Understanding Carpal Tunnel Syndrome and the Role of Movement-Based Therapies
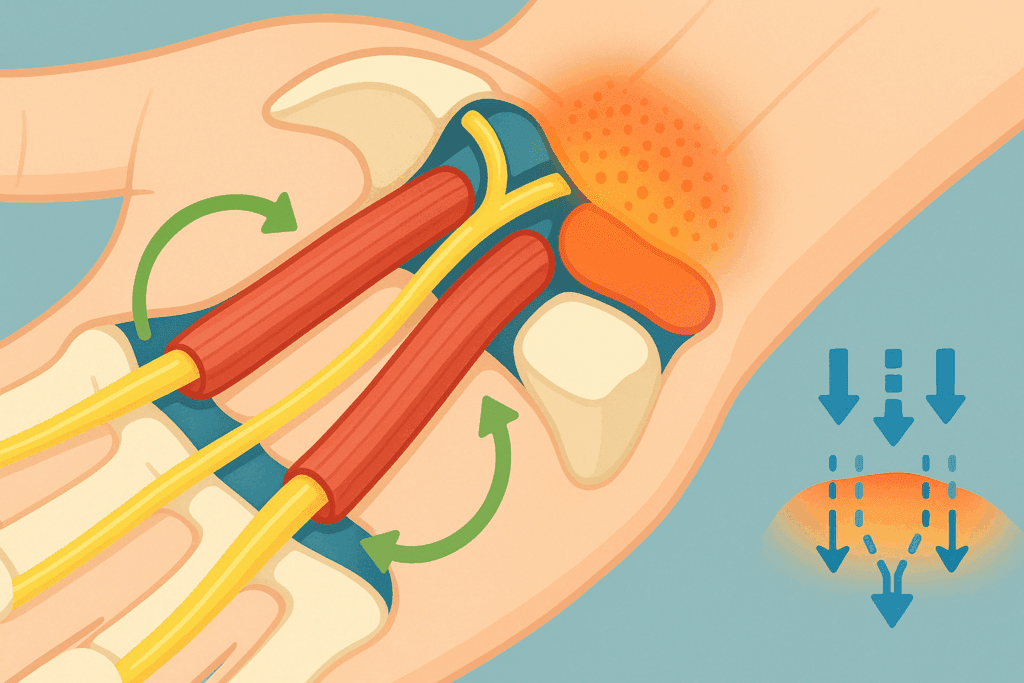
Carpal Tunnel Syndrome (CTS) is one of the most common peripheral nerve entrapments, affecting millions worldwide, particularly individuals who engage in repetitive hand movements. This condition occurs when the median nerve, which runs from the forearm into the hand through the carpal tunnel in the wrist, becomes compressed. The resulting symptoms—including numbness, tingling, pain, and weakness—can significantly impair daily activities and quality of life. What often goes unrecognized is how powerfully structured exercises can influence symptom relief and even contribute to long-term recovery. Among the most effective approaches are carpal tunnel tendon glides and median nerve stretching exercises, which directly target the mechanical and functional restrictions within the wrist and forearm.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Unlike passive treatments that simply address symptoms, these movement-based therapies operate at the intersection of anatomy and function. By deliberately mobilizing the tendons and nerves affected by CTS, patients can reduce intraneural pressure, improve circulation, and restore flexibility. In recent years, clinicians and rehabilitation specialists have increasingly emphasized these techniques not only as supportive but also as primary interventions, especially for individuals with mild to moderate CTS. When practiced regularly and with proper form, tendon glides for carpal tunnel syndrome and targeted nerve exercises can become cornerstones of conservative treatment strategies.

Why Tendon Glides Matter in Managing Carpal Tunnel Syndrome
Tendon gliding exercises are designed to help the flexor tendons of the hand move smoothly through the carpal tunnel. These tendons run alongside the median nerve and can become restricted due to inflammation, fibrosis, or repetitive strain. Over time, limited tendon mobility can exacerbate median nerve compression, increasing symptom severity. Carpal tunnel tendon glides aim to prevent this scenario by promoting differential motion between the tendons and surrounding structures. The term “glide” refers to the sliding of tendons within their sheaths—a natural motion that, when restricted, contributes to stiffness and dysfunction.
