As cannabis use becomes increasingly mainstream, questions about its effects on aging brains have taken center stage in public health discourse. Among these concerns is the relationship between cannabis, particularly its psychoactive component THC (tetrahydrocannabinol), and dementia. The complex nature of neurodegenerative diseases such as Alzheimer’s, vascular dementia, and Lewy body dementia makes it crucial to evaluate whether cannabis compounds offer neuroprotective benefits or pose risks for cognitive deterioration. For families caring for aging loved ones and older adults seeking symptom relief, the question looms large: can cannabis help dementia, or can cannabis cause dementia instead?
The rise of medical marijuana has prompted researchers to study its potential impact on cognitive health with renewed urgency. While early anecdotal evidence hinted at calming effects in patients exhibiting aggression or pacing behaviors, such as those with Alzheimer’s disease, robust clinical trials remain sparse. At the same time, some epidemiological studies suggest that frequent cannabis use may be associated with impaired cognition, raising concerns over long-term safety. In exploring the intersection of cannabis and brain health, we must weigh evidence from laboratory studies, clinical observations, and large-scale population research. With a growing senior population turning to cannabis for everything from pain management to mood stabilization, understanding the implications of marijuana use and dementia is now more important than ever.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
How THC Interacts with the Aging Brain
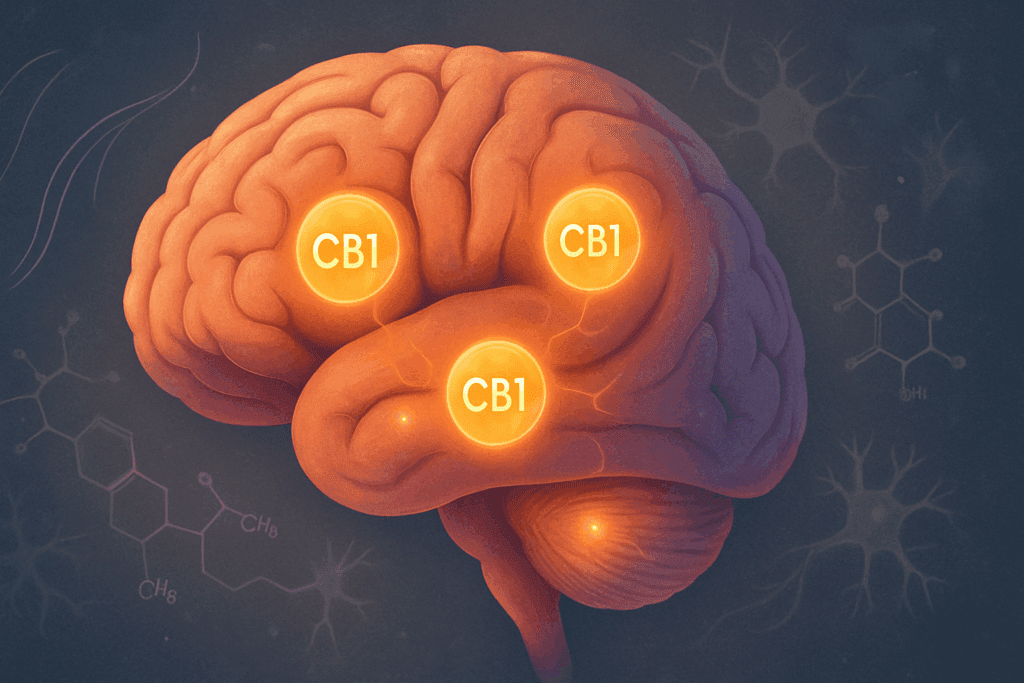
Tetrahydrocannabinol (THC), the main psychoactive ingredient in cannabis, exerts its effects by binding to cannabinoid receptors in the brain—primarily CB1 receptors, which are densely concentrated in areas responsible for memory, decision-making, and emotional regulation. As people age, changes in these brain regions often occur naturally, making them potentially more vulnerable to external influences. This raises an essential question: is marijuana good for dementia, or could its effects exacerbate age-related cognitive decline?
Laboratory studies have shown that low doses of THC may have anti-inflammatory and antioxidant effects that could, theoretically, protect neurons from degeneration. For example, animal studies suggest that THC may help clear beta-amyloid plaques, one of the hallmarks of Alzheimer’s pathology. However, dosage appears to be a critical factor. While minimal THC exposure might support neural resilience, higher doses can impair short-term memory, reduce executive functioning, and alter mood—effects that could worsen dementia symptoms rather than alleviate them.
