The Overlooked Power of the Small Brain: Why the Cerebellum Deserves Center Stage
When most people think of brain function, they naturally focus on the cerebral cortex—that wrinkled mass responsible for conscious thought, decision-making, and memory. Yet, nestled below this dominant structure lies an intricately folded, walnut-sized region known as the cerebellum. Often referred to as the “small brain,” the cerebellum has long been recognized for its role in coordinating motor functions. However, recent research has turned a revealing spotlight on this modest structure, demonstrating that it is not merely a neural assistant to the cortex but a dynamic participant in regulating emotional stability, attention, and overall mental health. Understanding this shift in perception requires more than a cursory glance at a textbook. A well-annotated cerebellum diagram, especially one where the cerebellum is labeled in detail, reveals a wealth of information about its nuanced internal structure. These visual guides make it easier to appreciate how different cerebellar lobes communicate with the limbic system, brainstem, and higher cognitive centers, and also the labeled cerebellum diagram.
As evidence mounts, the notion of the cerebellum as merely a coordinator of balance and voluntary movement is rapidly evolving. Functional MRI studies show that this small brain engages robustly during tasks involving language, working memory, and emotional regulation. Neuropsychological assessments support this, revealing that damage to the cerebellum can result in mood disorders, disorganized thinking, and even hallucinations. This revelation has profound implications for mental health diagnostics and treatment. For instance, anxiety disorders and autism spectrum conditions are increasingly being linked to structural or functional anomalies within the cerebellum. And while traditional psychiatry often prioritizes neurotransmitter imbalances in the cortex, newer therapeutic interventions are beginning to consider cerebellar neurostimulation and targeted neurofeedback as adjunctive treatments.
Moreover, a detailed cerebellum diagram serves not only as an anatomical guide but as a conceptual map for clinicians and researchers. When the cerebellum is labeled with its various zones—such as the flocculonodular lobe, vermis, and lateral hemispheres—it becomes clearer how each segment supports distinct cognitive and emotional processes. The vermis, for example, appears to be especially involved in affect regulation and social cognition. This kind of labeled visual representation enables a more precise interpretation of how cerebellar anomalies may manifest as psychological symptoms. In sum, recognizing the cerebellum’s broader contributions to mental health transforms our understanding of the brain itself. It no longer suffices to view the cerebellum as the backstage crew of the neural theater; it is, increasingly, a co-director in the drama of mental life.
You may also like: Boost Brain Power Naturally: Evidence-Based Cognitive Training Activities and Memory Exercises That Support Long-Term Mental Health
A Guided Tour Through the Cerebellum: What a Labeled Cerebellum Diagram Reveals
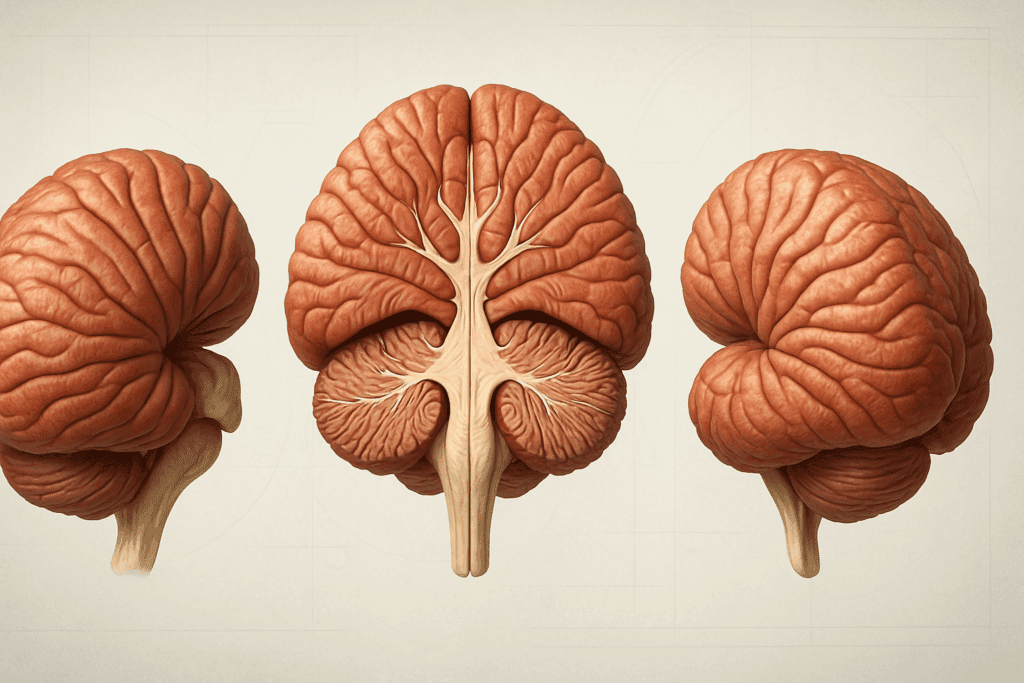
