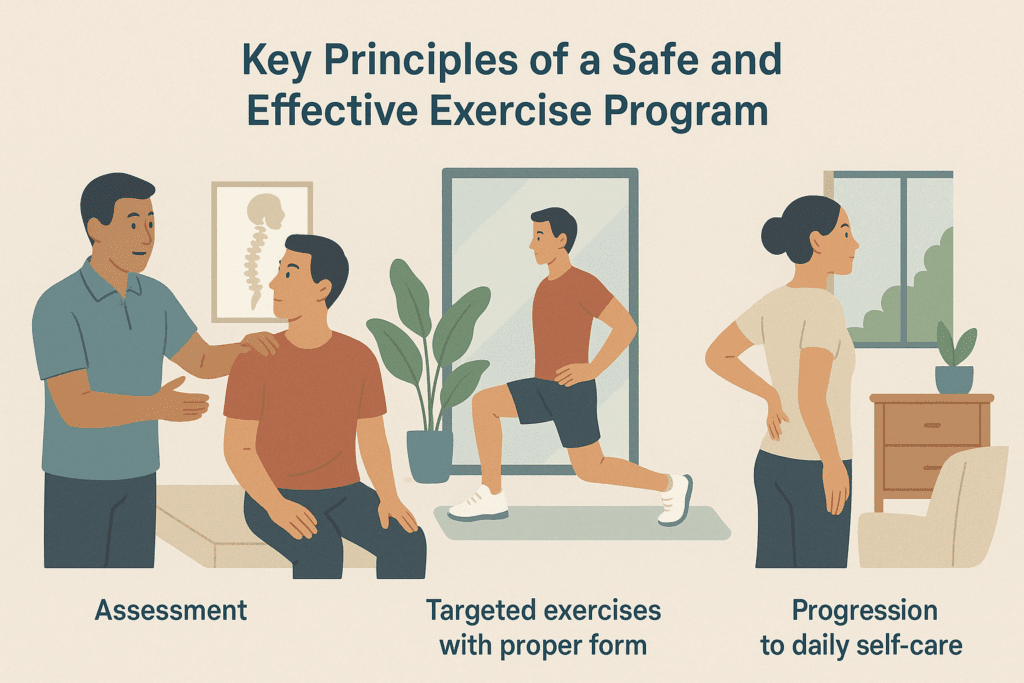
Key Principles of a Safe and Effective Exercise Program
Before engaging in exercises for lower back pain bulging disc rehabilitation, it is essential to consider several foundational principles. First and foremost, not all exercises are appropriate for every individual. A physical therapy plan should be tailored based on the severity and nature of the disc injury, the patient’s physical condition, and the presence of any comorbid conditions such as spinal stenosis or spondylolisthesis. A qualified physical therapist can help determine the right starting point and progression strategy.
Second, proper form is paramount. Incorrect execution of even a seemingly simple movement can exacerbate disc compression and increase pain. This is particularly true for exercises that involve spinal flexion or rotation. For patients with posterior disc bulges, forward bending may worsen symptoms, while extension-based movements may offer relief. Therefore, learning to perform exercises mindfully, often under the supervision of a rehabilitation professional, can make the difference between improvement and setback.
Finally, consistency is key. A single session of physical therapy is unlikely to produce lasting results. Sustained commitment, gradual progression, and ongoing assessment are all part of a successful rehabilitation journey. Patients should be encouraged to view exercise as a lifelong strategy for spine health, not a temporary fix.

Extension-Based Exercises for Lumbar Decompression
One of the most commonly prescribed approaches for discogenic pain from a bulging disc is the McKenzie Method, which emphasizes spinal extension. These exercises aim to centralize pain—that is, to reduce leg or buttock symptoms by redirecting discomfort toward the center of the back, an indicator of healing.
A classic example is the prone press-up. In this exercise, the patient lies face down and slowly presses the upper body upward using the arms, while keeping the hips and legs relaxed on the ground. This maneuver promotes lumbar extension and helps to reduce pressure on the anterior portion of the intervertebral disc. When performed regularly, prone press-ups can decrease nerve impingement and encourage disc retraction.