It is also worth noting that the aging brain may metabolize THC differently than that of younger individuals, potentially leading to prolonged psychoactive effects and heightened risk for disorientation or paranoia. In this context, the question “does cannabis cause dementia” is far from simple. Rather, the answer may depend on variables such as dosage, frequency of use, the specific dementia subtype, and the individual’s overall health profile.
Can THC Alleviate Behavioral Symptoms in Dementia?
Among caregivers and clinicians, there has been growing interest in whether THC can ease some of the most challenging behavioral symptoms in dementia patients. These include agitation, aggression, wandering, and repetitive pacing. Anecdotal reports and small pilot studies suggest that certain cannabis formulations may reduce these behaviors without the sedative effects typically seen with traditional antipsychotic medications. The concept of using THC for pacing and Alzheimer’s-related restlessness has gained traction, especially among those seeking alternatives to conventional pharmacological treatments.
Despite the growing popularity of cannabis-based interventions, scientific evidence remains limited. A few studies have explored synthetic cannabinoids such as dronabinol, finding some benefit in reducing agitation and promoting weight gain in patients with moderate to severe Alzheimer’s disease. However, these studies often suffer from small sample sizes, short duration, and methodological inconsistencies. As such, while preliminary findings suggest potential benefits, they are not yet robust enough to support widespread clinical use.
Still, the appeal of cannabis as a behavioral management tool in dementia care is understandable. Many families struggle with the emotional and logistical challenges posed by aggressive or wandering behavior. If cannabis-derived compounds can offer relief without the harsh side effects associated with antipsychotics or benzodiazepines, they warrant further investigation. However, given the paucity of conclusive data, clinicians must tread carefully, weighing both risks and benefits for each individual.
Exploring the Risks: Can Marijuana Cause Dementia?
While the therapeutic promise of cannabis has received considerable attention, there are also important concerns about its long-term effects on brain health. One of the most pressing questions is whether marijuana use and dementia are linked in a causative way. More specifically, does smoking weed cause dementia, or is the association merely correlative?
Some longitudinal studies have found that chronic cannabis use, particularly when started early in life and maintained into middle age, is associated with cognitive deficits in later years. These include impairments in attention, memory, and processing speed—functions that are often affected in dementia. A 2021 study published in The Journal of the American Medical Association found that persistent marijuana use was correlated with reduced cognitive performance over time, even after controlling for other variables such as education level and co-occurring substance use.
However, the issue is complicated by several confounding factors. For instance, cannabis users may also engage in other behaviors that independently increase dementia risk, such as tobacco smoking, sedentary lifestyle, or poor diet. Moreover, some studies have failed to find a significant association between cannabis use and later-life cognitive decline, suggesting that moderate or occasional use may not carry the same risks as chronic, heavy consumption. Nonetheless, the potential for THC to disrupt memory formation and executive functioning remains a concern, particularly in older adults with preexisting vulnerabilities.

Evaluating the Safety and Efficacy of Edibles in Dementia Care
As smoking cannabis can pose respiratory risks, especially in older adults with pulmonary conditions, many individuals exploring medical marijuana turn to edibles as an alternative. But this raises new questions: can edibles help dementia, and are they safe for older adults with cognitive impairments? The appeal of edibles lies in their ease of dosing and long-lasting effects, which may help stabilize mood and reduce behavioral volatility.
However, edibles also present unique challenges. First, they are metabolized through the liver, resulting in a delayed onset of action that can range from 30 minutes to two hours. This lag increases the risk of accidental overconsumption, especially in individuals with memory problems who may forget they have already taken a dose. Additionally, the effects of edibles can last much longer than those of inhaled cannabis, potentially leading to prolonged sedation, confusion, or even hallucinations in vulnerable individuals.
Still, when carefully dosed and monitored, some caregivers report that edibles offer a gentler, more predictable experience for patients experiencing agitation or insomnia. The best edibles for dementia patients are typically those with low THC concentrations, sometimes combined with cannabidiol (CBD), which may counteract some of THC’s psychoactive effects. Clinical trials evaluating these products are still in their early stages, but early findings suggest potential as part of a broader, multidisciplinary care plan.