When tendon glides are performed correctly, they help break up minor adhesions and encourage fluid movement within the carpal tunnel. This dynamic activity improves synovial fluid distribution, which nourishes the tendons and reduces friction. Additionally, tendon glides reduce swelling by encouraging lymphatic drainage and venous return, both of which are crucial in managing inflammation. For those experiencing early signs of CTS, such as nighttime numbness or mild hand fatigue, incorporating tendon gliding sequences into their daily routine may significantly delay the progression of symptoms.
Proper execution is key. Exercises typically involve moving the fingers through a series of coordinated positions, including straight hand, hook fist, full fist, and tabletop postures. Each movement isolates different tendons while maintaining wrist neutrality, which minimizes strain. Research suggests that individuals who perform tendon glides consistently, under professional guidance, experience a noticeable reduction in pain and improved hand function. Moreover, these exercises are low-impact, making them safe for older adults or those recovering from acute flare-ups.

Integrating Proximal Nerve Mobilization for Full-Chain Relief
Most discussions around CTS focus on the wrist and hand, but the median nerve originates from the brachial plexus, which stems from the cervical spine. This anatomical continuity means that median nerve tension or compression can also occur along the neck, shoulder, or upper arm. Proximal nerve mobilization techniques, therefore, can significantly enhance outcomes when combined with wrist-specific exercises. For instance, cervical lateral glides and shoulder girdle mobilization can reduce neural tension and improve nerve root health, facilitating better nerve conduction downstream.
This full-chain approach is particularly useful in individuals who present with overlapping symptoms of thoracic outlet syndrome or cervical radiculopathy. For them, treating only the wrist may yield suboptimal outcomes. A trained physical therapist might include nerve sliders that incorporate head movement, scapular positioning, and controlled shoulder abduction to create a global neuromobilization effect. These exercises help restore the dynamic adaptability of the entire median nerve pathway and may improve results more dramatically than isolated wrist-focused techniques alone.
Addressing Fascial Restrictions and Myofascial Adhesions
While tendon glides target mechanical mobility within tendon sheaths, soft tissue restrictions in the surrounding fascia can also contribute to movement limitation and nerve entrapment. Myofascial adhesions—dense, fibrotic patches within the connective tissue network—can impede neural mobility and compress soft tissues. Fascial release techniques, whether manual (as performed by therapists) or through self-myofascial tools like massage balls and rollers, can enhance mobility and reduce inflammation.
Recent studies in fascial science underscore the role of interstitial fluid dynamics and mechanotransduction in musculoskeletal health. This means that even minor restrictions in the fascial web can influence nerve function and pain perception. Addressing these areas through targeted fascial stretching, cupping therapy, or instrument-assisted soft tissue mobilization (IASTM) has shown promise in relieving chronic CTS symptoms. For example, the forearm’s flexor compartment often becomes tight in office workers and typists, and releasing this area can provide immediate symptomatic relief.

Exploring Median Nerve Stretching Exercises: Principles and Techniques
Median nerve exercises are designed to restore normal neural mobility and reduce nerve sensitivity within the carpal tunnel. When the median nerve is compressed, it loses its ability to glide freely through surrounding tissues. This restriction leads not only to pain and paresthesia but also to a phenomenon known as neurodynamic dysfunction. Median nerve stretching exercises aim to re-establish the nerve’s physiological motion, relieve tension, and ultimately decrease irritability.
The foundation of these exercises lies in neurodynamics—a therapeutic concept that involves the mechanical and physiological properties of nerves. Unlike static stretches that elongate muscles, median nerve exercises often incorporate gentle, rhythmic motions to coax the nerve back into healthy gliding patterns. For example, the widely recommended “median nerve slider” involves shoulder abduction, wrist extension, and finger extension while keeping the elbow flexed and then gradually extended. This movement sequence allows for controlled loading and unloading of the nerve without causing overstretching or further irritation.