To fully appreciate the cerebellum’s role in mental health, one must first understand its intricate architecture, and the most effective way to do this is through a labeled cerebellum diagram. These diagrams function as anatomical blueprints, offering a visual breakdown of cerebellar subdivisions and their corresponding functions. While the cerebellum may appear compact, it is incredibly dense with neurons and segmented into multiple lobes and hemispheres, each contributing uniquely to the broader landscape of brain function. The anterior and posterior lobes, for example, are instrumental in motor coordination, but they also intersect with neural circuits responsible for executive function and emotional regulation. When each region of the cerebellum is labeled with precision, these relationships become clearer, providing valuable insights for both clinical practice and cognitive neuroscience.
The central portion of the cerebellum, known as the vermis, serves as a bridge connecting both hemispheres and is particularly important in modulating mood and social behavior. This central region connects extensively with the prefrontal cortex and limbic structures, forming a neuroanatomical triangle that governs attention, self-awareness, and empathy. In contrast, the lateral hemispheres are more engaged in fine-tuned motor activity and language processing, revealing just how diverse the functional spectrum of the small brain really is. Understanding this diversity through a cerebellum diagram allows clinicians to localize dysfunction and formulate more personalized treatment approaches. For instance, targeted neurostimulation protocols that aim at specific lobules within the cerebellum are already being explored for treatment-resistant depression and obsessive-compulsive disorder.
Notably, one of the most fascinating discoveries about this small brain is its unexpectedly vast neural connectivity. Despite comprising only about 10% of the brain’s volume, the cerebellum contains more than half of its neurons. A cerebellum diagram that is clearly labeled can illustrate how this dense network communicates through the thalamus and brainstem to influence cortical activity. This communication is not unidirectional; it forms feedback loops that are essential for cognitive modulation. These loops allow the cerebellum to monitor and refine thought processes much like it does with physical movement. It acts as a kind of quality control mechanism, detecting errors in logic or emotion and attempting to adjust in real time. Thus, a labeled cerebellum diagram is more than a teaching tool; it is a lens into a dynamic regulatory system that is critical for mental equilibrium.

Cognitive and Emotional Regulation: Beyond Balance and Coordination
For much of modern neuroscience’s history, the cerebellum was typecast in a limited role—primarily as the conductor of motor symphonies. But a growing body of empirical research now reveals that this small brain plays a much more nuanced role, particularly in cognitive and emotional regulation. Functional neuroimaging studies have repeatedly shown that the cerebellum activates during tasks involving language comprehension, abstract reasoning, and even moral judgment. Such findings challenge the outdated notion that this part of the brain merely coordinates motion and suggests instead that it acts as a central node in a much larger cognitive network. A cerebellum diagram that is well-labeled helps illuminate this complexity by highlighting the anatomical regions involved in these higher-order processes, making it easier for researchers and clinicians alike to interpret neurological data in a psychological context.