Another effective movement is the standing back extension. Here, the individual stands upright and places both hands on the lower back for support. By gently arching backward, they can create a mild decompression of the posterior disc space. This exercise is especially useful for people who spend long hours seated, as it counteracts the forward flexion associated with prolonged sitting.

Core Stabilization and Deep Muscle Activation
While extension exercises focus on spinal decompression, core stabilization targets the muscles that support the spine and pelvis. These include the transverse abdominis, multifidus, and pelvic floor—muscles that are often weak or underutilized in individuals with chronic lower back pain. Strengthening these muscles improves postural control and reduces the risk of future injury.
One foundational core exercise is abdominal bracing. Performed lying on the back with knees bent, this movement involves contracting the deep abdominal muscles without allowing the pelvis to tilt or the spine to arch. It teaches patients how to engage the core without compensatory movements, building a stable base for more dynamic exercises.
Bird-dog is another core exercise that emphasizes spinal alignment and balance. While on hands and knees, the patient extends one arm and the opposite leg while maintaining a neutral spine. This exercise challenges both coordination and core endurance, and can be modified for beginners or progressed for advanced users. Over time, such exercises help restore muscular balance and reduce reliance on overactive superficial muscles that contribute to pain.
The Psychological Dimension of Chronic Back Pain
Chronic pain is never just physical. Psychological factors—such as fear-avoidance behaviors, depression, anxiety, and catastrophizing—can dramatically influence the perception of pain and the trajectory of recovery. The brain plays an integral role in modulating pain signals, and negative emotional states can amplify neural responses to noxious stimuli, creating a cycle of increased suffering.
Cognitive-behavioral therapy (CBT) is a well-established intervention that helps patients reframe maladaptive thoughts and develop coping strategies. When integrated into a multidisciplinary rehabilitation program, CBT has been shown to improve adherence, reduce pain intensity, and enhance functional outcomes. For patients dealing with persistent back pain from a bulging disc, learning to manage stress and anxiety may be as important as physical treatment.
Mindfulness-based stress reduction (MBSR), which incorporates meditation, body scanning, and gentle yoga, has also shown promise in reducing pain-related distress. By encouraging nonjudgmental awareness of bodily sensations, MBSR helps patients disengage from reactive pain behaviors and reconnect with movement in a safe and supported way.
The Emerging Role of Regenerative Therapies
While exercise remains the foundation of bulging disc management, regenerative medicine is expanding the toolbox of available treatments. Emerging interventions such as platelet-rich plasma (PRP), stem cell injections, and prolotherapy are being explored for their potential to repair disc tissue and reduce inflammation at the source.
PRP therapy involves concentrating a patient’s own platelets and injecting them into the affected area to stimulate healing. Preliminary studies suggest that PRP may help modulate the inflammatory environment and support tissue regeneration, although more large-scale trials are needed to confirm its efficacy.
Stem cell therapies, derived from bone marrow or adipose tissue, offer another frontier. These cells can differentiate into various tissue types and may help replenish damaged disc structures. However, ethical, regulatory, and logistical challenges remain, and such therapies should only be pursued under the guidance of board-certified specialists in a research-supported setting.
Prolotherapy, which involves injecting a mild irritant to stimulate the body’s healing response, has shown promise in select cases of ligamentous laxity and joint instability. Although not directly targeting the disc, this approach may reduce biomechanical stress and complement physical rehabilitation when used appropriately.

Flexibility Training to Reduce Muscular Tension
Tight hamstrings, hip flexors, and lumbar paraspinals often accompany discogenic lower back pain. Stretching these areas can alleviate strain on the lumbar spine and restore healthy movement patterns. However, it is crucial to approach stretching cautiously in the context of a bulging disc, avoiding any movements that place excessive pressure on the lumbar discs.
