Introduction: Why the Layers of the Brain Matter for Mental Health
Understanding how the human brain functions requires us to look beyond the neurons and neurotransmitters often spotlighted in neuroscience discussions. One of the most overlooked yet profoundly vital aspects of brain health is the physical structure that encases and protects it: the brain coverings. Often referred to as the 3 layers of the brain, these protective membranes—scientifically known as the meninges—play a central role not just in shielding the brain from injury but also in supporting mental and cognitive well-being. In the era of increased awareness around mental health, delving into the physical mechanisms that influence brain function helps deepen our understanding of holistic wellness.
Though these layers may not be as widely discussed as brain regions like the prefrontal cortex or the amygdala, their significance is foundational. Every brain layer contributes to the overall health of the central nervous system in ways that influence everything from neuroinflammation to cerebrospinal fluid dynamics. Recognizing the importance of each brain covering—dura mater, arachnoid mater, and pia mater—can offer us new insights into how our brain remains resilient against physical trauma and neurological disease. As science continues to explore the intersections of anatomy, physiology, and psychology, the protective function of these coverings is being increasingly linked to the long-term preservation of mental clarity, emotional balance, and cognitive strength. Furthermore, examining the layers of brain protection reveals how seemingly physical components of the brain are deeply connected to psychological states and mental wellness outcomes.
You may also like: Boost Brain Power Naturally: Evidence-Based Cognitive Training Activities and Memory Exercises That Support Long-Term Mental Health
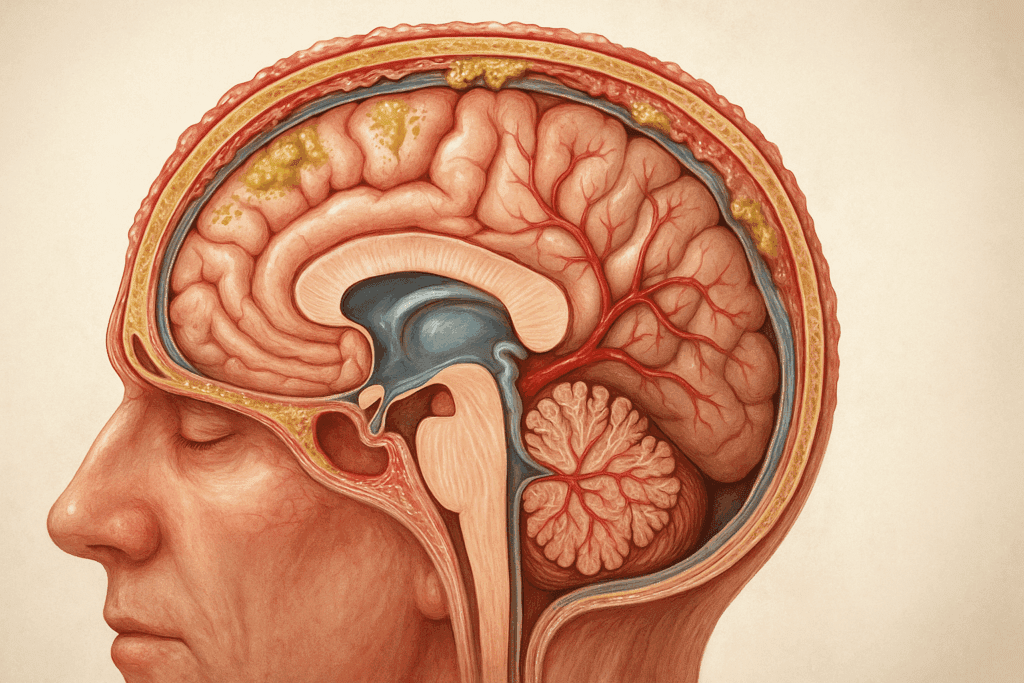
The Dura Mater: The Outer Shield of the Brain
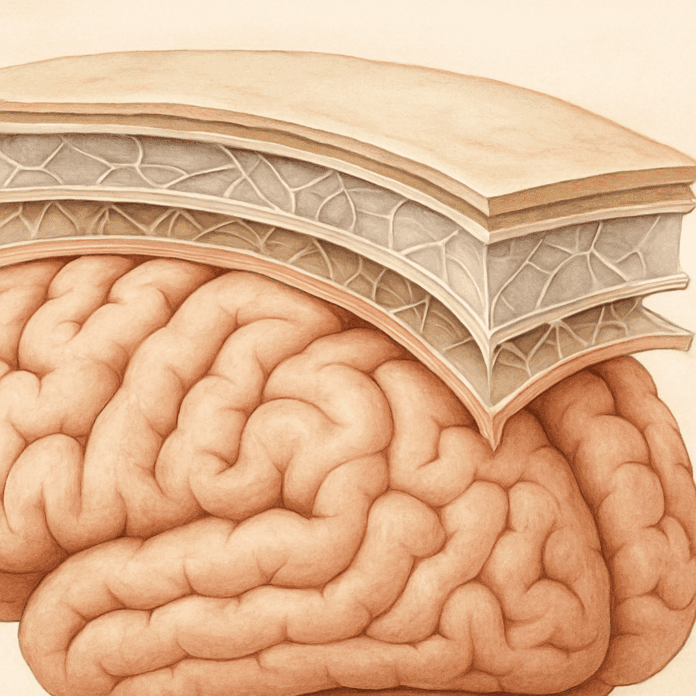
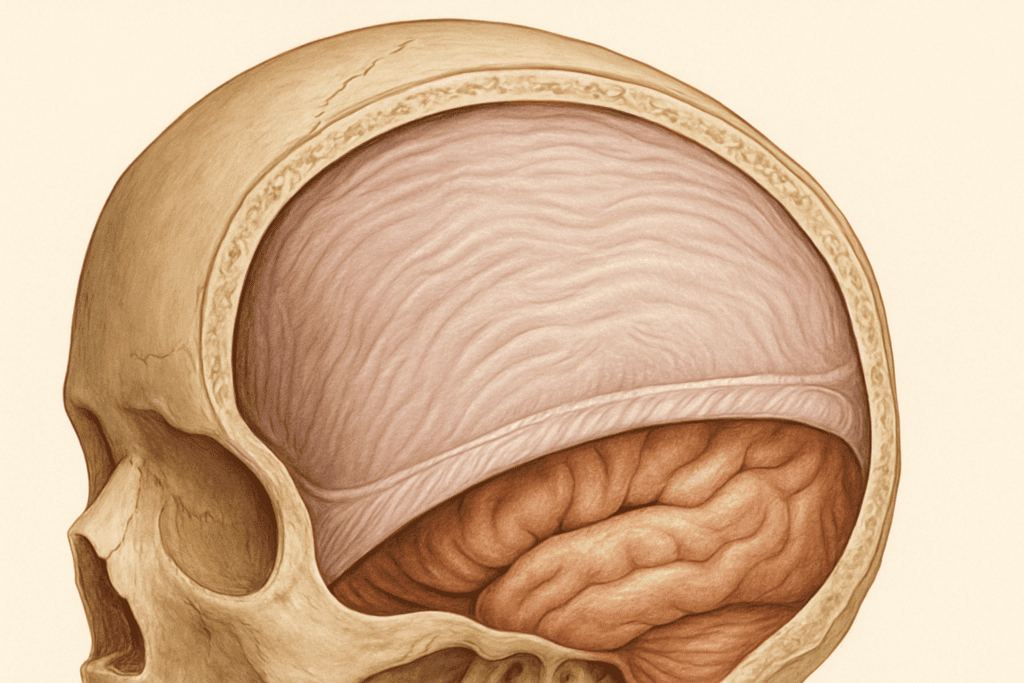
