Understanding Amnesia and the Search for Medical Solutions
Memory is central to the human experience, shaping our identities, relationships, and capacity to function in everyday life. When memory becomes impaired, as in cases of amnesia, the effects can be devastating and disorienting. Amnesia is not a single condition but rather an umbrella term encompassing various forms of memory loss. These range from transient episodes triggered by trauma or emotional stress to chronic and progressive conditions caused by neurological damage. For decades, researchers and clinicians have worked tirelessly to uncover effective ways to treat amnesia, leading to the development and refinement of pharmaceutical interventions. But the question remains: can amnesia medication truly restore lost memories or at least halt the decline? As science continues to explore the depths of cognitive dysfunction, modern amnesia drugs and treatment approaches offer both promise and limitation.
Amnesia may be caused by a multitude of factors, including traumatic brain injury (TBI), stroke, infections, prolonged substance abuse, or degenerative diseases like Alzheimer’s. While some forms of memory loss are reversible, others may be permanent, depending on the extent of the underlying neurological damage. Because amnesia can stem from diverse origins, treatment strategies must be tailored to the specific cause and type of memory loss. This personalized approach is critical for determining whether amnesia medicine can deliver meaningful results. Rather than a one-size-fits-all solution, effective care hinges on understanding the patient’s neurobiology, medical history, and current cognitive function.
The concept of an “amnesia drug” might sound like science fiction, yet there are medications currently used to manage symptoms of memory loss in both clinical and experimental settings. Some drugs are designed to improve neurotransmitter function, especially in areas of the brain involved in memory consolidation and retrieval. Others may seek to reduce inflammation or protect neurons from oxidative stress. Still, while pharmaceutical options can provide support, they are not magic bullets. For many individuals with amnesia, recovery involves a multifaceted regimen that includes cognitive therapy, lifestyle modification, and in some cases, social and emotional support networks. To fully appreciate the potential and limitations of amnesia medication, it’s important to examine the science behind memory, the pharmacology of available treatments, and the real-world outcomes experienced by patients.
You may also like: What to Eat to Boost Memory: Science-Backed Brain Foods That Improve Recall, Focus, and Long-Term Mental Health
How Memory Works: A Foundation for Understanding Amnesia Medication
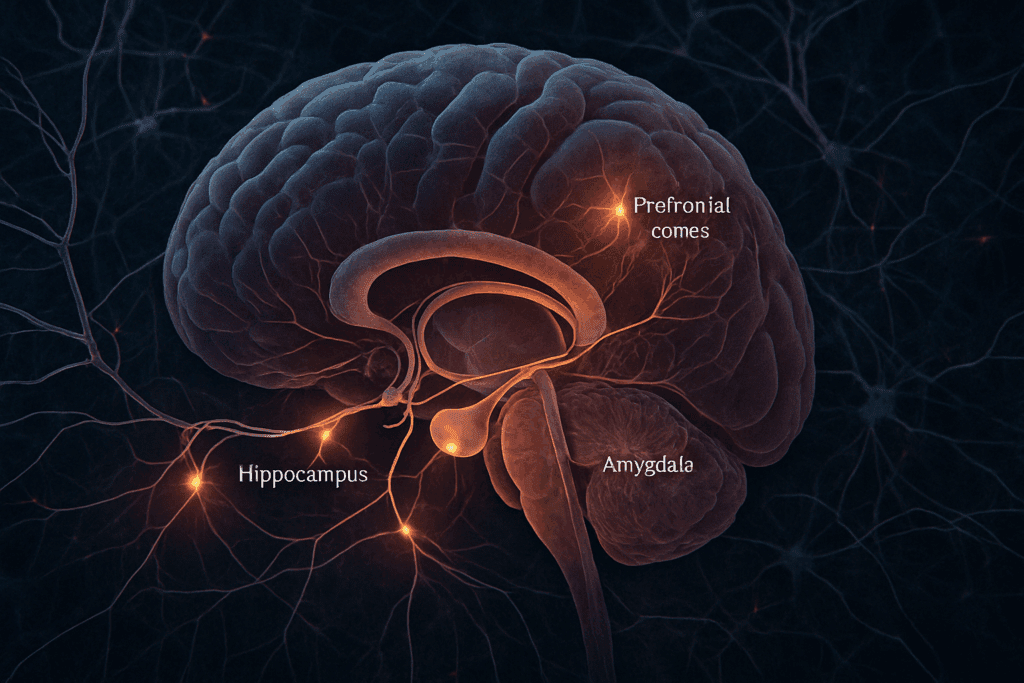
To grasp how an amnesia drug might aid memory recovery, we must first understand the biological underpinnings of memory itself. Memory formation involves a complex interplay between different regions of the brain, particularly the hippocampus, amygdala, and prefrontal cortex. These structures communicate through intricate networks of neurons, utilizing chemical messengers known as neurotransmitters. Among these, acetylcholine, glutamate, dopamine, and serotonin play key roles in encoding, storing, and retrieving memories. When this delicate system is disrupted by injury, illness, or degeneration, the result can be partial or complete memory loss.