Parsing the Evidence: Can Cannabis Help Dementia?
The idea that cannabis could offer therapeutic benefits for dementia patients is deeply compelling, especially in the face of limited pharmaceutical options. So, can cannabis help dementia? The answer appears to depend on how we define “help” and which aspects of dementia we are targeting. If the goal is to slow disease progression, the evidence is currently insufficient to make a strong claim. No large-scale randomized controlled trials have conclusively shown that cannabis halts or reverses the underlying pathology of neurodegenerative diseases.
However, if the goal is symptom management—reducing anxiety, aggression, sleeplessness, or appetite loss—then cannabis may offer some promise. In these cases, the focus shifts from disease modification to quality-of-life improvement. Anecdotal reports from caregivers and small observational studies have found that cannabis-based interventions may help some individuals feel calmer, sleep better, and engage more positively with their environment.
It is crucial to remember that cannabis is not a one-size-fits-all remedy. The diversity of cannabis strains, THC:CBD ratios, and modes of administration means that individual responses can vary widely. Moreover, dementia itself is not a single disease but a constellation of syndromes, each with distinct underlying mechanisms. What may help a person with Alzheimer’s might not benefit someone with Lewy body dementia, and vice versa. Thus, personalized approaches grounded in careful assessment and clinical oversight are essential.
Clarifying the Role of CBD and Other Cannabinoids
Although THC garners much of the spotlight, it is only one of more than a hundred cannabinoids present in cannabis. Cannabidiol (CBD), a non-intoxicating compound, has emerged as a promising agent for reducing anxiety, inflammation, and oxidative stress—all factors that may contribute to cognitive decline. Unlike THC, CBD does not produce a “high,” making it potentially safer and more acceptable for use in elderly populations.
Some researchers have explored whether combinations of THC and CBD could offer synergistic benefits. For example, a balanced ratio might allow for symptom relief with fewer side effects than THC alone. However, the evidence remains preliminary. Few studies have directly compared the effects of different cannabinoid profiles in dementia patients, and most clinical trials to date have focused on synthetic or isolated compounds rather than whole-plant formulations.
Understanding the full therapeutic potential of cannabis requires a deeper dive into the roles of lesser-known cannabinoids such as cannabigerol (CBG) and cannabinol (CBN). These compounds are believed to influence neuroinflammation and neurotransmitter function, though human data is still lacking. As the scientific community begins to explore these avenues, the hope is that targeted cannabinoid therapies may eventually be developed to support cognitive health more precisely and effectively.
Navigating Legal, Ethical, and Caregiving Considerations
The question of whether cannabis can help dementia or cause harm is not only scientific but also ethical and practical. In the United States, cannabis remains a Schedule I substance at the federal level, although many states have legalized its medical or recreational use. This legal patchwork creates confusion for caregivers, healthcare providers, and patients trying to make informed decisions.
Ethically, the use of cannabis in dementia care presents dilemmas around consent, autonomy, and safety. Patients with advanced cognitive impairment may not be able to provide informed consent, raising questions about who should make treatment decisions and how risks should be communicated. Caregivers must also consider how cannabis use might interact with other medications or exacerbate psychiatric symptoms such as delusions or paranoia.
From a practical standpoint, implementing cannabis into a dementia care plan requires attention to dosing, product quality, and ongoing monitoring. It also requires open communication between patients, families, and clinicians. Despite these challenges, the growing acceptance of medical cannabis suggests a paradigm shift in how we approach symptom management in neurodegenerative diseases.
Weed and Dementia: A Nuanced Relationship
To fully appreciate the implications of weed and dementia, we must move beyond simplistic narratives that frame cannabis as either a miracle cure or a dangerous gateway drug. The reality is far more nuanced. While the question “can marijuana cause dementia” remains unresolved, current evidence suggests that moderate, well-controlled use may offer benefits for certain behavioral symptoms, particularly when conventional treatments have failed.
At the same time, caution is warranted. The effects of cannabis on the aging brain are not yet fully understood, and vulnerable populations may be more susceptible to adverse outcomes. It is also important to distinguish between recreational use and medically supervised interventions, as the former often involves higher THC concentrations and less precise dosing.
Education, clinical oversight, and individualized treatment plans are critical for ensuring that cannabis is used safely and effectively in dementia care. Ongoing research will hopefully provide clearer guidance in the years ahead, helping caregivers and clinicians navigate this complex terrain with confidence and compassion.