The outermost of the 3 layers of the brain, the dura mater, serves as a formidable protective barrier. Aptly named from the Latin for “tough mother,” the dura mater is a thick, durable membrane that lies just beneath the skull. Its primary role is to act as a physical shield, defending the brain from mechanical injury such as blunt force trauma. Yet its function goes far beyond simple structural support. This brain layer is intimately involved in maintaining the overall homeostasis of the intracranial environment.
In addition to its protective function, the dura mater plays a crucial role in venous blood drainage. It contains dural sinuses, which are channels that drain blood from the brain and return it to the heart. This ensures that blood circulation within the brain remains efficient and uninterrupted—a vital factor for cognitive function and emotional regulation. When blood flow is compromised, symptoms such as brain fog, confusion, and mood disturbances often follow, highlighting the dura mater’s indirect yet significant impact on mental health.
Another lesser-known but increasingly studied aspect of the dura mater involves its role in neuroimmune interaction. Recent research suggests that immune cells residing in or near this brain covering can influence inflammation levels within the central nervous system. Because chronic neuroinflammation has been implicated in a wide range of mental health disorders—from depression to schizophrenia—the dura mater may hold more importance in mental wellness than traditionally thought. These insights underscore the need to explore brain coverings not just as anatomical structures but as dynamic components in the complex ecosystem of the mind.
Additionally, studies have explored the role of the dura mater in modulating pain perception through its interaction with nociceptors and trigeminal nerve pathways. This suggests potential implications for individuals suffering from chronic migraine or cluster headaches, conditions often accompanied by cognitive symptoms such as irritability or difficulty concentrating. By understanding the full range of functions performed by this brain covering, clinicians and researchers may identify new avenues for therapeutic intervention targeting the dura’s structural and biochemical contributions to mental health.
