Cartilage damage in the knee is a common yet often misunderstood condition, one that can profoundly impact mobility, physical confidence, and overall quality of life. Whether due to injury, age-related degeneration, or chronic conditions such as osteoarthritis, compromised knee cartilage can lead to pain, swelling, stiffness, and a reduced capacity to perform even the most basic movements. While surgical interventions like microfracture or cartilage transplantation are sometimes recommended, emerging evidence suggests that the right non-invasive strategies—including specific, well-designed exercises—can play a powerful role in both knee cartilage repair and ongoing joint support. For those seeking a long-term, natural solution, expert-approved exercises for knee cartilage problems may offer both relief and regeneration.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
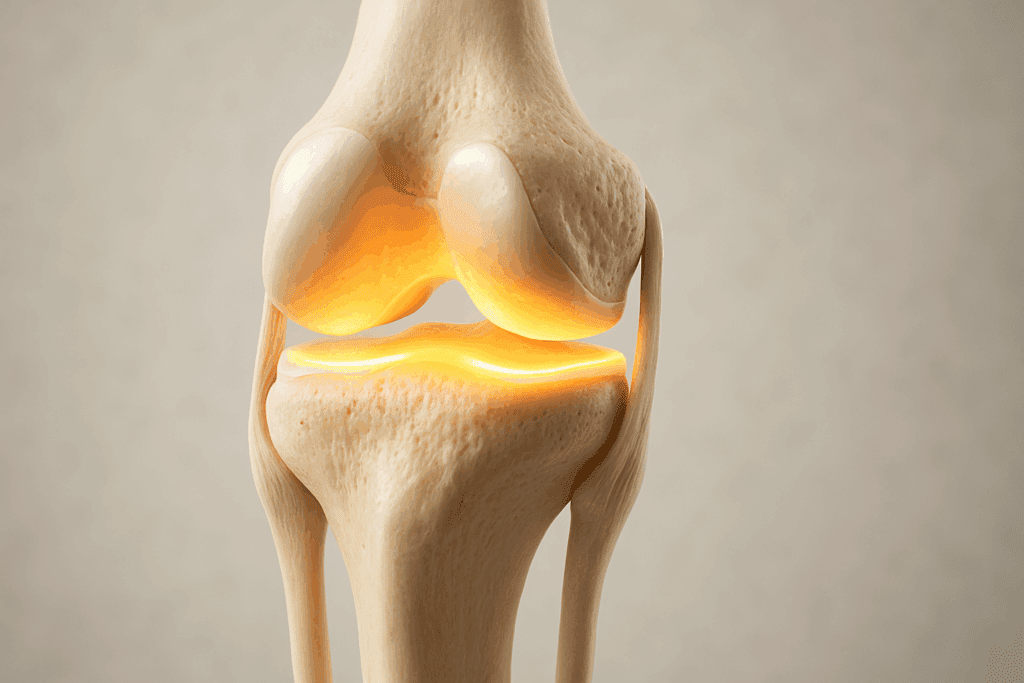
Understanding Knee Cartilage and Why It Matters
The knee is a complex joint, comprised of bones, ligaments, tendons, and most crucially, cartilage. Articular cartilage is a smooth, rubbery tissue that covers the ends of bones where they meet in the joint. It acts as a cushion and shock absorber, ensuring pain-free movement. Unfortunately, because cartilage lacks its own blood supply, it has a limited ability to heal when damaged. This makes early intervention through targeted movement strategies essential.
In many cases, the source of pain and dysfunction lies in the wear and tear of this protective layer. Activities that are high-impact or involve repetitive strain—such as running, jumping, or kneeling—can gradually erode cartilage. Equally, long periods of inactivity or poor biomechanics can contribute to deterioration. This dual vulnerability underscores the importance of incorporating specific knee cartilage repair exercises into any rehabilitation or prevention plan.