The cerebellum’s influence on emotional regulation is particularly striking. Research indicates that lesions or malformations in specific cerebellar lobules—notably within the posterior vermis—can lead to symptoms resembling those of psychiatric disorders, including anxiety, depression, and bipolar disorder. This phenomenon has been termed the Cerebellar Cognitive Affective Syndrome (CCAS), and it provides a clinical framework for understanding how disruptions in cerebellar function can manifest as mood and personality disturbances. When explored through the lens of a labeled cerebellum diagram, the correlation between specific cerebellar damage and particular emotional symptoms becomes increasingly evident. For instance, dysfunction in Crus I and Crus II of the cerebellar hemispheres has been associated with poor working memory and impaired social cognition, traits often observed in individuals with autism spectrum disorder.
In addition to these direct emotional and cognitive influences, the cerebellum also modulates the autonomic nervous system, indirectly impacting mood and psychological resilience. By influencing heart rate variability and stress hormone secretion through connections with the hypothalamus and brainstem, the cerebellum plays a quiet yet pivotal role in how we physiologically respond to stress. These subtle regulatory functions often go unnoticed but are essential for maintaining emotional balance. Understanding these connections through a detailed cerebellum diagram allows for a more integrative approach to mental health care. In clinical settings, recognizing the cerebellum’s contributions can guide diagnostic evaluations and inform holistic treatment plans that address both the emotional and physiological dimensions of mental illness.
Developmental and Neuroplastic Perspectives on the Small Brain’s Role in Mental Health
The influence of the cerebellum on mental health begins early, often shaping cognitive and emotional outcomes long before a person can articulate their inner world. During fetal development, the cerebellum undergoes rapid growth, and disruptions in this process have been associated with an increased risk for developmental disorders. For instance, children born prematurely often exhibit underdeveloped cerebellar structures, which has been correlated with attention deficits and difficulties in emotional self-regulation later in life. These findings suggest that the small brain plays an essential role in scaffolding early neurological frameworks for social and cognitive function. A well-labeled cerebellum diagram is indispensable in this context, helping to identify the regions most affected by developmental anomalies and offering a roadmap for potential interventions during critical windows of neuroplasticity.
The cerebellum’s remarkable capacity for neuroplasticity also makes it a promising target for therapeutic interventions across the lifespan. Neuroplasticity refers to the brain’s ability to reorganize itself by forming new neural connections, and in the cerebellum, this capacity is both robust and enduring. Rehabilitation techniques such as cerebellar transcranial direct current stimulation (ctDCS) and neurofeedback therapy are beginning to leverage this plasticity to treat psychiatric conditions ranging from ADHD to PTSD. These interventions are often guided by cerebellum diagrams that are meticulously labeled, ensuring precise electrode placement or biofeedback targeting. Such precision not only enhances efficacy but also minimizes the risk of unintended neural side effects.
Importantly, the cerebellum does not function in isolation. Its development and plasticity are shaped by interactions with the environment, including sensory experiences, social engagement, and even diet. For example, animal studies have shown that enriched environments can promote cerebellar growth and synaptic density, while chronic stress or malnutrition can impair cerebellar function. These findings underscore the importance of early-life experiences and lifestyle choices in shaping cerebellar health and, by extension, mental health. The cerebellum, although small, is a highly dynamic and sensitive structure that reflects both genetic and environmental influences. Understanding its evolving architecture through the use of a labeled cerebellum diagram can help educators, clinicians, and caregivers develop more supportive and individualized developmental strategies.