A safe and effective stretch is the knee-to-chest stretch, performed while lying on the back. By gently pulling one knee toward the chest and holding for several seconds, patients can release tension in the lower back and gluteal region. This stretch should be done slowly and without forcing the movement, especially if symptoms radiate into the leg.
Piriformis stretching also offers significant benefits, as tightness in this deep gluteal muscle can aggravate sciatic nerve symptoms. Lying on the back with one ankle crossed over the opposite knee, the patient pulls the uncrossed leg toward the chest, feeling a stretch in the hip and buttock. Consistent practice improves hip mobility and can reduce compensatory strain on the lower back.
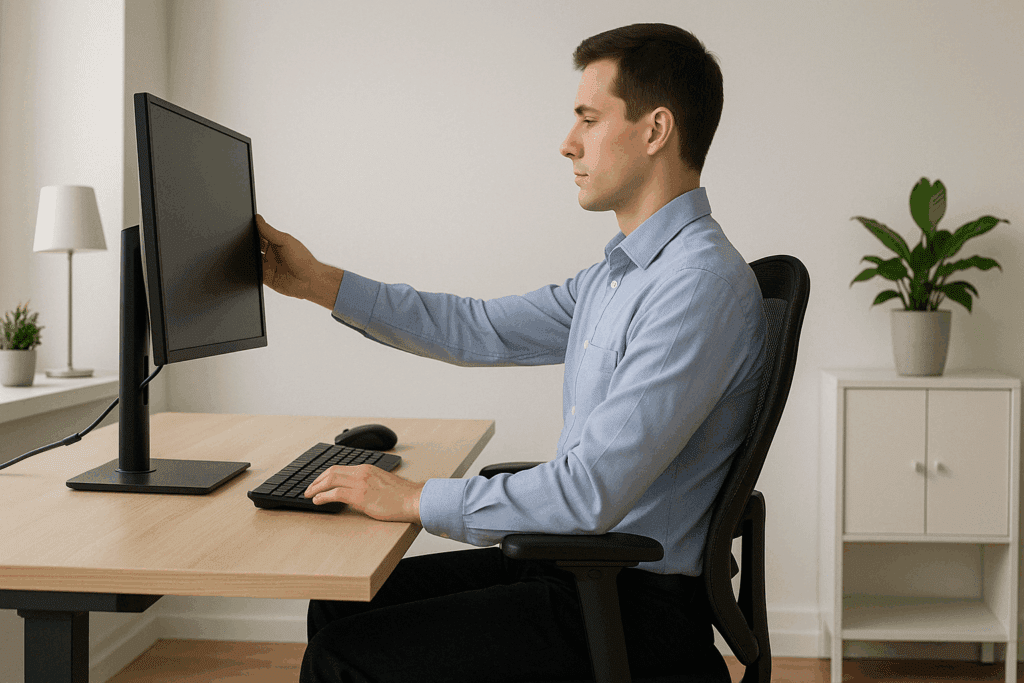
Postural Re-education and Ergonomic Awareness
In addition to therapeutic exercises, improving posture and daily body mechanics plays a vital role in long-term recovery from a bulging disc. Discogenic back pain physical therapy exercises often incorporate elements of postural re-education to help patients become aware of harmful habits and adopt spine-friendly movements.
Neutral spine training is a fundamental concept. It teaches individuals how to align the spine in its natural curves—cervical lordosis, thoracic kyphosis, and lumbar lordosis—during sitting, standing, and moving. Learning to maintain this alignment reduces stress on the intervertebral discs and prevents aggravation of existing injuries.
Ergonomic modifications also support recovery. Patients are advised to use lumbar rolls while sitting, elevate computer monitors to eye level, and avoid prolonged periods in one position. Instruction on safe lifting techniques—such as bending at the hips and knees rather than the waist—can further minimize strain. These interventions work synergistically with physical therapy exercises to reinforce spine health throughout the day.
Progressive Resistance Training for Functional Strength
Once pain has subsided and basic mobility has been restored, many patients benefit from integrating progressive resistance training into their regimen. This step builds muscular strength, enhances stability, and increases resilience against future episodes of lower back pain. The key is to introduce resistance gradually and avoid any exercises that involve spinal compression or excessive flexion.