The Science Behind Exercise for the Knees with a Damaged Cartilage
Exercise, when approached correctly, promotes the flow of synovial fluid, a lubricating substance in joints that delivers essential nutrients to cartilage. Controlled, low-impact movements stimulate chondrocytes—the specialized cells responsible for maintaining cartilage structure. Unlike passive treatments, movement-based interventions actively engage the body’s intrinsic healing mechanisms. Moreover, strength-building exercises stabilize the joint, reduce strain on the cartilage, and improve proprioception, which helps prevent future injuries.
For those with existing cartilage problems, the challenge is to engage in physical activity without exacerbating the damage. This is where expert guidance is critical. Well-structured exercise for the knees with a damaged cartilage typically includes a combination of mobility drills, isometric strengthening, and carefully progressed load-bearing activities. These routines, supported by scientific research and clinical application, represent a safe and effective approach to managing knee cartilage concerns naturally.
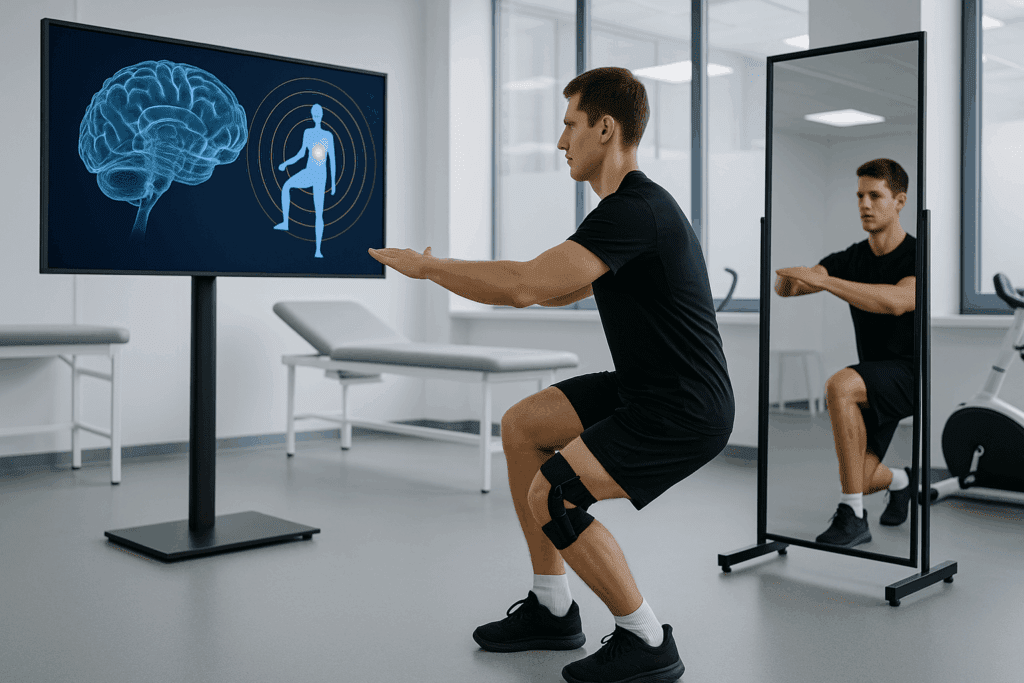
Neuromuscular Reeducation: Retraining the Brain-Knee Connection
An often-overlooked aspect of joint recovery is neuromuscular control—the ability of the nervous system to effectively coordinate muscle activation around the knee. Damage to cartilage can subtly impair motor patterns, leading to compensatory movement strategies that further stress the joint. Neuromuscular reeducation aims to retrain these movement patterns through task-specific exercises, tactile feedback, and muscle stimulation techniques.
Advanced approaches such as biofeedback training allow patients to visualize their muscle engagement in real time, fostering greater body awareness and movement precision. Techniques like mirror therapy and visual motor training help recalibrate the mind-muscle connection, reducing asymmetries and promoting symmetrical gait mechanics. In some rehabilitation settings, electrical stimulation is paired with active movement to reinforce proper firing sequences of muscles like the quadriceps and gluteals.
Incorporating neuromuscular reeducation into a program of exercises for knee cartilage problems can improve functional stability and reduce the risk of chronic compensatory strain. Over time, this results in smoother, more efficient movement that conserves joint integrity and enhances quality of life.