Rethinking Psychiatric Diagnosis and Treatment Through the Lens of the Cerebellum
The recognition of the cerebellum’s role in mental health challenges long-standing conventions in psychiatric diagnosis and treatment. Traditionally, the diagnostic framework for mental health disorders has centered around cortical dysfunction and neurotransmitter imbalances, often overlooking subcortical structures like the cerebellum. However, advances in neuroimaging and clinical research now highlight the cerebellum as a critical site of dysfunction in a wide array of psychiatric conditions. These insights invite a reevaluation of diagnostic criteria and therapeutic approaches, advocating for a more integrative neurobiological model. A cerebellum diagram that is thoroughly labeled can serve as an essential tool in this paradigm shift, allowing clinicians to correlate symptom clusters with specific cerebellar regions and tailor interventions accordingly.
For instance, recent studies have linked cerebellar abnormalities to schizophrenia, noting that disruptions in cerebellar-thalamic-cortical circuits can lead to disorganized thinking and auditory hallucinations. Similarly, individuals with major depressive disorder often exhibit reduced cerebellar volume, particularly in the vermis, which may contribute to anhedonia and emotional blunting. These findings suggest that cerebellar imaging could become a standard component of psychiatric assessment, offering new biomarkers for diagnosis and treatment monitoring. A labeled cerebellum diagram not only aids in the interpretation of imaging results but also enhances patient education by making complex neuroanatomical information accessible and understandable.
Therapeutically, interventions that directly target cerebellar function are gaining traction. Repetitive transcranial magnetic stimulation (rTMS) of cerebellar regions is being explored as a non-invasive treatment for depression and anxiety, while pharmacological agents that modulate cerebellar neurotransmission are under investigation for their mood-stabilizing effects. These emerging therapies rely on precise anatomical targeting, which in turn depends on accurate cerebellum diagrams. When the cerebellum is labeled in detail, it becomes possible to develop customized treatment plans that address the unique neurobiological profiles of individual patients.
Furthermore, integrating cerebellar assessments into mental health care encourages a more holistic approach that recognizes the interplay between movement, emotion, and cognition. Yoga, dance therapy, and other movement-based interventions that engage the cerebellum have shown promise in improving mood and cognitive flexibility. These practices underscore the cerebellum’s role not only as a site of pathology but as a potential hub for healing. Ultimately, a nuanced understanding of the small brain, supported by detailed cerebellum diagrams, can help usher in a new era of personalized, brain-based mental health care.
FAQ: The Cerebellum’s Influence on Mental Health and Function
1. How might understanding the cerebellum enhance psychological therapies in the future?
Emerging insights into the cerebellum’s role in emotional regulation and cognitive feedback loops are already influencing how we think about psychotherapy. Future therapies may incorporate real-time neurofeedback guided by a cerebellum diagram that is dynamically linked to patient symptoms. For instance, using a cerebellum labeled for emotion-related zones, therapists could personalize mindfulness or biofeedback exercises based on which regions are underactive. Integrating these strategies could help modulate emotional resilience, especially in treatment-resistant anxiety and depression. Since the small brain maintains connections with the limbic system, its targeted engagement may support more durable emotional regulation outcomes. Researchers are also exploring transcranial stimulation techniques directed at cerebellar regions to enhance emotional flexibility and cognitive reappraisal strategies. In the future, psychotherapy might look more like a hybrid model of talk therapy combined with personalized neuromodulation protocols grounded in cerebellar science.
2. Can the cerebellum influence creativity and imaginative thinking?
Yes, recent research suggests the cerebellum’s role extends well beyond coordination and emotional regulation, with potential implications for creativity. Functional neuroimaging shows that during imaginative or divergent thinking tasks, parts of the small brain activate in synchrony with the default mode network—the brain’s introspective and idea-generating system. When explored using a cerebellum diagram that highlights connectivity zones, such as Crus I and II, a pattern of interaction with the prefrontal cortex becomes evident. These regions may act as neural moderators that refine and streamline creative impulses before they’re expressed. A cerebellum labeled to include linguistic and symbolic interpretation zones also points to its role in metaphor generation and conceptual blending. This means that artists, writers, and problem-solvers might benefit from cerebellar-enhancing practices like rhythmic movement or coordinated fine-motor tasks, which indirectly stimulate imaginative thinking through cerebellar-cortical loops.