These exercises should be performed with precision, ideally under the supervision of a physical therapist trained in nerve mobilization. If done improperly or too aggressively, there is a risk of aggravating symptoms rather than alleviating them. The key lies in slow progression and sensitivity to bodily feedback. Symptoms such as tingling during movement are acceptable if transient, but persistent discomfort may indicate the need to adjust technique or reduce intensity. Practitioners often recommend performing these exercises multiple times daily, especially during periods of high hand use or after static postures such as typing or driving.
The Science Behind Tendon and Nerve Mobilization
The clinical rationale for tendon glides and median nerve exercises is rooted in both biomechanical and neurophysiological science. When tendons and nerves are repeatedly subjected to stress, they can lose their gliding capacity due to micro-adhesions or inflammation-induced fibrosis. Tendon gliding exercises enhance differential movement between anatomical structures, thereby minimizing friction and pressure buildup. Meanwhile, nerve mobilization techniques work to reduce intraneural edema and improve axonal transport—a critical mechanism for nerve health.
Moreover, recent research has demonstrated that regular mobilization exercises can promote neuroplasticity and pain modulation. This means that not only are physical structures being restored, but the brain’s perception of pain is also being retrained. In chronic cases, where pain persists despite structural healing, such neuroplastic effects are essential for recovery. These insights validate the importance of movement-based therapies as part of a comprehensive CTS management strategy. Furthermore, studies indicate that individuals who engage in structured tendon and nerve exercises are less likely to require surgical intervention.
Beyond symptom control, mobilization exercises help preserve hand dexterity and coordination. This is especially valuable for individuals whose professions depend on fine motor skills—musicians, writers, surgeons, or technicians, for instance. Longitudinal studies have found that consistent performance of median nerve stretching exercises correlates with enhanced grip strength, reduced fatigue, and increased sensory feedback in the hand. These benefits underscore the functional relevance of such exercises in real-world contexts, bridging the gap between rehabilitation and practical application.

Daily Practice: Building an Effective Exercise Routine for Carpal Tunnel Relief
Creating an effective routine for managing CTS involves more than simply learning the movements. It requires a deliberate integration of exercises into daily life, tailored to the individual’s needs and lifestyle. For many, this begins with identifying the optimal time of day to perform tendon glides and median nerve exercises—often in the morning to combat stiffness, and again in the evening to mitigate fatigue from daily activities. A full routine may take just 10 to 15 minutes but should be performed with focused attention and proper technique.
Consistency is the cornerstone of effectiveness. Individuals who practice daily, even during asymptomatic periods, often maintain greater range of motion and experience fewer flare-ups. Combining both tendon glides for carpal tunnel syndrome and median nerve movements into a single session can yield synergistic benefits. For example, starting with tendon glides may help loosen up the wrist and fingers, making subsequent nerve stretches more comfortable and effective. Including gentle warm-ups, such as wrist circles or forearm massages, can further prepare the tissues for movement.
It is also critical to adopt ergonomic modifications alongside exercises. This might involve using a split keyboard, wrist rests, or adjusting workstation height to reduce undue stress on the wrist. While the exercises target internal mobility, external postural changes prevent ongoing aggravation. For individuals with moderate CTS, this dual approach often leads to faster recovery and improved symptom control. Additionally, incorporating mindfulness techniques or breath control during exercises can enhance neuromuscular connection and encourage relaxation, which is particularly helpful for reducing the sympathetic nervous system’s influence on nerve sensitivity.
Common Mistakes and How to Avoid Them
Despite their simplicity, tendon glides and nerve stretches can be rendered ineffective or even harmful when performed incorrectly. One of the most common mistakes is applying excessive force, particularly with nerve mobilizations. The goal is not to stretch the nerve as one would a muscle but to gently encourage motion. Using too much tension can lead to rebound inflammation, increasing discomfort and delaying recovery. It is important to remember that subtlety and consistency often yield better results than intensity.
Another frequent error is neglecting wrist positioning during exercises. Maintaining a neutral wrist is crucial, especially during tendon glides, as flexion or extension can place additional pressure on the carpal tunnel. Many individuals also overlook the importance of pacing and rest between repetitions. Rushing through movements or repeating them too many times without pause can lead to fatigue or tissue irritation. Ideally, exercises should be performed in sets with sufficient recovery between them, allowing tissues to respond and adapt gradually.