What the Future Holds for Cannabis-Based Dementia Therapies
As interest in cannabis and cognitive health continues to grow, so does the need for rigorous, well-designed research. Clinical trials examining different formulations, dosages, and delivery methods are currently underway in various countries. These studies aim to answer essential questions such as: Which cannabinoids are most effective? What are the optimal THC:CBD ratios for different dementia types? How can we minimize risks while maximizing therapeutic benefits?
Advancements in neuroimaging and biomarker development may also pave the way for more targeted cannabis therapies. For example, researchers are exploring whether PET scans can detect early changes in brain activity following cannabinoid treatment, providing real-time insights into efficacy and safety. Such tools could revolutionize the way we evaluate cannabis-based interventions, transforming anecdotal evidence into actionable clinical strategies.
In addition, growing public support for cannabis legalization may accelerate funding for research and foster collaboration between academic institutions, pharmaceutical companies, and government agencies. As barriers to cannabis research gradually fall, the scientific community is poised to develop a more nuanced understanding of its role in dementia care.
Frequently Asked Questions: Cannabis and Dementia
1. Can cannabis slow the progression of dementia, or does it only manage symptoms?
Current scientific understanding suggests that cannabis may offer symptom management but does not definitively slow the progression of dementia. While some cannabinoids show potential in laboratory models for reducing inflammation and oxidative stress, human clinical trials have yet to confirm any long-term neuroprotective effects. Thus far, the most consistent benefits of cannabis have been related to behavioral symptom relief, such as managing agitation or improving appetite. Questions like “can cannabis help dementia” often refer to its short-term impact on quality of life rather than its ability to alter the disease trajectory. Ongoing trials may one day clarify whether cannabis can modify the course of neurodegeneration, but for now, its role remains primarily palliative.
2. Are THC-based treatments safe for long-term use in older adults with dementia?
The long-term safety profile of THC in older adults with cognitive impairment is still under investigation. While low doses may provide relief from behavioral disturbances, repeated or prolonged exposure to THC could pose risks, especially when combined with polypharmacy, which is common in geriatric patients. When assessing the relationship between THC and dementia, physicians must consider factors such as liver function, drug interactions, and metabolic rate, which change with age. There’s also concern that overuse could worsen confusion or lead to increased fall risk in frail individuals. Therefore, any long-term use of THC for dementia should involve close medical supervision and periodic reevaluation of benefits versus side effects.
3. What role does cannabis play in reducing caregiver stress for dementia patients?
One often overlooked aspect of the cannabis-dementia discussion is its impact on caregiver burden. In families where dementia symptoms are severe and disruptive, cannabis may reduce the intensity of behavioral episodes, indirectly easing caregiver stress. For example, THC for pacing and Alzheimer’s symptoms like agitation may offer some relief that allows for more manageable daily routines. While this does not directly prove that cannabis treats the underlying disease, its role in enhancing the caregiving experience deserves more research. This perspective is essential in evaluating whether weed and dementia can coexist in a supportive, ethical care model that acknowledges both patient and caregiver needs.
4. How do cannabinoid delivery methods affect therapeutic outcomes in dementia care?
Different delivery systems significantly influence how cannabinoids affect individuals with dementia. Inhalation methods offer rapid relief but may irritate the lungs, while edibles offer longer-lasting effects but come with delayed onset and unpredictable absorption. This variability is important when considering whether cannabis is good for dementia patients whose symptoms fluctuate or whose routines are sensitive to timing. Many clinicians argue that the best edibles for dementia patients are those with consistent THC:CBD ratios and easy-to-administer formats, such as gummies or tinctures. Ultimately, delivery method impacts not just effectiveness but also safety and quality of life, particularly for patients with swallowing difficulties or erratic appetites.
5. What are the legal and ethical concerns with using cannabis for dementia?
Cannabis legality varies by state and country, complicating its integration into dementia care. Additionally, ethical issues arise when patients cannot provide informed consent. When evaluating whether to use cannabis, caregivers must ask not just “can cannabis help dementia?” but also “should it be used in this context?” Informed consent, supervision, and monitoring are crucial in avoiding potential misuse or harm. These concerns intensify when asking questions like “can cannabis cause dementia” if used inappropriately, especially without medical oversight. Navigating these challenges requires collaboration between legal advisors, physicians, and family members.