The Arachnoid Mater: The Brain’s Fluid Mediator
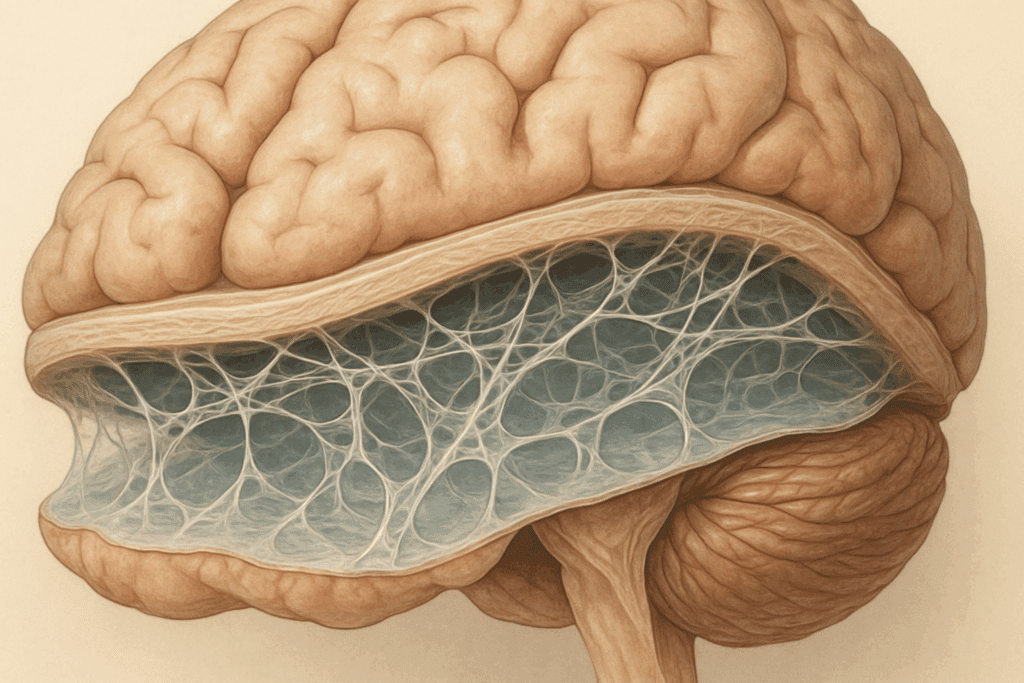
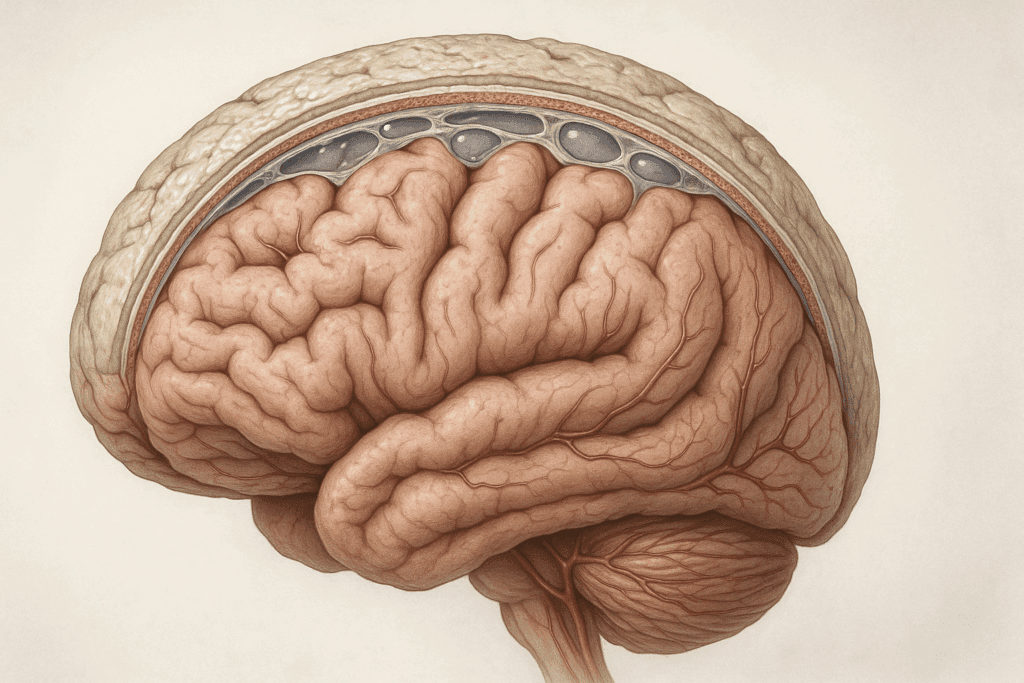
Nestled between the dura mater and the pia mater is the arachnoid mater, a delicate, web-like membrane that takes its name from the Greek word for spider. This middle layer of the brain covering is unique in both structure and function. Its web-like configuration creates a subarachnoid space filled with cerebrospinal fluid (CSF), which plays a key role in cushioning the brain and spinal cord.
This fluid environment is far more than a passive buffer. The CSF helps regulate intracranial pressure, remove metabolic waste, and distribute nutrients—all processes essential to maintaining brain health and function. Disruptions in CSF dynamics have been associated with neurodegenerative diseases such as Alzheimer’s and multiple sclerosis, as well as psychiatric disorders like bipolar disorder and chronic anxiety. Therefore, the arachnoid mater, as a brain layer that governs CSF flow, is indirectly but powerfully connected to mental health outcomes.
Moreover, the arachnoid mater is home to the arachnoid villi—small protrusions that absorb excess cerebrospinal fluid and return it to the bloodstream. This drainage system helps keep pressure levels in check, preventing conditions such as hydrocephalus. Just as unregulated physical pressure can damage delicate neural tissue, so too can the psychological pressure of mental stress. The analogy between physical and emotional balance is no coincidence; the body’s ability to maintain equilibrium on all fronts is intricately tied to the health of its brain coverings.
The arachnoid mater also serves as a semi-permeable membrane that helps control what substances can reach the brain. While the blood-brain barrier often takes center stage in this role, the arachnoid membrane’s contribution to selective permeability adds another layer of protection. This dual filtering mechanism reinforces the concept that the layers of brain protection are not redundant but rather collaborative—each contributing a unique function that collectively sustains mental resilience.