The hippocampus, often referred to as the brain’s memory center, is especially vulnerable to damage in cases of anterograde amnesia, where new memories cannot be formed. Retrograde amnesia, by contrast, involves the loss of pre-existing memories and often implicates broader neural circuits. In either case, the loss of neuronal integrity or impaired synaptic communication leads to the symptoms typically associated with amnesia. It is within this neurobiological context that amnesia medication seeks to intervene. By enhancing neurotransmitter activity or protecting neurons from further damage, these drugs aim to restore functionality to the memory-related areas of the brain.
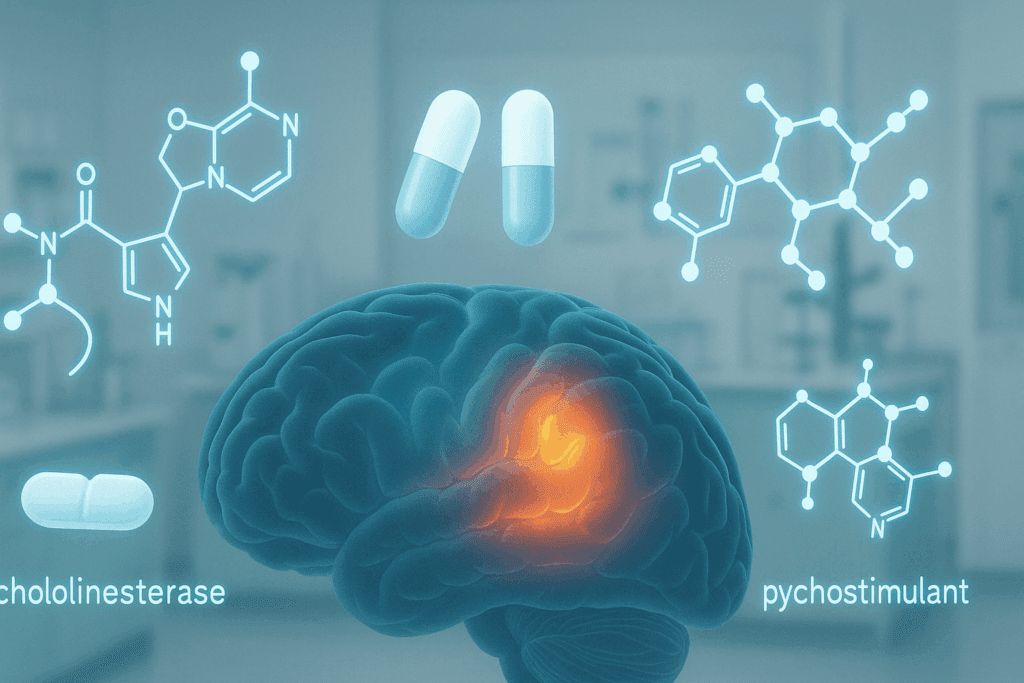
One prominent class of amnesia medicine targets cholinergic pathways. Drugs such as donepezil and rivastigmine, often used in the treatment of Alzheimer’s disease, are acetylcholinesterase inhibitors that increase the availability of acetylcholine in the brain. By preventing the breakdown of this critical neurotransmitter, these medications can enhance cognitive performance and may help individuals with certain types of amnesia recover memory function. However, the efficacy of these drugs varies significantly depending on the etiology and severity of memory loss. While they may offer meaningful improvements in cases of mild to moderate cognitive impairment, their benefits are less clear for individuals with severe brain trauma or long-standing neurological disease.
In addition to cholinergic drugs, some researchers have explored the use of glutamate-modulating medications like memantine, which blocks the NMDA receptor and prevents excitotoxicity—a condition where excessive stimulation leads to neuron damage. Such interventions aim to protect existing memory structures while facilitating neuroplasticity, the brain’s ability to form new neural connections. Together, these pharmacological approaches represent a growing toolkit in the effort to address memory loss, though none offer a complete cure. Instead, they serve as important components of a broader therapeutic strategy, underscoring the multifactorial nature of memory recovery.