Improper sequencing is also a factor. Some practitioners recommend beginning with light aerobic movement or soft tissue massage to warm the area before engaging in more focused mobilization. Skipping this step can make tissues more susceptible to strain. Finally, relying solely on exercises without addressing contributing lifestyle factors—such as poor posture, stress, or inadequate sleep—limits the overall effectiveness of any therapeutic intervention. A truly integrative approach must consider both physical and behavioral contributors to CTS.
How to Know If These Exercises Are Working
Monitoring progress is essential to understanding whether your exercise regimen is effective. Improvement may manifest in various ways, from a reduction in nighttime symptoms to improved grip strength or enhanced tactile sensitivity. Individuals may also notice that activities which previously triggered discomfort—such as holding a phone or using a computer mouse—become more manageable over time. These functional gains are often more telling than subjective pain levels, which can fluctuate for other reasons.
Keeping a symptom journal can be helpful. Recording metrics like duration and intensity of numbness, times of day when symptoms worsen, and how long relief lasts after exercise can provide valuable data. Over weeks or months, patterns emerge that allow for targeted adjustments to the exercise protocol. This kind of self-monitoring also enhances engagement and accountability, encouraging continued practice.
It is equally important to set realistic expectations. While some may experience noticeable improvement within a few days, others may require several weeks of consistent practice before seeing results. This variability is influenced by factors such as severity of CTS, overall health status, and adherence to the routine. Consulting with a healthcare provider or physical therapist can provide reassurance and guidance if progress seems slow. In some cases, they may suggest adjunct therapies such as ultrasound, manual therapy, or bracing to support the exercise regimen.
When to Seek Professional Help
While tendon glides and median nerve exercises are highly effective for many individuals, they are not a panacea. Persistent or worsening symptoms may indicate that more advanced interventions are needed. For example, if there is muscle wasting in the thumb area (thenar eminence), significant loss of hand function, or constant pain unrelieved by rest and exercise, a referral to a specialist is warranted. Electromyography (EMG) or nerve conduction studies can assess the extent of nerve involvement and guide next steps.
In some cases, corticosteroid injections or surgical decompression may be recommended, especially if conservative management fails. Even then, movement-based therapies retain their value. Post-operative rehabilitation often includes the same tendon and nerve gliding techniques to promote recovery and prevent scar tissue formation. Thus, understanding these exercises and how to perform them correctly has long-term relevance, regardless of the treatment pathway.
It is also worth noting that not all wrist or hand pain stems from carpal tunnel syndrome. Conditions such as cervical radiculopathy, pronator teres syndrome, or rheumatoid arthritis can mimic CTS symptoms but require different interventions. This underscores the importance of accurate diagnosis and personalized care. Engaging a physical therapist, occupational therapist, or hand specialist ensures that the chosen exercises align with the individual’s unique condition and goals.

Wearable Technology and Biofeedback Integration
The rise of wearable technology offers new opportunities for optimizing exercise routines. Devices that track range of motion, muscle activation, or grip strength provide real-time feedback and encourage compliance. For instance, smart gloves equipped with sensors can detect wrist angle deviations or insufficient movement quality during tendon glides and median nerve stretches. This data empowers patients to self-correct and track progress quantitatively.
Biofeedback systems, which measure muscle tension or nerve conductivity, can be used in clinical settings to guide relaxation training or improve neuromuscular control. These technologies add a layer of interactivity and personalization to the rehabilitation process, making exercises more engaging and data-driven. In telehealth contexts, such tools also enable therapists to monitor and adjust programs remotely, expanding access to care.
The Future of Conservative CTS Care
Emerging research continues to refine our understanding of nerve mobility, pain modulation, and the psychosomatic dimensions of hand function. Techniques such as virtual reality (VR)-assisted rehabilitation, which immerses patients in interactive environments requiring precise hand movements, are currently being explored for upper extremity disorders. These approaches merge gamification with therapeutic intent, motivating patients to engage more fully in their recovery.