In clinical settings, conditions such as meningitis that affect the arachnoid mater can trigger severe psychological symptoms ranging from delirium to personality changes. The inflammation and infection within this brain covering demonstrate the direct relationship between structural compromise and altered mental states. For healthcare professionals, this underscores the importance of considering the integrity of brain coverings in differential diagnoses related to mental health complaints.
The Pia Mater: The Brain’s Intimate Ally
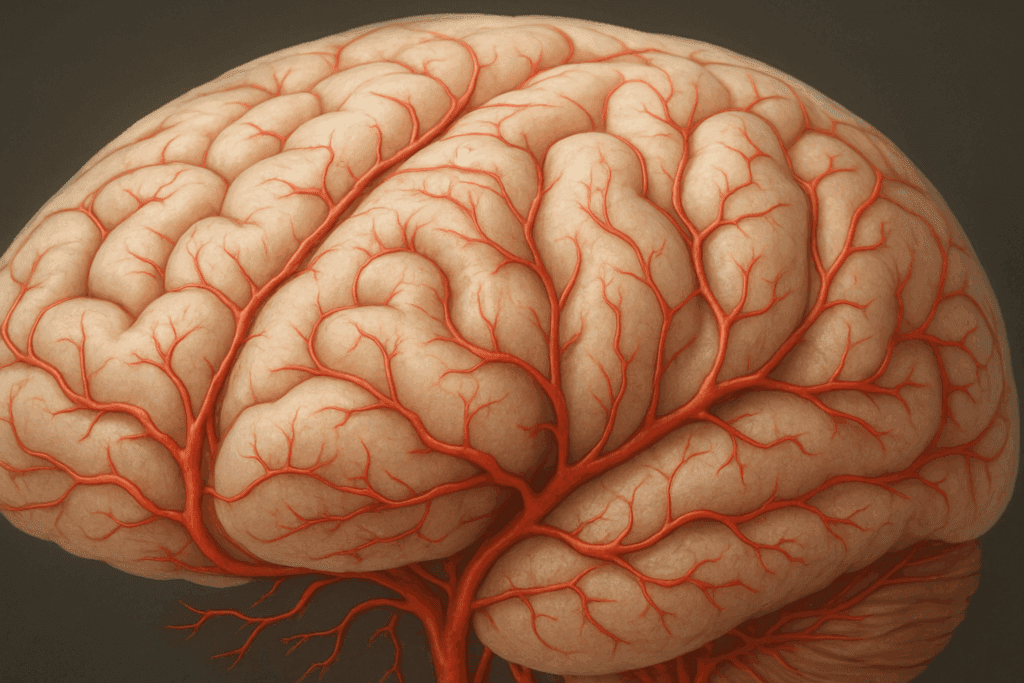
Of the three layers of the brain, the pia mater is the most delicate and intimately connected to neural tissue. It adheres closely to the contours of the brain, following every ridge and groove with meticulous precision. This close relationship allows the pia mater to act as a direct interface between the brain’s surface and its protective coverings, ensuring that essential substances like oxygen and glucose can efficiently pass into neural tissues.
While the pia mater might seem structurally insignificant compared to the robust dura mater, its role in supporting the health of neurons cannot be overstated. It houses a rich network of blood vessels that supply the brain with the nutrients it needs to function. Without the efficient delivery of these resources, mental faculties such as memory, attention, and emotional regulation would quickly deteriorate. Indeed, ischemic conditions that impair blood flow to the brain often begin at this microvascular level, making the pia mater essential in preventing strokes and cognitive decline.
This innermost brain layer is also involved in producing a small portion of the cerebrospinal fluid and contributes to the structural integrity of the blood-brain barrier. These roles position the pia mater not only as a passive membrane but also as an active participant in neuroprotection. Furthermore, the presence of immune cells within this brain covering hints at a more complex involvement in neurological defense mechanisms than once believed. From neurovascular regulation to immune surveillance, the pia mater serves as a sentinel for mental clarity and stability.
Perhaps most importantly, the pia mater’s integrity is vital in preserving the sanctity of the brain’s microenvironment. Because it is so closely associated with the actual surface of the brain, any breach—such as in cases of meningitis or traumatic injury—can lead to direct and severe neurological consequences. Therefore, maintaining the health of this particular brain covering is not just an anatomical concern but a mental health imperative. As researchers dive deeper into the pia mater’s unique cellular composition and signaling pathways, we may uncover new biomarkers for neurodegenerative diseases and psychiatric conditions alike.
Interplay Between the Brain Coverings and Mental Health Disorders
Although the 3 layers of the brain are often described in purely anatomical terms, emerging research is beginning to bridge the gap between structure and psychological function. Studies have shown that disruptions to the meninges can trigger a cascade of effects that impact mental health. For instance, chronic inflammation in any brain layer can contribute to neuroimmune dysregulation, a factor increasingly linked to depression, anxiety, and even psychosis.
The dura mater, with its high density of immune cells, has been shown to play a role in autoimmune brain diseases, which often present with psychiatric symptoms. Similarly, compromised cerebrospinal fluid flow—regulated by the arachnoid mater—can lead to symptoms that mimic major depressive disorder or cause executive dysfunction. In traumatic brain injury (TBI), damage to the pia mater often correlates with long-term cognitive impairments and heightened susceptibility to mood disorders.