3. How does cerebellar health affect social behavior and empathy?
The cerebellum’s interaction with social behavior is one of its most compelling and underexplored functions. A well-labeled cerebellum diagram shows connections between the vermis and regions of the brain associated with empathy, such as the medial prefrontal cortex. This small brain structure plays a subtle yet important role in interpreting social cues, regulating emotional tone in conversation, and maintaining prosocial behavior. Impairments in these cerebellar areas have been observed in individuals with autism spectrum disorder and certain personality disorders, suggesting a link between cerebellar dysfunction and diminished empathy. Interventions that support cerebellar activity, including mirror neuron training or social rhythm therapies, could offer promising approaches for enhancing interpersonal connection. Additionally, developmental neuroscience supports the idea that social bonding in early childhood helps strengthen cerebellar networks, further underscoring the lifelong importance of cerebellar health for human connection.
4. What role does the cerebellum play in stress regulation and trauma response?
Though often overlooked in discussions of stress, the cerebellum is deeply involved in modulating autonomic nervous system responses. A cerebellum diagram can help illustrate how this small brain structure communicates with the hypothalamus, a major player in hormonal stress regulation. When the cerebellum is labeled to include its connections with the brainstem, its regulatory reach over heart rate, blood pressure, and cortisol release becomes more apparent. These functions are particularly relevant for trauma survivors who experience heightened sympathetic arousal. New therapeutic modalities such as vagus nerve stimulation and cerebellar tDCS, are being evaluated for their ability to recalibrate this system. Moreover, body-based practices like tai chi and gentle yoga—which engage the cerebellum’s motor coordination systems—may serve as indirect tools to quiet overactive stress responses through cerebellar-mediated regulation.
5. How is the cerebellum involved in long-term emotional memory?
Although typically associated with motor memory, the cerebellum is increasingly recognized for its contributions to emotional memory consolidation. Studies using cerebellum diagrams with labeled posterior lobules reveal connectivity with the amygdala and hippocampus, structures central to emotional learning. The small brain seems to refine and filter emotional memories, making them less reactive over time. This could explain why individuals with cerebellar injury often report inappropriate emotional responses or difficulty letting go of negative past experiences. Advanced imaging suggests that during sleep, the cerebellum participates in emotional memory processing, particularly REM phases. This opens new discussions around how sleep quality affects cerebellar function and, by extension, emotional health. Targeted interventions that optimize sleep architecture might thus be beneficial not just for rest but for cerebellar-mediated emotional recalibration.
6. Could cerebellar stimulation enhance learning and academic performance?
There is growing interest in using non-invasive cerebellar stimulation to support learning, attention, and memory consolidation. Clinical trials have shown promising results in using tDCS applied to regions identified in a detailed cerebellum diagram, particularly when the cerebellum is labeled to show cognitive and executive regions like Crus I. This small brain structure helps automate repetitive tasks and may reduce cognitive load, making mental processing more efficient. Enhancing these pathways could help students, especially those with learning differences, retain and integrate new material more fluidly. Real-world applications include cognitive tutoring systems that incorporate rhythm-based tasks or motion-coordination games designed to engage cerebellar circuits. These interventions don’t replace traditional education but may serve as neurological primers that boost the brain’s readiness to learn.
7. In what ways does the cerebellum affect sleep and circadian regulation?
Though less studied than its role in movement and emotion, the cerebellum influences both sleep quality and circadian rhythms. A cerebellum diagram can show how this small brain structure communicates with the suprachiasmatic nucleus and brainstem regions that govern sleep-wake cycles. When the cerebellum is labeled for its autonomic connections, researchers can better understand its subtle contributions to melatonin regulation and REM cycling. Poor cerebellar function may contribute to sleep disorders such as insomnia, particularly when tied to emotional dysregulation. Enhancing cerebellar health through structured sleep hygiene practices, blue-light reduction, and physical activity may support more restorative sleep patterns. As sleep and mental health are tightly linked, these interventions have broader implications for improving mood, memory, and cognitive performance.