Fascial Release and Manual Therapies to Improve Joint Function
The health of knee cartilage cannot be considered in isolation from the surrounding fascial and connective tissues. Fascia, the web-like tissue enveloping muscles and joints, plays a significant role in force transmission and joint alignment. When fascial adhesions or trigger points develop—often as a response to injury or overuse—they can limit range of motion and contribute to uneven joint loading.
Myofascial release, both manual and tool-assisted, can restore tissue glide and reduce tension on the knee joint. Techniques such as instrument-assisted soft tissue mobilization (IASTM) or fascial cupping help loosen bound connective tissue, promote local circulation, and facilitate more symmetrical movement patterns. Massage therapy and trigger point release in the quadriceps, hamstrings, and hip flexors can also improve knee mechanics by addressing muscular tightness upstream of the joint.
When combined with knee cartilage repair exercises, these therapies provide a supportive foundation for movement efficiency. Releasing restrictive tissues prior to exercise ensures that joint loading is more evenly distributed, reducing wear and enhancing the potential for tissue adaptation.

Blood Flow Restriction (BFR) Training to Stimulate Muscle Growth Safely
One of the most innovative techniques currently used in knee rehabilitation is blood flow restriction (BFR) training. This method involves the application of a specialized cuff or band around the upper thigh to restrict venous return while maintaining arterial inflow. The resulting environment mimics high-intensity exercise effects using only low-load resistance—ideal for patients who need to protect fragile cartilage.
Studies show that BFR training can stimulate hypertrophy and strength gains comparable to traditional heavy lifting, without imposing excessive stress on the joint. This makes it especially useful in early to mid-phase rehabilitation for individuals who cannot tolerate standard weight-bearing protocols. When used correctly under professional supervision, BFR can accelerate muscle development around the knee, offering critical support to the joint and potentially enhancing the outcomes of other knee cartilage repair exercises.
Clinical Integration of Kinesiology Taping and Bracing
Although bracing is often viewed as a passive solution, modern bracing technologies and kinesiology taping techniques can play an active role in rehabilitation by facilitating better movement patterns. Kinesiology tape, applied with specific tension and direction, can provide gentle sensory input that guides muscle activation, encourages lymphatic drainage, and reduces inflammation around the knee.
Custom-fitted knee braces, especially those designed to unload specific compartments of the joint, can also be valuable in cases of cartilage lesions or osteoarthritis. These devices redistribute forces during movement, allowing for more comfortable engagement in exercises for knee cartilage problems. Moreover, the psychological benefit of improved perceived stability can empower patients to move more confidently and consistently.
Nutritional Support for Cartilage Regeneration and Joint Health
Exercise is only one component of a holistic joint health strategy. Nutritional interventions can provide the raw materials necessary for cartilage maintenance and repair. Collagen peptides, glucosamine, chondroitin sulfate, and hyaluronic acid are among the most studied compounds for their potential to support cartilage integrity.
Recent research also highlights the role of anti-inflammatory nutrients such as omega-3 fatty acids, curcumin, and polyphenols in modulating the inflammatory environment within the joint. By reducing chronic inflammation, these nutrients may create a more favorable milieu for tissue recovery. Ensuring adequate intake of vitamin C and amino acids like proline and glycine is also essential for collagen synthesis.
Hydration plays an often underestimated role in cartilage health, as the tissue is composed primarily of water. Dehydration can reduce the cushioning effect of cartilage and increase friction during movement. Therefore, optimal fluid intake should be part of any knee health program.
Technology-Enhanced Rehabilitation: From Apps to Virtual Reality
Technology is revolutionizing how rehabilitation is delivered and monitored. Smartphone apps now allow patients to follow customized exercise programs with instructional videos, track their progress, and receive reminders for daily practice. Many apps also feature pain-tracking and functional assessment tools that give real-time feedback to users and their therapists.
Virtual reality (VR) and augmented reality (AR) platforms are being explored as immersive tools for pain distraction, movement education, and proprioceptive training. These platforms create gamified environments where users can perform therapeutic movements in a fun and engaging way. Preliminary studies suggest that VR may improve motivation, reduce perceived exertion, and encourage greater consistency in rehabilitation programs.