Furthermore, regenerative medicine techniques, including platelet-rich plasma (PRP) injections and stem cell therapies, are being investigated for their potential to repair damaged nerve tissue in chronic CTS. While still experimental, these treatments may one day complement exercise-based approaches and offer hope for individuals with refractory symptoms.
Frequently Asked Questions: Advanced Insights on Tendon Glides and Median Nerve Exercises for Carpal Tunnel Syndrome
1. Can carpal tunnel tendon glides be used preventively, even without symptoms?
Yes, carpal tunnel tendon glides can be beneficial as a preventive measure, especially for individuals whose daily routines involve repetitive wrist and finger use. While most people begin using these exercises only after symptoms arise, incorporating tendon glides into a regular stretching regimen can promote tendon health and reduce the likelihood of inflammation around the median nerve. These movements improve fluid exchange and tendon mobility, keeping soft tissues flexible and resilient. In professions like data entry, playing musical instruments, or laboratory work, early integration of tendon glides for carpal tunnel syndrome can help maintain healthy motion patterns before dysfunction develops. Preventive use of these exercises also encourages better body awareness and reduces the tendency to overload specific muscles and tendons.
2. How do median nerve stretching exercises interact with postural therapy?
While median nerve stretching exercises directly target the nerve’s ability to glide, their effects are amplified when paired with postural therapy that addresses upper body alignment. For example, if forward head posture and rounded shoulders are compressing the brachial plexus, even perfect execution of median nerve exercises may not fully resolve symptoms. Correcting posture through thoracic mobility drills, scapular stabilization, and cervical spine exercises reduces upstream tension that can travel down to the wrist. The synergistic combination of postural correction and median nerve exercises can optimize neural mobility throughout the entire arm. This holistic strategy is particularly valuable in cases where nerve symptoms extend beyond the wrist, such as into the forearm or upper arm.
3. What role does grip strength play in recovery from carpal tunnel syndrome?
Grip strength is both a functional indicator and a therapeutic target in carpal tunnel syndrome rehabilitation. As median nerve function declines, grip strength often suffers due to reduced innervation of the thenar muscles. Median nerve exercises help restore this neuromuscular connection, but strengthening protocols are also necessary to rebuild lost muscle performance. Hand therapy putty, resistance bands, and small hand tools can be used in parallel with carpal tunnel tendon glides to promote coordinated recovery. Importantly, grip strength should be rebuilt gradually, avoiding overexertion that may aggravate nerve compression or inflammation.
4. Can tendon glides for carpal tunnel syndrome benefit patients after surgery? Absolutely. In fact, post-operative rehabilitation protocols often include carpal tunnel tendon glides as a foundational component. After surgical decompression, adhesions and scar tissue can form around the flexor tendons, limiting their ability to glide freely. Tendon glides reduce the risk of this postoperative stiffness while promoting circulation and healing. Additionally, gentle median nerve stretching exercises can restore neural mobility disrupted by surgery or prolonged immobilization. Working with a certified hand therapist ensures that these exercises are introduced at the right intensity and frequency to support safe and effective healing.
5. How can technology enhance the precision of median nerve exercises?
Emerging technologies, such as wearable motion trackers and biofeedback gloves, are being integrated into physical therapy to provide real-time data on joint angles and nerve excursion. These tools help patients maintain optimal alignment during median nerve exercises and avoid compensatory movements. For instance, a sensor-equipped glove can alert a user when wrist extension surpasses a safe range, protecting the nerve from overstretching. Using technology in this way enhances the quality of carpal tunnel tendon glides and related nerve stretches by improving consistency and precision. Such tools are particularly helpful for home-based rehab, where access to in-person supervision may be limited.
6. Are there psychological factors that influence the effectiveness of tendon glides?
Yes, psychological variables like stress, fear of movement, and perceived control over symptoms can greatly influence how effective tendon glides for carpal tunnel syndrome are. Chronic stress increases muscle tension and systemic inflammation, which may exacerbate nerve compression. Patients who engage in mindfulness techniques while performing exercises often report better outcomes, likely due to reduced sympathetic nervous system activity. Incorporating breath work or meditative awareness into a tendon gliding session can deepen relaxation and enhance neuromuscular control. Moreover, cultivating a sense of agency over the recovery process helps counteract helplessness or avoidance behaviors that may worsen symptoms.