Furthermore, structural changes in brain coverings have been noted in conditions like schizophrenia and bipolar disorder, although these findings are still under active investigation. What is clear, however, is that mental health does not exist in isolation from the physical integrity of the brain. Rather, it is interwoven with it—literally and metaphorically. This understanding opens new avenues for diagnosis and treatment, including imaging techniques that assess the health of the meninges and potential therapeutics that target meningeal inflammation.
These revelations also encourage a more holistic view of mental health interventions. Treatments like mindfulness, proper sleep hygiene, and anti-inflammatory diets not only benefit mood and cognition but may also preserve the function of each brain layer. Just as a calm mind supports a healthy brain, a well-maintained set of brain coverings provides the physical foundation for emotional and cognitive stability. The more we understand about the intricacies of these protective layers, the better equipped we are to promote mental resilience across the lifespan.
Aging, Brain Layers, and Cognitive Longevity
As we age, the health of the brain’s protective coverings becomes increasingly critical. Degenerative changes in the meninges can lead to altered cerebrospinal fluid dynamics, impaired blood flow, and a weakened blood-brain barrier—all of which can contribute to cognitive decline. Understanding how the layers of brain structure change over time provides valuable insights into the aging process and how to counteract its effects.
One of the earliest signs of aging-related neurological change is the calcification of the dura mater, which can impede its flexibility and impact intracranial pressure regulation. At the same time, the arachnoid mater may experience decreased efficiency in CSF absorption, leading to the accumulation of metabolic waste that can damage neurons. The pia mater, with its vascular network, may show reduced blood flow capacity, impairing the delivery of oxygen and nutrients to sensitive brain regions.
However, these changes are not entirely irreversible. Research suggests that certain lifestyle modifications can help maintain the health of brain coverings well into older adulthood. Regular aerobic exercise, for example, improves cerebral blood flow and enhances meningeal elasticity. Nutritional strategies that support vascular health—such as omega-3 fatty acids and antioxidant-rich foods—can protect the pia mater and its capillary networks. Meanwhile, stress reduction practices can lower the likelihood of chronic inflammation within any brain layer, preserving the overall integrity of the meninges.
These protective strategies underscore the value of a proactive approach to brain health. Rather than viewing mental decline as an inevitable consequence of aging, we can begin to see it as a modifiable risk, influenced in part by the condition of the brain’s coverings. Such an outlook empowers individuals to take charge of their cognitive future through informed lifestyle choices. In doing so, they not only protect their brain covering structures but also reinforce the connection between physical health and emotional well-being that is so critical in later life.
Frequently Asked Questions: How the 3 Layers of the Brain Protect Your Mind
1. How do lifestyle factors like diet and exercise influence the function of each brain covering?
Lifestyle choices play a critical role in maintaining the health and resilience of each brain covering. Regular physical exercise increases cerebral blood flow, which not only supports cognitive function but also maintains the elasticity and vascular health of the dura mater and pia mater. This is especially important as aging can stiffen the dura mater, reducing its ability to regulate intracranial pressure efficiently. Meanwhile, a nutrient-rich diet—particularly one high in omega-3 fatty acids and antioxidants—can help protect the delicate vascular network within the pia mater, ensuring optimal delivery of oxygen and glucose to neurons. This direct support for vascular structures reinforces the overall integrity of each brain layer.
On the other hand, poor lifestyle habits like excessive alcohol consumption or chronic sleep deprivation can degrade the protective capabilities of the brain coverings over time. Alcohol, for example, has been shown to compromise blood-brain barrier integrity and may increase inflammation within the brain coverings, particularly the pia mater. Sleep is another crucial factor, as cerebrospinal fluid clearance—which relies heavily on the arachnoid mater—accelerates during deep sleep stages. Disruption of this process can lead to waste accumulation and inflammatory responses in the layers of brain tissue. In this way, even seemingly mundane habits can have a long-term impact on the 3 layers of the brain.
Furthermore, stress management techniques like meditation and yoga are being explored for their potential to reduce inflammation across the brain layer system. These practices may influence neuroimmune activity associated with the dura mater and arachnoid mater, suggesting a profound link between mind-body practices and structural brain protection. Taken together, a comprehensive lifestyle strategy that includes nutrition, exercise, and stress reduction is increasingly recognized as vital for sustaining the health of every brain covering and, by extension, promoting mental well-being.
2. Can the layers of brain coverings affect emotional regulation and mood disorders?
Yes, the health and function of brain coverings can significantly influence emotional regulation and the development or exacerbation of mood disorders. While emotional processing is typically associated with limbic structures like the amygdala or hippocampus, recent research has suggested that inflammation or dysfunction within the 3 layers of the brain may indirectly affect these systems. For example, chronic inflammation in the dura mater can activate immune pathways that lead to the release of cytokines, which have been linked to depressive and anxious behaviors in both animal and human studies. This interplay between immune signaling and mood suggests that brain coverings play a subtle but impactful role in emotional balance.