These technological adjuncts are particularly valuable for home-based care, which has become increasingly important in post-pandemic healthcare models. They also support the goal of long-term adherence to knee cartilage repair exercises, which is essential for meaningful and lasting improvements.

Isometric Exercises: Foundation for Stability Without Joint Stress
Isometric exercises form the cornerstone of early-stage rehabilitation for knee cartilage injuries. These exercises involve contracting a muscle without changing its length, thereby activating stabilizing structures without requiring movement at the joint. For those experiencing pain or instability due to damaged cartilage, isometric holds allow for strength development without mechanical stress on the affected tissues.
One of the most commonly recommended isometric movements is the quadriceps set. By tightening the thigh muscle while the leg remains straight and unmoving, individuals can stimulate muscle fibers critical to knee support. Wall sits, another isometric variation, engage the glutes and quadriceps simultaneously, enhancing support around the knee while promoting muscular endurance. Clinical studies have demonstrated that regular performance of such exercises can improve functional outcomes in patients with osteoarthritis and other cartilage-related conditions.
Importantly, these exercises also serve as a preparatory phase for more dynamic movements. By reinforcing joint stability, they provide a safe platform from which individuals can later progress to weight-bearing and mobility-enhancing routines. For those navigating exercises for knee cartilage problems, isometric strength training offers a low-risk, high-reward entry point.

Low-Impact Strength Training for Joint Protection and Pain Relief
As symptoms stabilize, introducing low-impact strength training becomes essential. This phase of exercise for the knees with a damaged cartilage targets muscle groups that support and align the joint. The primary focus is on the quadriceps, hamstrings, glutes, and calves—each of which plays a key role in knee biomechanics.
Mini squats, performed with proper form and within a pain-free range of motion, can strengthen key stabilizers without overloading the joint. Seated leg presses on low resistance settings offer another safe avenue for strengthening. These types of closed kinetic chain exercises reduce shearing forces on the cartilage while promoting muscle engagement across multiple joints. Resistance bands can also be incorporated for lateral leg lifts or hamstring curls, providing progressive overload in a controlled environment.
Research suggests that individuals engaging in structured strength training experience improvements in both pain and function, even when cartilage damage is present. By reducing muscular imbalances and enhancing neuromuscular control, these exercises contribute to joint stabilization and may slow further degeneration. This makes strength-based interventions a core component of any comprehensive program of knee cartilage repair exercises.
Mobility Work to Restore Functional Range and Prevent Stiffness
Stiffness is a common companion to cartilage degeneration in the knee. As discomfort limits motion, the joint capsule tightens, reducing range and reinforcing dysfunctional movement patterns. Mobility exercises counteract this spiral by gently restoring normal movement, improving circulation, and reducing compensatory stress on surrounding tissues.
Targeted mobility drills such as heel slides, active assisted knee bends, and seated leg extensions help encourage gentle articulation without overloading the joint. Foam rolling the quadriceps and IT band, while not directly addressing cartilage, can alleviate soft tissue tension that may pull the knee into suboptimal alignment. Additionally, ankle and hip mobility work should not be overlooked, as stiffness in these regions often affects knee tracking and contributes to strain.
Consistency is critical when performing mobility routines. Ideally, these should be done daily or as part of a warm-up and cool-down during strength sessions. Over time, improved flexibility and range of motion can lead to decreased pain, improved gait mechanics, and greater confidence in movement—especially in individuals following a long-term plan of exercises for knee cartilage problems.
Hormonal and Genetic Considerations in Cartilage Regeneration
Emerging science is beginning to explore the impact of hormonal balance and genetic predisposition on cartilage health. Estrogen, for example, has been shown to influence cartilage metabolism, which may partly explain the higher incidence of knee osteoarthritis in postmenopausal women. Hormonal optimization, particularly in aging populations, may thus play a role in supporting joint repair.