6. Are there early indicators that cannabis might be causing harm in dementia patients?
Recognizing early signs of cannabis-related complications is key to preventing harm. Symptoms such as increased confusion, paranoia, sleep disturbances, or mood swings may indicate that cannabis is not well-tolerated. When asking, “does cannabis cause dementia or just exacerbate existing issues?” these red flags should be considered. In some cases, caregivers mistake cannabis-induced cognitive changes for disease progression, which can delay proper treatment adjustments. These subtle cues reinforce the need for personalized care plans and continual observation when incorporating cannabis into dementia protocols.
7. Is there evidence that marijuana use earlier in life contributes to dementia later on?
Studies exploring the long-term cognitive effects of marijuana suggest that heavy use beginning in adolescence may be linked to later-life cognitive impairment. While correlation does not prove causation, the question “can marijuana cause dementia” remains central to public health policy. A lifetime of marijuana use and dementia risk might share confounding factors such as socioeconomic status, mental health, or substance use. That said, most experts agree that occasional or medically supervised use in adulthood is less likely to be harmful than habitual use from a young age. These nuances are critical in interpreting studies that examine whether weed and dementia are related over decades.
8. Can cannabis be used in combination with conventional dementia medications?
There is emerging interest in combining cannabis with standard dementia medications, but research in this area is still in its infancy. Preliminary observations suggest that cannabinoids may complement certain treatments by reducing agitation without interfering with drugs like donepezil or memantine. However, clinicians must monitor for drug interactions, especially with medications metabolized through the liver. When asking, “does pot help dementia in conjunction with traditional therapies?” the answer lies in carefully tailored regimens rather than blanket recommendations. Integrated approaches may yield new opportunities for comprehensive care if validated through future studies.
9. What makes certain edibles more appropriate for dementia care than others?
The best edibles for dementia patients are those that offer low THC doses, predictable absorption, and minimal psychoactive effects. Products with balanced THC:CBD ratios tend to be better tolerated and pose fewer cognitive side effects. This makes them more suitable in answering the question, “can edibles help dementia without worsening symptoms?” Additionally, the texture and ease of ingestion matter, as some dementia patients experience swallowing difficulties. Flavor and palatability also play a role in adherence, especially in populations with diminished appetite or taste changes. All these factors determine whether edibles enhance or hinder quality of life in a dementia care setting.
10. How should families approach the decision to try cannabis for dementia treatment?
Families considering cannabis must start with open conversations involving the patient’s healthcare team. The question isn’t just “can cannabis help dementia,” but also whether it fits into the person’s broader care philosophy and goals. Clinicians should evaluate risks, consider drug interactions, and propose a structured plan with dosage guidelines and outcome tracking. Concerns like “does smoking weed cause dementia” or “is marijuana is good dementia therapy” should be explored with evidence, not assumptions. When handled thoughtfully, cannabis may offer compassionate, individualized relief that aligns with both medical insight and the patient’s lived experience.
Final Reflections: Balancing Hope and Caution in the Cannabis-Dementia Debate
In the search for innovative solutions to one of the most pressing public health challenges of our time, cannabis has emerged as both a beacon of hope and a source of controversy. The question of whether cannabis can help dementia or cause harm does not lend itself to easy answers. Instead, it demands thoughtful exploration, grounded in scientific evidence and guided by ethical considerations.
For now, cannabis remains a potential tool—not a panacea—for managing certain symptoms of dementia. It may offer relief for behaviors that strain caregivers and diminish quality of life, such as agitation or insomnia. But its use must be carefully tailored, continuously evaluated, and integrated within a broader, person-centered approach to care.
As researchers continue to investigate marijuana use and dementia, a more detailed picture will emerge. Until then, the guiding principle must be one of cautious optimism: embracing the therapeutic potential of cannabis while remaining vigilant to its risks. Whether considering THC for pacing and Alzheimer’s behaviors, exploring the best edibles for dementia patients, or simply asking, “does pot help dementia?” the answer must be informed, individualized, and rooted in both compassion and science.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Cannabis use and cognitive dysfunction
A Systematic Review of the Neurocognitive Effects of Cannabis Use in Older Adults
Can Cannabis Treat or Cause Dementia?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While Health11News strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. Health11News, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of Health11News.