The arachnoid mater, through its regulation of cerebrospinal fluid (CSF), also influences mood stability. Poor CSF circulation may allow for the accumulation of metabolic byproducts that interfere with neurotransmitter function, potentially contributing to the biochemical imbalances often seen in mood disorders. This is particularly relevant in disorders such as bipolar disorder, where fluctuations in brain fluid dynamics have been noted. Furthermore, the brain layer’s semi-permeable nature means it helps control which substances can reach the deeper brain regions, providing another level of chemical regulation tied to mood and emotion.
The pia mater, being rich in capillaries and in close contact with neurons, is instrumental in delivering the nutrients and oxygen vital for mood-regulating brain functions. Any compromise to its integrity—whether through vascular aging or neuroinflammation—can diminish the brain’s capacity to maintain stable neurotransmitter levels, further influencing emotional states. This means that while brain coverings are often considered secondary to brain tissue in mental health, they may actually hold key regulatory roles in how we experience and manage emotion. As research evolves, these connections between brain covering health and emotional regulation are likely to become more clinically significant in psychiatric care.
3. Are there any emerging technologies that can assess the health of each brain layer?
Emerging technologies are making it increasingly possible to assess the health and integrity of the layers of brain tissue in clinical and research settings. One of the most promising advancements is high-resolution magnetic resonance imaging (MRI), which can now differentiate between the individual layers of the meninges with impressive accuracy. Specialized contrast agents and diffusion tensor imaging (DTI) have made it feasible to observe subtle structural changes in each brain covering, including thickening, inflammation, or vascular abnormalities. These tools allow for non-invasive evaluations of how well each brain layer is functioning, especially in conditions like multiple sclerosis, meningitis, or chronic neuroinflammation.
Ultrasound elastography, though still in developmental stages for neurological application, is another innovative technology that may one day be used to measure the mechanical properties of the dura mater. Changes in elasticity can indicate underlying problems such as fibrosis or calcification, which are associated with aging or disease. Such a technique would be particularly useful in evaluating the outermost brain covering in elderly patients or those with head trauma. Researchers are also investigating how optical coherence tomography, typically used in ophthalmology, could be adapted to examine superficial brain structures like the pia mater during surgery or in specialized imaging environments.
Biomarkers in cerebrospinal fluid are also gaining traction as indirect indicators of brain covering health. For instance, elevated levels of certain proteins in the CSF may suggest inflammation or breakdown of the arachnoid mater’s regulatory function. These emerging diagnostic strategies, while still evolving, underscore a shift in neuroscience toward recognizing the 3 layers of the brain not just as passive membranes but as active structures worthy of clinical attention. As these technologies become more refined, they may revolutionize how we monitor and treat conditions related to brain covering dysfunction.
4. How do autoimmune diseases target brain coverings, and what are the implications?
Autoimmune diseases can have a profound impact on the brain coverings by initiating inflammatory attacks against these protective layers. Conditions like multiple sclerosis (MS), neurosarcoidosis, and systemic lupus erythematosus (SLE) often involve immune system dysregulation that targets the central nervous system, including the layers of brain tissue. In multiple sclerosis, for example, immune cells sometimes breach the dura mater and infiltrate the subarachnoid space, disrupting cerebrospinal fluid dynamics and contributing to the demyelination of neurons. This direct attack on brain coverings can exacerbate the neurological and psychological symptoms of autoimmune disorders.
Moreover, autoimmune inflammation within the arachnoid mater can severely alter CSF flow and increase intracranial pressure, potentially leading to cognitive impairment or mood dysregulation. These changes may not always be visible through routine imaging, making it essential to consider autoimmune etiologies when diagnosing unexplained neuropsychiatric symptoms. Autoantibodies can also affect the pia mater, disrupting blood-brain barrier function and allowing harmful substances or additional immune cells to enter the brain, amplifying neuroinflammatory cascades. Such breaches can increase susceptibility to secondary infections and raise the risk of psychiatric complications.
Clinicians are increasingly recognizing the importance of early detection and targeted immunotherapy for autoimmune conditions that impact the 3 layers of the brain. Treatments such as corticosteroids, biologic agents, or plasmapheresis may help reduce inflammation and preserve brain covering function. Additionally, research into specific biomarkers for autoimmune damage to each brain layer is underway, offering the possibility of more precise diagnostics in the future. Ultimately, understanding how autoimmune responses interact with each brain covering adds a new layer of complexity—and opportunity—to the treatment of neuroimmune disorders.
5. Can traumatic brain injuries (TBIs) cause long-term damage to brain coverings, and what are the risks?
Traumatic brain injuries (TBIs) can inflict long-lasting damage on the brain coverings, and this damage often goes underdiagnosed compared to the more apparent neural trauma. A direct blow to the head can cause tears or shearing forces within the 3 layers of the brain, especially the dura mater, which is prone to developing subdural hematomas. These bleeding episodes can increase intracranial pressure, disrupt blood flow, and impair the brain’s ability to function normally. Even when overt bleeding is not present, microstructural damage to each brain covering may set the stage for chronic inflammation and neurodegeneration.
Damage to the arachnoid mater is particularly concerning because it can compromise cerebrospinal fluid flow. A common consequence is post-traumatic hydrocephalus, a condition where CSF accumulates and leads to increased pressure on the brain. This pressure can alter the biochemical environment within the brain, interfering with neurotransmitter function and elevating the risk for mood disorders or cognitive decline. The integrity of the arachnoid layer is, therefore, a critical consideration in both acute care and long-term rehabilitation planning for TBI patients.