7. How do carpal tunnel tendon glides differ from general finger stretches?
While general finger stretches often aim to lengthen soft tissues, carpal tunnel tendon glides are designed to promote the differential movement of tendons within their synovial sheaths. This specificity is crucial for maintaining the health of tendons that share the confined space of the carpal tunnel with the median nerve. Unlike passive stretches, tendon glides involve active, sequenced finger movements that target distinct anatomical pathways. They are biomechanically strategic, enhancing mobility without overloading the nerve. Median nerve stretching exercises may be paired with tendon glides for an integrated approach, but each serves a unique role in managing CTS symptoms.
8. What are the risks of doing median nerve exercises incorrectly?
Improper execution of median nerve stretching exercises can actually increase discomfort and potentially worsen nerve irritation. Overstretching the nerve or performing the movements too quickly can provoke inflammation or exacerbate symptoms like tingling and burning. Without appropriate supervision, individuals might also adopt compensatory postures that increase tension elsewhere, such as the neck or shoulder. For example, shoulder elevation during a nerve glide can diminish its effectiveness and add strain to the upper trapezius. Working with a therapist initially can help individuals internalize safe movement patterns and tailor the exercise to their sensitivity level.
9. Can tendon glides for carpal tunnel syndrome be adapted for people with arthritis? Yes, though with certain modifications. Individuals with coexisting arthritis may have joint stiffness or swelling that limits range of motion, making traditional tendon glides challenging. In such cases, shorter ranges, slower pacing, and extended warm-ups can help reduce joint stress. Moist heat packs or paraffin wax baths before performing the exercises can enhance comfort and tissue pliability. Median nerve exercises may also need to be modified to avoid wrist positions that trigger arthritic pain. Collaboration with a hand therapist ensures that both carpal tunnel and arthritis concerns are addressed harmoniously within a personalized plan.
10. How do occupational tasks influence the long-term success of tendon and nerve exercises?
The long-term success of carpal tunnel tendon glides and median nerve stretching exercises depends heavily on modifying occupational risk factors. If someone continues repetitive tasks without adjusting ergonomics, the benefits of these exercises may be limited. For instance, assembly line workers or dental hygienists may require customized rest breaks, assistive tools, or alternative task rotations to protect their wrists. Integrating exercises into the workday—for example, performing tendon glides during short pauses—can sustain mobility and reduce flare-ups. The most effective outcomes occur when individuals combine consistent exercise with proactive changes to their work environment, ensuring that therapeutic gains are preserved and reinforced.
Conclusion: Reclaiming Function with Evidence-Based Carpal Tunnel Relief Strategies
Tendon glides and median nerve exercises represent a clinically grounded, non-invasive approach to addressing the challenges of carpal tunnel syndrome. When performed consistently and correctly, these techniques improve tendon mobility, enhance nerve function, and reduce discomfort, often making the difference between chronic impairment and functional independence. The science supporting tendon glides for carpal tunnel syndrome and median nerve stretching exercises is both robust and evolving, with ongoing research continuing to refine their application.
These exercises empower individuals to take an active role in their recovery, promoting body awareness and self-efficacy. They are not merely symptomatic treatments but tools for restoring harmony between the structures of the hand, wrist, and forearm. Whether used as preventive measures, early interventions, or post-surgical rehabilitation strategies, carpal tunnel tendon glides and median nerve exercises have earned their place as foundational components in the modern management of CTS.
In embracing these expert-recommended stretches for flexibility and recovery, individuals can reclaim not just mobility, but confidence in their ability to heal. By integrating movement with mindfulness, education with execution, and precision with patience, the path to relief becomes not just possible, but sustainable. For those navigating the complexities of carpal tunnel syndrome, this evidence-based, movement-oriented strategy offers a safe, effective, and empowering way forward.
Further Reading:
Carpal Tunnel Median Nerve Gliding Exercises