Modern Amnesia Drugs: What the Evidence Shows
Scientific research into amnesia drugs has advanced significantly over the past few decades, fueled by improved imaging technologies, animal models, and clinical trial methodologies. While no single medication has emerged as a definitive solution for memory loss, several have shown promise in specific contexts. One of the most extensively studied drug categories in this realm includes cholinesterase inhibitors, which have demonstrated modest efficacy in slowing cognitive decline associated with neurodegenerative diseases. Although originally developed for Alzheimer’s, these drugs are sometimes prescribed off-label to individuals with non-Alzheimer’s forms of amnesia, including those recovering from TBI or encephalitis.
Amnesia medication is not limited to cholinergic agents. Psychostimulants such as methylphenidate and modafinil have also been explored for their potential to enhance attention and working memory in individuals with cognitive deficits. While these drugs are more commonly associated with attention deficit hyperactivity disorder (ADHD) or narcolepsy, studies have indicated that they may improve executive function in select amnesic patients. These benefits are typically short-term and require careful monitoring due to the risk of dependency or cardiovascular side effects. Nonetheless, their ability to support focus and mental clarity can be invaluable for patients engaged in cognitive rehabilitation programs.
Another intriguing area of exploration involves the use of nootropic agents, sometimes referred to as “smart drugs.” Substances like piracetam, aniracetam, and oxiracetam have garnered attention for their purported cognitive-enhancing effects, particularly in aging populations or individuals with neurological deficits. While clinical data on these compounds remain mixed, some studies suggest they may increase cerebral blood flow, enhance mitochondrial function, or modulate neurotransmitter release. The challenge lies in separating anecdotal enthusiasm from empirical evidence, as many of these agents are available as supplements with limited regulatory oversight. Despite the uncertainty, nootropics continue to be a focal point in the search for effective amnesia medicine, especially as interest grows in personalized and preventative approaches to cognitive decline.
Beyond individual compounds, researchers are investigating combination therapies that integrate pharmacological agents with behavioral interventions. For example, pairing memory-enhancing drugs with structured cognitive training may yield synergistic benefits, allowing patients to leverage neurochemical support while actively engaging memory circuits. In some cases, medications may be used to prime the brain for learning, while therapy reinforces the neural pathways responsible for memory retention. This integrative approach acknowledges that while drugs can modulate the biological foundations of memory, behavioral inputs are often essential for lasting change. Thus, the future of amnesia drug development may lie not in a single breakthrough molecule but in the thoughtful coordination of multiple therapeutic avenues.
Personalized Treatment Strategies and Clinical Realities
Despite the growing arsenal of medications for memory loss, the clinical reality remains that amnesia is a highly individualized condition. What works for one person may have limited effect in another, depending on variables such as age, genetics, health status, and the specific nature of the memory impairment. Personalized medicine, an emerging field that tailors treatment based on a patient’s genetic and biological profile, holds considerable promise for optimizing the use of amnesia medication. Advances in genomics and biomarker analysis allow clinicians to predict how a person might respond to a given drug, thereby improving outcomes and reducing the risk of adverse effects.
In real-world settings, the success of an amnesia drug often depends on how well it is integrated into a broader care plan. This includes not only pharmacological treatment but also rehabilitation, psychological support, and lifestyle interventions. For example, patients recovering from a head injury may benefit from medications that support neuroplasticity while also participating in speech therapy and occupational training. Likewise, individuals with degenerative conditions may experience improved quality of life through a combination of medication, social engagement, and mental stimulation. The goal is not merely to restore lost memories but to enhance overall cognitive resilience and adaptability.
It is also essential to recognize the limitations of current medications. While many amnesia drugs can provide symptomatic relief, few address the root causes of memory loss, especially when structural damage is involved. In cases of severe brain trauma or advanced dementia, the potential for meaningful recovery may be constrained. Nevertheless, even modest improvements in memory or attention can have a profound impact on a patient’s ability to function independently and maintain emotional well-being. Thus, the role of medication should be viewed not as a cure but as a tool that, when used judiciously, can significantly enhance therapeutic outcomes.
Ultimately, the decision to use amnesia medication must be made collaboratively between patient and provider, taking into account the full spectrum of potential benefits and risks. Informed consent, ongoing monitoring, and flexibility in treatment planning are critical components of ethical care. As new research continues to illuminate the mechanisms underlying memory loss, clinicians will be better equipped to match patients with the interventions most likely to succeed. This evolving landscape underscores the importance of individualized care in achieving optimal results in the management of amnesia.