The pia mater, being the most delicate and directly connected to the brain’s surface, is especially vulnerable in high-impact injuries. Disruption to its vascular network may lead to localized ischemia or trigger inflammatory responses that damage surrounding neural tissue. Long-term effects may include memory problems, executive dysfunction, and emotional dysregulation—symptoms often mistakenly attributed solely to neural damage. Understanding how brain layer trauma contributes to these outcomes can refine both diagnostic protocols and recovery strategies, ensuring that clinicians address all components of brain injury. By incorporating evaluations of each brain covering, care teams can develop more nuanced and effective treatment plans for those recovering from TBIs.
6. How might the layers of brain coverings influence neurodevelopment in children and adolescents?
During childhood and adolescence, the brain undergoes rapid structural and functional changes, and the 3 layers of the brain play crucial yet underappreciated roles in this developmental process. The pia mater, for instance, facilitates the delivery of essential nutrients and oxygen to maturing neurons. In a developing brain, any interruption in this supply can impair synaptogenesis, the formation of synaptic connections vital for learning and memory. This makes the integrity of this brain covering especially important during critical windows of neurodevelopment.
The arachnoid mater, which manages cerebrospinal fluid (CSF) dynamics, also plays a key role in waste clearance and intracranial pressure regulation. These processes are particularly active during periods of rapid brain growth. Inadequate CSF drainage may result in pediatric conditions like hydrocephalus, which can lead to developmental delays or cognitive impairment. Subtle dysfunctions in CSF circulation governed by this brain layer may go undetected but still influence long-term outcomes in emotional regulation and executive function.
The dura mater, while primarily a mechanical shield, interacts with emerging immune and vascular systems during early development. Studies suggest that inflammation or premature calcification of this brain layer during infancy or adolescence can trigger immune responses that potentially disrupt brain maturation. Pediatric neurological disorders such as autism spectrum disorder (ASD) and attention-deficit/hyperactivity disorder (ADHD) are being examined in the context of meningeal development, indicating a broader relevance of brain coverings in neuropsychiatric health.
As neuroscience advances, there is growing recognition that supporting the healthy development of the brain coverings may be just as important as fostering synaptic and cortical maturation. Pediatric care that includes early detection of brain layer dysfunction—perhaps through neuroimaging or biomarker analysis—could become a cornerstone of preventive strategies in child and adolescent mental health.
7. Can infections like meningitis permanently damage the 3 layers of the brain?
Meningitis, an infection that inflames the meninges, can indeed cause lasting damage to all 3 layers of the brain, particularly when not treated promptly. The dura mater may experience fibrosis or scarring, reducing its flexibility and impairing its ability to manage intracranial pressure. More critically, the arachnoid mater, which governs cerebrospinal fluid circulation, can develop adhesions or blockages after infection. This can lead to chronic hydrocephalus, where CSF accumulates and compresses neural tissues, affecting cognitive and physical function.
Damage to the arachnoid layer may also impair the absorption of CSF, which is essential for clearing metabolic waste. This disruption in fluid dynamics could increase the risk of long-term neurological complications, including memory deficits, difficulty concentrating, and mood instability. The pia mater, being the innermost and most delicate of the brain coverings, is often the most affected during bacterial meningitis. Inflammation here can damage the capillaries that nourish the brain, potentially leading to localized neuronal death and brain atrophy.
Even after the infection is cleared, post-meningitic complications like seizures, sensory processing issues, or behavioral changes may persist. These are often not due solely to brain tissue damage but to the lingering effects on the layers of brain protection. Advanced imaging techniques are increasingly used to assess the long-term impact of meningitis on these brain layers, offering insights into the anatomical origins of post-infectious symptoms.
Vaccination and prompt antibiotic or antiviral treatment remain critical in preventing irreversible damage. Rehabilitation following meningitis should not overlook the brain coverings as potential contributors to ongoing cognitive or emotional issues. New therapies aimed at reducing inflammation or promoting tissue regeneration in these layers may soon play a larger role in long-term recovery and the prevention of secondary neurological disorders.
8. What role do the brain coverings play in sleep quality and circadian rhythm regulation?
Although often overlooked in sleep science, the 3 layers of the brain have an indirect yet significant role in regulating sleep quality and circadian rhythms. One of the most crucial mechanisms influenced by the brain coverings—particularly the arachnoid mater—is the circulation of cerebrospinal fluid (CSF). During deep sleep, CSF clearance intensifies, flushing out toxins such as beta-amyloid, which are associated with neurodegenerative conditions. Impaired function of this brain layer may reduce waste clearance efficiency, thereby lowering sleep quality and increasing the risk of cognitive decline.
The pia mater, closely aligned with neural tissue, also contributes by ensuring the stable delivery of nutrients like glucose during sleep. Brain cells remain metabolically active even while we rest, and any dysfunction in this brain covering may disrupt the microvascular networks that support nighttime brain maintenance. Inadequate nutrient supply could lead to disrupted REM sleep, which is vital for emotional processing and memory consolidation.