For example, modified squats using a resistance band or stability ball can strengthen the quadriceps and glutes without loading the spine. Dead bug exercises, performed lying on the back while moving limbs in a controlled fashion, are excellent for dynamic core training. These movements reinforce the neuromuscular patterns established during earlier stages of rehabilitation and transition the patient toward full physical capacity.
Patients should also be encouraged to integrate functional movements that mimic daily activities, such as reaching, twisting, and bending safely. This promotes real-world applicability and ensures that exercise outcomes translate into improved quality of life. With guidance from a skilled physical therapist, resistance training becomes a tool not just for rehabilitation, but for lifelong health maintenance.

Integrating Mind-Body Approaches for Holistic Recovery
Emerging research supports the inclusion of mind-body techniques—such as yoga, tai chi, and breathwork—into physical therapy for discogenic pain. These approaches emphasize awareness, controlled movement, and relaxation, all of which can complement traditional exercises for lower back pain bulging disc recovery.
Yoga poses such as cat-cow, sphinx, and supported bridge can gently mobilize the spine and reduce tension, provided they are performed with attention to spinal alignment. Tai chi, with its slow and deliberate motions, can improve balance and proprioception. Mindful breathing enhances parasympathetic activation, helping to counteract the stress and muscular guarding often associated with chronic pain.
Patients who incorporate these modalities often report improved mood, reduced fear-avoidance behaviors, and greater adherence to their rehabilitation programs. While these methods are not substitutes for physical therapy, they offer a valuable adjunct that enhances the mind-body connection and supports comprehensive recovery.
The Role of Supervision and Patient Education
Effective rehabilitation hinges not only on exercise selection but also on patient education and professional oversight. Individuals recovering from a bulging disc should be thoroughly educated on the nature of their condition, the expected timeline of healing, and the signs that warrant medical reassessment. This knowledge empowers them to make informed decisions and avoid behaviors that may hinder progress.
A physical therapist plays a crucial role in guiding this process. They provide real-time feedback, modify exercises based on patient response, and help navigate setbacks. Regular reassessment ensures that the program remains aligned with the patient’s goals and capabilities. Without professional oversight, there is a risk of performing movements incorrectly, leading to reinjury or delayed recovery.
Equally important is the patient’s willingness to take an active role. Self-management strategies, including daily home exercises, posture correction, and lifestyle modifications, reinforce the benefits of clinical therapy. The therapeutic alliance between patient and provider becomes a key factor in successful outcomes.
A Long-Term Strategy for Spine Health and Function
Recovery from a bulging disc is rarely instantaneous. It requires patience, discipline, and a holistic approach that addresses the underlying mechanical and functional issues. Discogenic back pain physical therapy exercises are not a quick fix but rather part of a broader lifestyle shift aimed at optimizing spinal health and preventing future problems.
Ultimately, patients who embrace exercise as a cornerstone of their wellness strategy experience not only relief from acute symptoms but also enhanced physical confidence, better mobility, and improved overall health. As they regain function and resume daily activities, many report a renewed sense of control over their bodies and their lives. This transformation speaks to the power of movement as medicine.
Preventive Strategies for Long-Term Spine Health
Prevention is the ultimate goal in managing discogenic conditions. Once symptoms subside, patients must adopt proactive strategies to maintain spinal health and reduce the likelihood of recurrence. This involves more than continuing physical therapy exercises; it requires a holistic approach to body awareness, self-care, and lifestyle alignment.
Maintaining a consistent exercise routine that includes core strengthening, flexibility work, and aerobic conditioning is essential. Walking, swimming, and low-impact cycling are excellent cardiovascular choices that support spinal mobility without excessive strain. Regularly checking posture and alignment during daily activities—such as driving, cooking, or gardening—can reinforce spinal awareness.
Footwear also plays a surprising role. Poor arch support or misalignment at the feet can create kinetic chain imbalances that travel upward, affecting the lumbar spine. Investing in proper footwear or orthotic inserts can contribute to overall alignment and reduce compensatory stress.