The Ethical and Societal Dimensions of Treating Memory Loss with Medication
The pursuit of effective treatments for memory loss raises not only scientific questions but also complex ethical and societal considerations. As amnesia drugs become more sophisticated and widely used, healthcare providers and policymakers must grapple with issues of accessibility, consent, and long-term impact. For instance, should amnesia medicine be made available to individuals with mild cognitive complaints, or reserved only for those with clinically significant impairment? This question touches on broader debates about medicalization, the definition of disease, and the boundaries between therapy and enhancement.
Access to treatment is another pressing concern. Many of the most effective medications for memory loss are expensive and may not be covered by insurance, particularly if prescribed off-label. This creates disparities in care, where only certain populations can afford cutting-edge therapies. In addition, some amnesia medications may carry risks of side effects, addiction, or interactions with other drugs. Informed consent is therefore essential, especially when dealing with vulnerable populations who may already experience confusion or difficulty processing information. Clinicians must balance the hope of improvement with a realistic appraisal of potential downsides.
From a societal perspective, the increasing use of amnesia drugs also raises questions about identity and authenticity. If memory shapes who we are, what does it mean to alter that process pharmacologically? For some, the restoration of lost memories represents a return to self; for others, it may feel intrusive or unnatural. These philosophical issues become even more pronounced when considering future technologies that might one day allow for targeted memory editing or enhancement. While such innovations remain speculative, they highlight the need for ongoing ethical dialogue as science advances.
In the meantime, it is crucial that the development and distribution of amnesia medication be guided by principles of equity, transparency, and respect for patient autonomy. This includes rigorous testing, clear labeling, and thoughtful education about both the potential and limitations of pharmaceutical interventions. By fostering a culture of informed decision-making and inclusive access, society can ensure that memory-enhancing treatments are used responsibly and effectively. The journey to reclaiming memory is as much a moral endeavor as a medical one, requiring compassion, insight, and a commitment to the dignity of every patient.
Frequently Asked Questions: Amnesia Medication, Treatment Innovations, and Long-Term Outlook
1. How do lifestyle factors influence the effectiveness of amnesia medication?
While amnesia medication plays a critical role in symptom management, its effectiveness is often intertwined with a patient’s daily habits. Sleep quality, diet, physical activity, and cognitive engagement can all influence how well an amnesia drug performs. For instance, individuals who maintain regular sleep cycles and engage in mental exercises like puzzles or language learning often respond better to treatment. These activities support brain plasticity and can amplify the benefits of amnesia medicine by reinforcing neural pathways. Therefore, the integration of lifestyle adjustments alongside medication enhances the brain’s ability to adapt and recover, making a holistic approach crucial for long-term memory improvement.
2. Can amnesia drugs be used preventatively for those at risk of memory decline?
Using an amnesia drug as a preventative tool is an emerging concept, though it’s still under investigation. Some neurologists suggest that certain amnesia medicines, such as cholinesterase inhibitors, may delay the onset of memory symptoms in high-risk individuals, particularly those with mild cognitive impairment. However, long-term preventive use of amnesia medication is controversial due to the risk of side effects and limited data on efficacy in asymptomatic individuals. Current research is exploring biomarkers that could help identify who might benefit most from such early intervention. Until more evidence is available, preventative use should be cautiously considered and supervised by a medical professional.
3. Are there significant differences in how men and women respond to amnesia medication?
Emerging studies suggest that biological sex may influence how the brain responds to certain amnesia drugs. Differences in hormone levels, brain structure, and metabolism can affect both the absorption and impact of amnesia medicine. For instance, estrogen appears to have a protective effect on memory, potentially altering how women respond to cholinergic-based treatments. Men, on the other hand, may metabolize some amnesia medications more rapidly, which could affect their therapeutic window. Personalized dosing strategies that account for sex-based physiological differences are increasingly being explored to optimize treatment outcomes.
4. What role do genetics play in determining the success of amnesia drugs?
Genetic variations can significantly influence an individual’s response to amnesia medication. Certain gene polymorphisms, such as APOE-e4, are linked to a higher risk of memory-related conditions and may alter drug metabolism. Individuals with these markers might require customized dosing or benefit more from specific classes of amnesia drugs. Pharmacogenomic testing is becoming a valuable tool in identifying the most effective treatments for each patient. As the field evolves, tailoring amnesia medicine based on genetic makeup may enhance efficacy and reduce unwanted side effects.
5. How does amnesia medication interact with treatments for co-existing conditions?
Patients with memory loss often have other health issues, such as cardiovascular disease, diabetes, or depression, all of which can complicate treatment. Many amnesia drugs interact with medications used to treat these conditions, influencing absorption, efficacy, or side effect profiles. For instance, certain antidepressants can either enhance or blunt the effect of amnesia medicine, depending on the neurotransmitter systems involved. Careful medication management and cross-specialty collaboration are essential to ensure that treatment regimens are both safe and synergistic. Comprehensive care planning can help avoid adverse reactions and optimize cognitive outcomes.