8. What future technologies could help us monitor cerebellar function in everyday life?
Advancements in wearable neuroscience are making it possible to assess cerebellar activity in real-world settings. Devices that integrate motion capture and biofeedback could soon use data derived from a cerebellum labeled to identify real-time anomalies in balance, coordination, or mood-related physiological signals. Future apps may offer cerebellum diagram overlays that correlate motor irregularities or stress levels with specific cerebellar zones. Such tools could benefit athletes, older adults, or individuals undergoing mental health treatment by flagging subtle changes in neural regulation. These innovations aim to bring cerebellar monitoring out of the lab and into daily routines, empowering users to take proactive steps toward neurological well-being. As the understanding of the small brain deepens, its real-time applications will likely expand dramatically in both clinical and consumer health technologies.
9. How might early-life cerebellar stimulation support healthy brain development?
Stimulating the cerebellum during early development may offer a neuroprotective effect for children at risk of cognitive or emotional disorders. A cerebellum diagram used in pediatric neurology often highlights underdeveloped areas in premature infants or children with neurodevelopmental delays. When the cerebellum is labeled to reflect these gaps, therapies can be directed more precisely. Interventions such as infant massage, rhythmic play, and coordinated crawling exercises have shown the potential to activate cerebellar networks. This small brain responds particularly well to sensorimotor enrichment, which supports not only coordination but also attention and social engagement. Implementing cerebellum-informed early interventions in schools and childcare settings could help reduce the incidence or severity of developmental disorders, creating a stronger foundation for lifelong mental health.
10. Are there lifestyle choices that can strengthen cerebellar health over time?
Absolutely. Although genetics and early development play significant roles, lifestyle choices continue to influence cerebellar health throughout life. Activities that require precise coordination—like martial arts, musical instrument practice, or dance—activate the small brain in ways that promote long-term plasticity. A cerebellum labeled for motor and cognitive areas can guide such activities to ensure balanced stimulation. Nutrition also matters; omega-3 fatty acids, flavonoids, and B vitamins support neurogenesis and mitochondrial efficiency in cerebellar cells. Additionally, stress management practices such as meditation and deep breathing help regulate the autonomic feedback loops mediated by the cerebellum. When combined with regular physical and cognitive engagement, these strategies can preserve cerebellar integrity and enhance emotional resilience well into older adulthood.
Conclusion: Embracing the Cerebellum’s Full Potential for Mental Health and Wellness
The cerebellum, long relegated to the background of neuroscience and psychiatry, is now emerging as a key player in the orchestration of mental health. Once known primarily for its role in coordinating physical movement, this small brain has proven to be deeply involved in emotional regulation, cognitive function, and even social behavior. Its intricate neural networks, dense connectivity, and remarkable plasticity make it a potent influence on mental wellness across the lifespan. A well-crafted and thoroughly labeled cerebellum diagram serves as more than just an educational tool; it is a bridge between clinical practice and neuroscience research, illuminating pathways that are vital for both diagnosis and healing.
The integration of cerebellar analysis into mental health care represents not just a shift in focus but a deepening of our understanding of the human mind. By acknowledging the cerebellum’s contributions, we open the door to more precise diagnostics, more effective therapies, and a more holistic view of what it means to be mentally well. Whether through advanced imaging, neurostimulation, or lifestyle-based interventions, the potential to support mental health by engaging the cerebellum is both scientifically grounded and clinically promising. As we continue to decode the mysteries of this small brain, we must embrace its role not as a mere supporting actor but as a central figure in the complex drama of human psychology. With every cerebellum labeled clearly and each diagram studied carefully, we take one step closer to understanding the profound influence this structure exerts on our mental and emotional lives.
Further Reading:
The big role of the ‘little brain’: exploring the developing cerebellum and its role in cognition