Genetic testing for markers related to collagen production, inflammatory response, and cartilage integrity is now available through various health platforms. While still an emerging field, this information may one day guide personalized prevention and treatment strategies, including which types of exercise are most beneficial based on genetic predisposition.

Balance and Proprioceptive Training for Injury Prevention
When knee cartilage is compromised, the joint’s ability to sense position and respond to stimuli—known as proprioception—can diminish. This loss contributes to instability and increases the risk of falls or missteps that may aggravate existing injuries. Restoring proprioception through balance-focused exercises is a powerful, though often overlooked, strategy in natural knee rehabilitation.
Basic movements such as standing on one leg, progressing to unstable surfaces like a balance pad or Bosu ball, challenge neuromuscular coordination. Dynamic drills like lateral stepping or single-leg reaches further reinforce the brain-muscle connection, training the body to react appropriately under varying conditions. Tai chi and certain styles of yoga, which emphasize slow, mindful transitions and weight shifts, have also demonstrated benefits in enhancing joint stability and sensory feedback.
Incorporating proprioceptive training into a broader regimen of knee cartilage repair exercises yields dual benefits: it protects against future injury while subtly reinforcing muscular engagement. By improving spatial awareness and response time, these practices ensure that newly regained strength and mobility are integrated into functional, real-world movement.

The Role of Aquatic Therapy in Cartilage Recovery
Water-based exercise offers a unique and valuable environment for individuals with knee cartilage issues. The buoyancy of water reduces the impact on joints while still providing resistance that supports strength gains. This makes aquatic therapy a preferred modality for those with severe pain, obesity, or advanced cartilage degeneration.
Aquatic walking, water aerobics, and underwater cycling enable full joint movement without the gravitational stress of land-based exercise. The resistance of water provides a natural form of gentle resistance training, encouraging muscle activation while protecting sensitive cartilage. In addition, the hydrostatic pressure of water can help reduce inflammation and improve circulation in the lower extremities.
Numerous clinical studies support the effectiveness of aquatic exercise for improving pain, strength, and quality of life in individuals with osteoarthritis or cartilage defects. For those just beginning their rehabilitation journey—or for whom traditional exercise is not yet possible—pool-based movement represents a safe and effective stepping stone in the journey toward joint health.
Sustainable Strategies for Lifelong Joint Health
Ultimately, sustaining joint health in the presence of cartilage damage requires an integrative, multifaceted approach. While exercises for knee cartilage problems remain foundational, the inclusion of advanced strategies such as neuromuscular training, fascial release, BFR, and psychological support provides a more robust framework for healing.
The path to recovery is rarely linear, and setbacks are part of the process. However, by embracing a broad view that includes physical, nutritional, psychological, and technological elements, individuals can not only recover but thrive. The goal is not merely to restore movement but to reclaim the freedom, vitality, and confidence that pain may have taken away.
Incorporating these emerging practices alongside traditional exercise routines empowers individuals to take an active role in their joint health. It reflects a modern, evidence-informed understanding of rehabilitation—one that recognizes the body’s innate capacity for healing when given the right tools, support, and environment to flourish.
Stretching and Yoga for Joint Flexibility and Pain Management
Stretching, when applied correctly, can significantly ease the tension and muscular imbalances that accompany cartilage problems. Tight quadriceps, hamstrings, and hip flexors can pull on the knee joint, altering its mechanics and exacerbating wear. Gentle, sustained stretches aimed at these muscle groups can improve alignment, ease discomfort, and complement strength and mobility efforts.
Yoga adds another layer of benefit, combining stretching with breath awareness, balance, and muscular control. Poses such as Warrior II, Bridge, and Reclining Hand-to-Big-Toe (Supta Padangusthasana) engage the hips and legs while respecting the natural limitations of the knee. Many yoga modifications, including the use of bolsters or blocks, allow individuals with knee issues to practice safely and progressively.
Moreover, the meditative aspect of yoga has been shown to reduce pain perception, stress, and inflammation. This makes it not only a physical tool but a psychological one, helping individuals stay consistent with their rehabilitation regimen and maintain a positive mindset during recovery. For those incorporating exercises for knee cartilage problems into their daily life, yoga offers a holistic approach to healing.