Emerging research suggests the dura mater may also play a part in the biomechanical aspects of sleep. Since it houses blood vessels and lymphatic-like structures recently discovered in the central nervous system, its role in fluid drainage and pressure regulation is gaining new attention. Any imbalance in this system can affect not only sleep patterns but also the hormonal cycles that govern circadian rhythms, such as melatonin secretion.
Furthermore, inflammatory responses in any brain layer may interfere with the neural circuits involved in sleep-wake cycles. Chronic stress or immune activation targeting these coverings can lead to insomnia or fragmented sleep, contributing to mood disorders and reduced cognitive performance. Understanding how brain coverings intersect with sleep physiology may lead to novel approaches in treating sleep disorders and enhancing mental health through improved meningeal care.
9. Are there gender differences in how the brain layer system responds to stress or disease?
Yes, emerging evidence suggests there are gender-based differences in how the 3 layers of the brain respond to physiological stress and disease. Hormonal differences—particularly in estrogen and progesterone—may influence inflammatory responses in the brain coverings. For example, estrogen has been shown to exert a protective effect on the dura mater by modulating immune activity and promoting vascular resilience. This could partly explain why premenopausal women often have lower rates of certain neurological diseases that involve meningeal inflammation.
However, women also appear more susceptible to autoimmune diseases like multiple sclerosis and lupus, which frequently involve immune attacks on brain coverings. The arachnoid mater is often implicated in these diseases due to its role in immune surveillance and CSF circulation. Gender-related differences in cytokine profiles and blood-brain barrier permeability may make the female brain layer system more prone to inflammatory cascades under specific conditions.
On the other hand, men may be at greater risk of meningeal complications following traumatic brain injuries. Research indicates that male brains exhibit a heightened inflammatory response in the dura and arachnoid mater after injury, potentially increasing the risk of long-term cognitive or emotional dysfunction. This has implications for clinical management, as personalized treatments based on gender could help mitigate such risks.
Gender also plays a role in how pain is perceived and processed, with the dura mater containing nociceptors linked to headache and migraine pathways. Women are statistically more prone to migraines, suggesting a possible connection between hormonal fluctuations and dural sensitivity. Future studies focusing on gender-specific responses in brain coverings may yield new insights into optimizing treatments for neurological and psychiatric conditions across diverse populations.
10. How could future therapies be designed to strengthen or repair damaged brain coverings?
Future therapies aimed at strengthening or repairing the layers of brain coverings are expected to become a central focus in neuroprotective medicine. One promising direction involves the development of biomaterials that can mimic or reinforce the structure of each brain layer. For instance, hydrogel scaffolds impregnated with anti-inflammatory agents or stem cells may be used to repair damage in the dura mater following surgery or trauma. These bioengineered patches could eventually be applied in minimally invasive procedures to restore the protective function of the outermost brain covering.
Nanotechnology also offers exciting possibilities for delivering therapeutic agents directly to the pia mater or arachnoid mater. Nanoparticles designed to cross the blood-brain barrier could be programmed to release drugs in response to inflammation markers, offering targeted treatment for autoimmune or infectious damage within the brain coverings. Such approaches could reduce side effects and improve the precision of meningeal therapies.
Gene therapy is another frontier being explored, particularly for congenital conditions that impair brain covering function. By targeting genes involved in collagen production or CSF regulation, researchers hope to enhance the resilience of all 3 layers of the brain. These therapies could be administered early in life or after injury to prevent long-term deterioration and preserve mental function.
Finally, pharmaceutical research is beginning to investigate compounds that enhance the structural integrity of the brain layers without invasive procedures. Flavonoids, omega-3s, and other nutraceuticals are being tested for their ability to support vascular networks within the pia mater and reduce immune reactivity in the dura mater. As our understanding of brain coverings deepens, future therapies will likely integrate material science, pharmacology, and personalized medicine to restore and protect these essential but often overlooked structures.
Conclusion: Protecting the Brain by Understanding Its Layers
The concept of safeguarding mental health has often centered on psychology, therapy, and pharmaceuticals, but there is an equally important anatomical perspective to consider. The 3 layers of the brain—dura mater, arachnoid mater, and pia mater—are not just passive barriers; they are active participants in the preservation of cognitive and emotional well-being. Each brain layer plays a vital role in regulating blood flow, managing cerebrospinal fluid, and mediating immune responses—all of which are foundational to a healthy mind.
As research continues to unravel the complexities of the brain covering system, it becomes increasingly clear that these structures are far more than biological wrappings. They are integral to the delicate equilibrium that supports thought, memory, mood, and resilience. Whether we are considering the physical consequences of brain injury or the subtle biochemical shifts that accompany aging, the condition of the brain’s protective layers matters profoundly.
For individuals seeking to maintain long-term mental clarity and emotional balance, understanding the layers of brain protection is not merely academic—it is practical. Supporting these layers through lifestyle choices, medical care, and continued education can enhance not only our physical well-being but also our mental and cognitive longevity. As we move forward in redefining what it means to nurture mental health, let us not forget the vital scaffolding that holds the mind together: the coverings of the brain that quietly, yet powerfully, protect our most essential human capacities. In this understanding, we find a powerful reminder—that true brain health begins not only with what happens inside the neurons but also with the integrity of the layers that safeguard them.
Further Reading:
The 3 Layers of Meninges: What Are They and What Are They For?