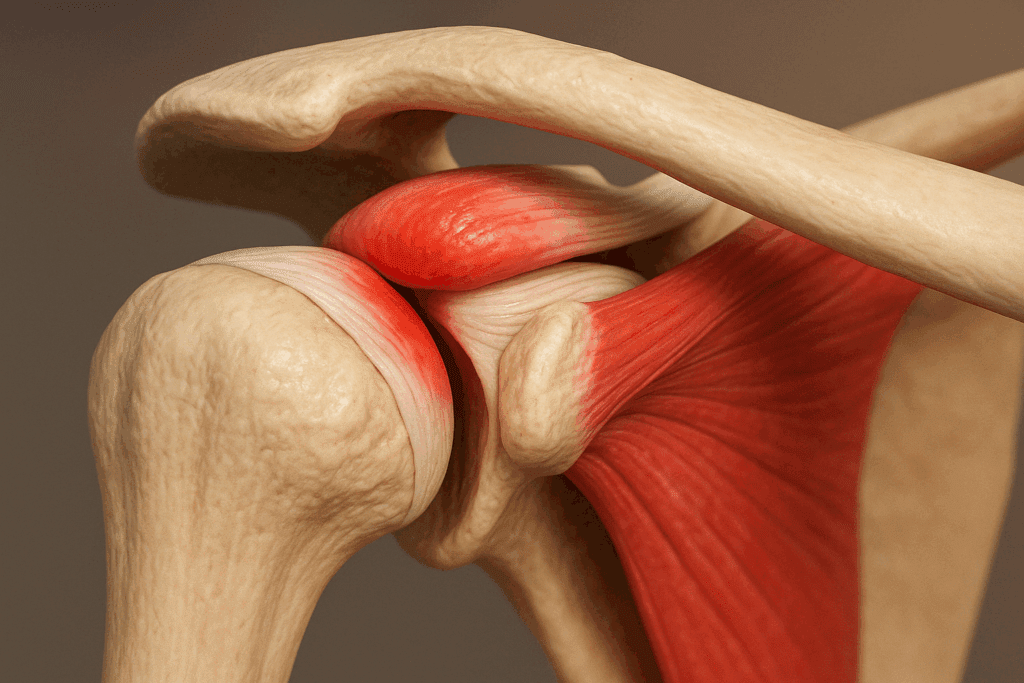
Shoulder impingement syndrome is a common but often misunderstood condition that affects individuals ranging from athletes to office workers. Characterized by pain and reduced mobility in the shoulder, it occurs when the rotator cuff tendons become compressed between the bones of the shoulder joint, particularly the acromion and humeral head. This compression leads to inflammation, pain, and eventually a loss of function if left unaddressed. The most effective approach to managing this condition combines rest, physical therapy, and a carefully designed regimen of targeted movements. In this comprehensive guide, we explore the best exercises for shoulder impingement syndrome and highlight how they can alleviate symptoms while promoting long-term mobility and joint health.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Understanding the Mechanics Behind Shoulder Impingement
To truly appreciate how exercises for impinged shoulder conditions can help, it is essential to understand the biomechanics of the shoulder joint. The shoulder is a ball-and-socket joint with remarkable mobility, but this flexibility also makes it vulnerable to instability and mechanical dysfunction. Impingement typically arises when the space between the acromion and the rotator cuff narrows, often due to poor posture, muscular imbalances, repetitive overhead motion, or structural abnormalities like bone spurs. The resulting friction can cause swelling and irritation of the tendons, leading to persistent discomfort and restricted range of motion.
Unlike acute injuries, which result from sudden trauma, shoulder impingement tends to develop gradually. This progressive nature highlights the importance of early intervention through exercises specifically designed to reduce inflammation and restore functional movement. A consistent, structured exercise plan can decrease pain, enhance strength, and improve posture—all of which contribute to long-term recovery and prevention of recurrence.
Why Exercise Is Crucial in Managing Shoulder Impingement
When dealing with shoulder impingement syndrome, rest alone is rarely sufficient for a full recovery. While temporary rest can reduce acute inflammation, inactivity may also lead to stiffness and weakening of the shoulder stabilizers. Targeted exercises help to reestablish joint mechanics by strengthening the rotator cuff, improving scapular control, and promoting proper posture. Importantly, the best exercises for shoulder impingement syndrome do not exacerbate pain but instead support healing by increasing circulation, maintaining flexibility, and enhancing neuromuscular control.
Research supports the efficacy of therapeutic exercise in managing shoulder impingement. Clinical studies have consistently shown that structured rehabilitation programs are as effective, if not more so, than corticosteroid injections for long-term symptom relief. Moreover, exercise interventions carry fewer risks and support whole-body function, making them a cornerstone of evidence-based treatment for this condition. With proper guidance, individuals can safely integrate exercises into their daily routine to support pain relief and functional recovery.