Realistic Expectations and the Importance of Progression
It’s vital to acknowledge that while exercises cannot regenerate cartilage in the traditional sense, they can significantly influence the joint environment to encourage preservation and potentially limited repair. Cartilage adaptation is a slow process, often occurring over months rather than weeks, and requires consistency, patience, and intelligent progression.
Attempting advanced exercises prematurely or training through pain can lead to setbacks and worsen joint damage. Instead, a phased approach, beginning with isometric work and progressing through strength, mobility, and dynamic balance, ensures both safety and effectiveness. Working with a qualified physical therapist or exercise professional experienced in knee rehabilitation is highly recommended to tailor exercises to individual needs and monitor progress.
Incorporating rest days, using ice post-exercise, and maintaining a nutrient-rich diet are additional strategies that support recovery. Nutritional supplements such as glucosamine, chondroitin, and omega-3 fatty acids may also play a supportive role when used under professional guidance. Ultimately, the goal of any exercise for the knees with a damaged cartilage is not only to alleviate symptoms but to create an environment that supports long-term function and minimizes degeneration.
Frequently Asked Questions: Advanced Insights into Knee Cartilage Repair and Exercise Therapy
1. Can overtraining worsen cartilage damage in the knee, even if I’m doing the right exercises?
Yes, overtraining can absolutely hinder recovery—even when you’re performing appropriate exercises for knee cartilage problems. Cartilage responds best to low-load, high-frequency stimulus, meaning moderation is crucial. Repeated overuse without sufficient rest can exacerbate inflammation and degrade joint structures, even during exercise for the knees with a damaged cartilage. It’s essential to vary intensity and allow time for tissue recovery. Active rest days involving mobility work or aquatic therapy can maintain joint engagement without compounding damage.
2. Are there any cutting-edge techniques that can enhance the effects of knee cartilage repair exercises?
Recent advances such as blood flow restriction (BFR) training and neuromuscular electrical stimulation are gaining traction in sports medicine. These methods intensify muscle activation around the knee using lighter loads, which is ideal when managing compromised cartilage. When integrated into exercises for knee cartilage problems, they can accelerate strength gains without increasing joint stress. Clinical use of augmented reality is also on the rise, guiding patients through form-optimized movement. These innovations are particularly promising in personalized rehabilitation plans.
3. How does my body weight influence the success of exercise for the knees with a damaged cartilage?
Excess body weight places amplified pressure on already vulnerable joint surfaces, potentially offsetting the benefits of knee cartilage repair exercises. Research shows that even a modest reduction in weight can significantly reduce joint load and improve exercise tolerance. Maintaining a healthy weight supports better alignment during movement and reduces compensatory strain on surrounding tissues. When combined with proper nutrition and tailored movement programs, weight management becomes a critical factor in cartilage protection. Working with a dietitian alongside a physiotherapist can further optimize outcomes.
4. Is it safe to do high-resistance strength training if I have cartilage degeneration?
Not all resistance training is contraindicated, but heavy loading without proper progression can be risky. For those with advanced cartilage issues, low-resistance, high-rep protocols are typically recommended early on. The goal is to condition the surrounding muscles without increasing compressive stress on the joint. Over time, individuals may progress to moderate loads if symptom-free, using movements that keep the knee in alignment. For sustainable improvement, all exercises for knee cartilage problems should be guided by symptom response and structural limits, not performance goals.
5. What role does cross-training play in maintaining knee health when cartilage is damaged?
Cross-training can be highly beneficial by minimizing repetitive stress while still enhancing cardiovascular and muscular endurance. Swimming, cycling, and elliptical training are excellent low-impact complements to knee cartilage repair exercises. These activities preserve aerobic capacity and promote synovial fluid circulation without excessive joint loading. They also help maintain movement variety, which is crucial for long-term joint resilience. Including cross-training in your routine reduces overreliance on any single movement pattern that might aggravate cartilage problems.