6. What are some promising experimental alternatives to traditional amnesia medicine?
Innovative treatments beyond conventional amnesia drugs are gaining traction in clinical research. One area of exploration includes gene therapy aimed at regenerating damaged neural circuits responsible for memory. Additionally, the use of neurostimulation techniques, such as transcranial magnetic stimulation (TMS), has shown early promise in enhancing memory retention. There’s also growing interest in psychedelic-assisted therapy, where substances like psilocybin are studied for their potential to reshape cognitive frameworks in memory-impaired individuals. While these experimental interventions are not yet mainstream, they represent a future frontier in supplementing or even replacing traditional amnesia medication.
7. How do cultural attitudes impact the prescription and acceptance of amnesia drugs?
Cultural beliefs significantly shape how amnesia medication is perceived and used around the world. In some cultures, memory loss is viewed as a natural part of aging, and pharmacological treatment may be resisted in favor of traditional or herbal remedies. Conversely, in societies with a strong emphasis on cognitive performance and independence, there may be greater openness to using an amnesia drug for even mild memory issues. These differences influence both access to and the effectiveness of interventions, as patient attitudes directly affect medication adherence. Understanding cultural context allows clinicians to frame treatment options in ways that respect beliefs while promoting evidence-based care.
8. What are the risks of over-reliance on amnesia medication without cognitive rehabilitation?
Using an amnesia drug without concurrent cognitive therapy can lead to a plateau in recovery. While medication can support neurotransmitter function, it does not teach the brain how to form or retrieve memories. Over-reliance on pharmacological solutions may foster passivity in the rehabilitation process, potentially delaying more sustainable improvements. Long-term success often requires a dual strategy where amnesia medicine creates a more favorable neurochemical environment while therapy retrains the brain through structured mental exercises. Without this complementary approach, patients may experience only short-lived or superficial gains.
9. Are there socioeconomic barriers to accessing effective amnesia treatment?
Access to quality amnesia medicine often depends on socioeconomic factors, including income level, insurance coverage, and proximity to specialized care centers. High out-of-pocket costs for brand-name amnesia drugs or off-label prescriptions can be prohibitive for many patients. Moreover, those in rural or underserved areas may lack access to neurologists or cognitive rehabilitation services that complement pharmaceutical treatment. These disparities highlight the need for broader health equity initiatives, including better coverage for memory care and more investment in community-based treatment programs. Expanding access could improve outcomes and reduce the burden of untreated memory loss.
10. What future advancements are likely to reshape how amnesia is treated?
The future of treating memory loss with amnesia medication is likely to be shaped by precision medicine and neurotechnology. Advances in brain imaging and artificial intelligence are making it easier to map individual cognitive profiles and predict drug responses. Personalized amnesia drugs designed for specific memory subtypes—such as episodic or semantic memory loss—could become the norm. Additionally, wearable neurofeedback devices may eventually work in tandem with amnesia medicine to provide real-time cognitive monitoring and adjustment. These innovations promise a more dynamic and responsive approach to memory care, with the goal of not only managing symptoms but actively reversing neural decline.
Conclusion: The Evolving Promise of Amnesia Medicine in the Quest to Restore Memory
The question of whether amnesia medication can truly help with memory loss is both urgent and nuanced. While no single amnesia drug offers a cure, a growing body of evidence suggests that certain medications can play a meaningful role in managing symptoms, supporting cognitive function, and improving quality of life. These pharmacological tools are most effective when integrated into a comprehensive treatment plan that addresses the biological, psychological, and social dimensions of memory impairment. From cholinesterase inhibitors to nootropics, and from personalized medicine to ethical reflection, the landscape of amnesia treatment is rich with possibility and complexity.
As scientific understanding of the brain continues to deepen, the development of more targeted and effective amnesia drugs remains a critical goal. Yet even the best medication is unlikely to succeed in isolation. True progress will come from interdisciplinary collaboration, patient-centered care, and a willingness to embrace both the challenges and hopes that memory loss entails. In this evolving field, the future of amnesia medicine lies not only in molecules and mechanisms but in the profound human desire to remember, reconnect, and reclaim the threads of personal history that make us who we are.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Medications and Drugs for Treatment of Amnesia
Understanding Amnesia: Causes, Symptoms, and Treatment Options to Help You Cope
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.