The Kinetic Chain and Shoulder Dysfunction
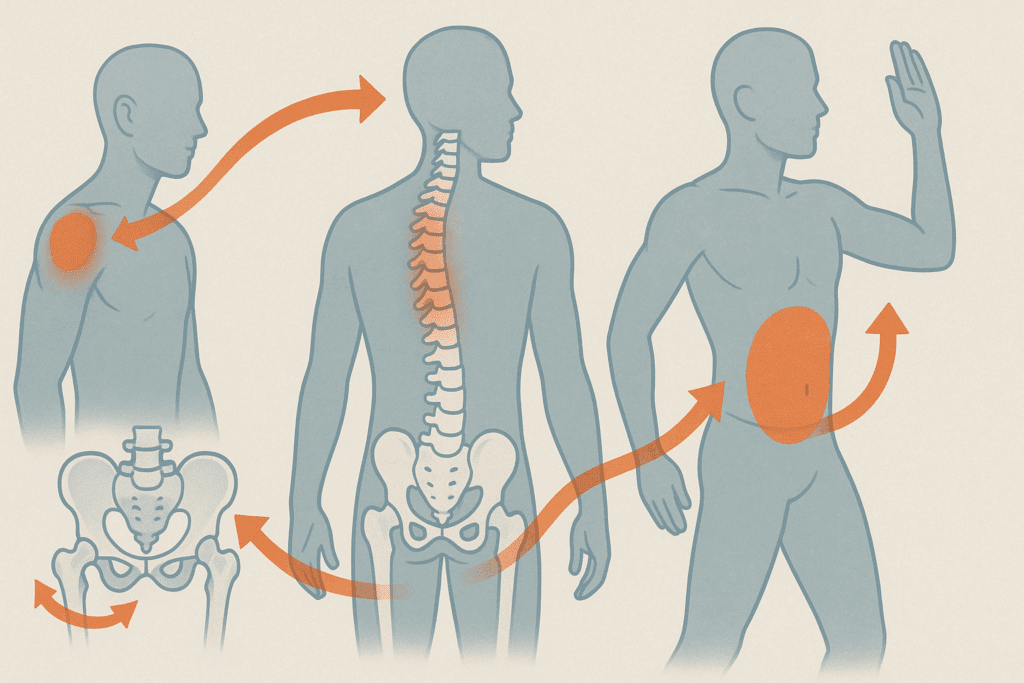
While much of the focus in shoulder impingement rehabilitation lies in localized strengthening and mobility exercises, it is increasingly recognized that shoulder function is deeply interconnected with the rest of the body—particularly the thoracic spine, cervical spine, and hips. The concept of the kinetic chain emphasizes that no joint operates in isolation. Dysfunction or restriction in adjacent areas can alter the biomechanics of the shoulder, setting the stage for impingement.
Thoracic spine stiffness, for example, restricts the ability to extend and rotate through the upper back, which is essential for proper scapular motion. Without adequate thoracic extension, the scapula cannot upwardly rotate effectively during arm elevation, narrowing the subacromial space and increasing the risk of impingement. Likewise, poor hip mobility or weak core engagement can lead to compensatory upper body mechanics that place excess strain on the shoulders. These relationships highlight the importance of assessing and addressing movement quality throughout the kinetic chain when designing a comprehensive recovery plan.
Neurodynamics and the Role of the Nervous System
Another often-overlooked aspect of shoulder impingement is the contribution of neural tension and sensitivity. The nerves that innervate the shoulder and arm—primarily the brachial plexus—travel through a series of anatomical tunnels and are susceptible to mechanical irritation, especially in posturally compromised individuals. Neural irritation can mimic or exacerbate the symptoms of impingement, leading to burning, tingling, or radiating pain that does not resolve with traditional rotator cuff or scapular exercises alone.
In these cases, neurodynamic mobilization techniques can be incredibly beneficial. These gentle movements are designed to restore the gliding capability of the nerves within their sheaths, reducing mechanosensitivity and improving the overall function of the neuromuscular system. Nerve glides for the median, radial, and ulnar nerves are often incorporated into impingement rehab programs when neurogenic symptoms are present. This neural perspective complements the mechanical model of impingement and provides another avenue for symptom resolution.