6. Are there psychological barriers that might interfere with my commitment to knee rehabilitation?
Absolutely. Individuals with chronic joint pain often develop kinesiophobia—a fear of movement—that impedes progress. This psychological barrier can make consistent practice of exercise for the knees with a damaged cartilage difficult, even if the movements are safe and effective. Incorporating mindfulness, cognitive-behavioral strategies, or working with a therapist can address these fears. Visualizing successful, pain-free movement and celebrating small progress milestones helps reinforce a positive feedback loop. Mind-body integration is increasingly viewed as essential in orthopedic recovery.
7. How can aging affect the outcomes of exercises for knee cartilage problems?
As we age, cartilage naturally loses its water content and regenerative capacity, making recovery slower and less robust. However, this doesn’t mean repair is impossible—only that expectations must be adjusted and consistency becomes even more important. Aging populations often benefit from longer warm-ups, slower progressions, and increased focus on balance and proprioception. Strengthening the hip and core also becomes more critical to offload the knee joint. Tailoring knee cartilage repair exercises to accommodate age-related changes is key to maintaining independence and mobility.
8. What lifestyle factors can quietly undermine my rehabilitation efforts?
Subtle lifestyle habits can sabotage even the most disciplined exercise plan. For example, poor sleep quality hinders tissue regeneration and can amplify pain sensitivity, reducing motivation for rehab. Chronic dehydration can alter cartilage viscosity, increasing friction during movement. High-sugar or inflammatory diets may worsen joint swelling and stiffness. Additionally, prolonged sitting with poor posture can counteract the benefits of exercise for the knees with a damaged cartilage. A holistic approach that includes nutrition, rest, and ergonomic awareness is crucial for full recovery.
9. How do environmental factors like weather affect cartilage-related knee pain and exercise performance?
While the link isn’t fully understood, many individuals with knee cartilage problems report worsened symptoms during cold, damp weather. Barometric pressure changes are thought to affect joint capsule expansion and fluid dynamics. These changes can lead to increased stiffness and delayed warm-up times during exercise sessions. Strategies like using a heated wrap pre-exercise or increasing warm-up duration can mitigate these effects. It’s also helpful to schedule knee cartilage repair exercises during the warmest part of the day to take advantage of naturally higher tissue elasticity.
10. Can smart technology really help manage exercises for knee cartilage problems at home?
Yes, wearable technology and smartphone applications are revolutionizing home rehabilitation. Devices that track knee angle, step count, or load distribution can provide real-time feedback and reduce form errors during unsupervised sessions. Many apps offer guided routines that ensure progression and maintain motivation. When applied correctly, these tools make home-based execution of exercise for the knees with a damaged cartilage more effective and personalized. They also bridge the gap between clinic visits, allowing continuous adaptation based on data and user feedback.
Conclusion : Choosing the Right Knee Cartilage Repair Exercises for Lifelong Mobility
Choosing the best knee cartilage repair exercises involves more than simply finding movements that don’t hurt—it requires a thoughtful, personalized strategy that respects the complexity of joint health. Through isometric strengthening, low-impact training, mobility work, proprioceptive enhancement, aquatic therapy, and mindful stretching, individuals can forge a path toward reduced pain and improved mobility. Each of these components plays a distinct and complementary role in preserving cartilage and restoring function.
Crucially, these approaches embody the essence of a natural, evidence-based solution. They do not promise miraculous cures but offer real, tangible improvements grounded in science and clinical experience. Whether you’re just beginning your recovery or looking to maintain joint health as you age, integrating expert-backed exercises for knee cartilage problems into your daily life can be transformative. With consistency, professional guidance, and a long-term mindset, it’s possible to move with confidence, strength, and stability—without relying solely on invasive procedures.
In the evolving landscape of musculoskeletal rehabilitation, movement remains medicine. And for those managing knee cartilage concerns, the right exercise is not just therapy—it’s empowerment.
Further Reading:
Best Exercises for Knee Pain & Cartilage Loss
Best Exercises to Relieve Knee Joint Pain
Osteoarthritis of the knee: Learn More – What can you do to strengthen your knees?