Staying informed and educated is another cornerstone of prevention. Patients who understand their condition are more likely to adhere to safe movement practices, identify early warning signs, and seek timely intervention when needed. Resources such as physical therapy handouts, online workshops, and patient support groups can foster empowerment and community.
Frequently Asked Questions: Advanced Guidance on Exercises for Lower Back Pain from a Bulging Disc
1. Can discogenic back pain physical therapy exercises reduce the likelihood of future disc injuries?
Yes, when executed correctly and consistently, discogenic back pain physical therapy exercises do more than relieve immediate symptoms—they lay a foundation for long-term spinal resilience. These exercises are designed to strengthen deep stabilizing muscles like the multifidus and transverse abdominis, which support spinal integrity. Over time, a well-conditioned core can help absorb mechanical stresses that would otherwise overload the intervertebral discs. Additionally, improved posture and movement efficiency gained through therapeutic exercise reduces the risk of cumulative disc damage during everyday tasks. It’s important to note that injury prevention also depends on lifestyle factors such as body weight, ergonomics, and flexibility maintenance, all of which should complement your exercise regimen.
2. How should athletes approach exercises for lower back pain bulging disc rehabilitation?
Athletes require a nuanced approach to disc rehabilitation because of the higher loads and dynamic movements involved in their training. For them, exercises for lower back pain bulging disc recovery must begin with deloading and neutral spine awareness before progressing to sport-specific movements. In the early phase, low-impact isometric holds and anti-rotation core exercises like Pallof presses are safer alternatives to traditional lifts. As healing progresses, dynamic stabilization drills and controlled plyometrics can be phased in. A physical therapist familiar with sports performance should supervise return-to-play timelines, ensuring that the athlete doesn’t compromise their spine in pursuit of pre-injury performance levels.
3. Are there any risks associated with performing discogenic back pain physical therapy exercises without professional guidance?
Yes, while many exercises appear simple, the spinal mechanics involved in discogenic back pain physical therapy exercises are complex and highly individualized. Improper technique, incorrect progression, or misidentifying pain types can worsen the condition or trigger new injuries. For example, performing flexion-based movements when an extension bias is more appropriate can increase disc pressure and nerve irritation. Without a trained eye to monitor form and adapt protocols, patients may unknowingly reinforce harmful compensation patterns. It’s strongly recommended to start under professional supervision and gradually transition to a home-based program once proper movement patterns are established.
4. Can exercises for lower back pain bulging disc conditions be effective even after years of chronic pain?
Absolutely, though the path may be more gradual and require additional multidisciplinary strategies. Chronic pain often results in deconditioned muscles, altered pain processing in the nervous system, and psychological barriers such as fear-avoidance behaviors. Nonetheless, when introduced carefully, exercises for lower back pain bulging disc rehabilitation can retrain the nervous system, rebuild core endurance, and improve functional confidence. Patients may benefit from combining exercise therapy with cognitive-behavioral therapy or pain neuroscience education to reframe their relationship with movement. Long-term sufferers should expect a progressive, holistic approach rather than a quick fix.
5. How do discogenic back pain physical therapy exercises compare to surgical intervention for disc bulges?
In many cases, discogenic back pain physical therapy exercises can offer equivalent or superior long-term results compared to surgery, especially for non-emergency bulging discs. Numerous studies show that conservative treatment—including guided therapeutic exercise—can lead to significant improvements in pain, mobility, and quality of life without the risks associated with surgical intervention. Surgery may be necessary in cases of severe neurological compromise or persistent symptoms that don’t respond to conservative care. However, even post-surgical patients are typically prescribed therapeutic exercises as part of their rehabilitation, reinforcing the universal value of physical therapy in discogenic pain management.
6. Are there any specific breathing techniques that can enhance the effects of exercises for lower back pain bulging disc rehabilitation?
Yes, incorporating diaphragmatic breathing can significantly improve the quality and safety of spinal rehabilitation exercises. Proper breath control enhances core engagement and stabilizes intra-abdominal pressure, which supports the lumbar spine during movement. Coordinating breath with movement—such as exhaling during exertion—can prevent valsalva maneuvers that increase disc pressure. Breath-focused techniques also help reduce muscle tension and anxiety, creating a more favorable neuromuscular environment for healing. Some therapists integrate breath training with pelvic floor activation to further improve lumbar-pelvic stability.
7. What role does sleep posture play in complementing discogenic back pain physical therapy exercises?
Sleep posture can have a substantial impact on disc recovery and should not be overlooked as part of a comprehensive management plan. Poor sleep positioning—such as sleeping on the stomach with the neck rotated—can exacerbate spinal misalignment and undo progress made through discogenic back pain physical therapy exercises. A side-sleeping position with a pillow between the knees or a supine position with knees slightly elevated are often better choices. Using a firm mattress that maintains spinal neutrality is equally important. Patients should treat nighttime posture with the same attention to alignment and muscle support as daytime movement patterns.
8. Can wearable tech or digital apps improve outcomes when using exercises for lower back pain bulging disc recovery?
Yes, the integration of wearable sensors and digital feedback tools is becoming increasingly common in physical therapy. These devices can monitor spinal posture, core engagement, and movement accuracy in real-time, offering immediate corrections and motivational tracking. For patients practicing exercises for lower back pain bulging disc recovery at home, such feedback enhances accountability and helps refine form. Some apps also use gamification or virtual coaching to increase patient engagement, particularly for younger populations. As technology advances, remote rehabilitation supported by real-time metrics is likely to become a key adjunct to traditional in-clinic therapy.
9. What are the signs that discogenic back pain physical therapy exercises need to be modified or paused?
Pain that intensifies during or after exercise, especially if it radiates down the leg, is a red flag that the current routine may need adjusting. Other signs include increased numbness, tingling, or a sudden drop in mobility or strength. Discogenic back pain physical therapy exercises are meant to reduce, not provoke, symptoms—so any worsening should prompt a reassessment. It’s also important to distinguish between muscle soreness, which can be normal in the early stages, and joint or nerve-related pain. A skilled therapist will regularly monitor symptom response and modify movements based on individual tolerance and progression.
10. How can patients transition from therapeutic to preventive exercises after recovering from a bulging disc?
The transition involves a shift from isolated rehabilitation drills to integrated, functional movements that mimic real-life tasks. Once symptoms stabilize, discogenic back pain physical therapy exercises evolve into maintenance routines that emphasize dynamic stability, mobility, and load tolerance. Activities such as Pilates, tai chi, or functional strength training can serve as bridges between recovery and prevention. Patients should continue to monitor form, manage fatigue, and incorporate recovery days to avoid overtraining. Periodic check-ins with a physical therapist or exercise specialist help ensure that movement patterns remain sound and adaptive to new physical demands.
Conclusion: Lasting Relief Through Smart Movement and Consistency
When it comes to managing lower back pain caused by a bulging disc, the most effective solutions are rooted in understanding, action, and consistency. By incorporating evidence-based exercises for lower back pain bulging disc recovery into a structured physical therapy program, individuals can experience significant symptom reduction and functional improvement. These exercises, when performed with proper guidance and personalization, offer lasting discogenic relief without the need for invasive procedures or long-term medication use.
The journey may begin with gentle, targeted movements and evolve into a robust routine that includes core stabilization, stretching, and strength training. Along the way, integrating mind-body techniques, postural awareness, and ergonomic changes can reinforce healing and prevent recurrence. Supervised physical therapy, combined with self-directed effort and education, forms the backbone of sustainable recovery.
In embracing this holistic, exercise-based strategy, patients not only alleviate current discomfort but also invest in their long-term spinal health. Discogenic back pain physical therapy exercises are more than rehabilitative tools—they are keys to freedom, resilience, and renewed quality of life.
Further Reading:
Herniated Disc Pain? 5 Key Exercises to Help