Postural Correction as a Foundation for Recovery
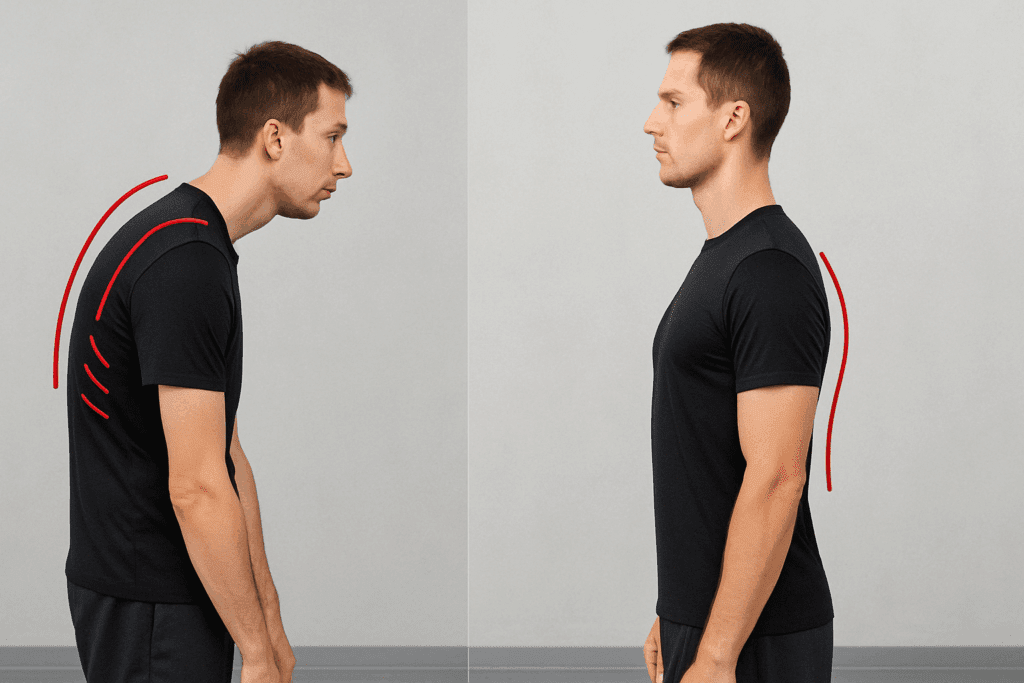
One often-overlooked contributor to shoulder impingement is poor posture, particularly the rounded-shoulder, forward-head posture associated with prolonged sitting and screen use. This alignment compresses the subacromial space, placing additional stress on the rotator cuff and surrounding tissues. Addressing postural issues through exercise can dramatically improve shoulder kinematics and reduce impingement symptoms.
Postural correction involves more than simply “standing up straight.” It requires a combination of thoracic spine mobilization, scapular strengthening, and pectoral stretching. For instance, foam rolling the upper back helps restore thoracic extension, which supports more natural scapular positioning. At the same time, exercises that activate the lower trapezius and rhomboids can counteract the dominance of the upper trapezius and pectoralis minor, which tend to pull the shoulder blades into a protracted, elevated position. These foundational changes set the stage for more targeted rehabilitation exercises to be effective.
Scapular Stabilization: Rebuilding the Shoulder’s Foundation
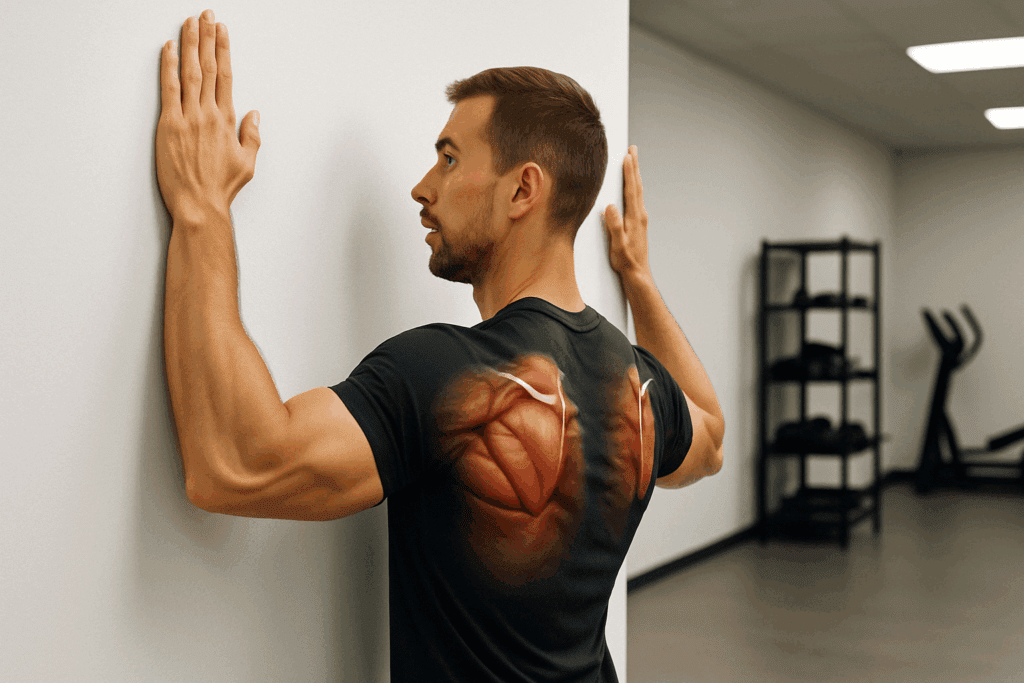
Scapular stability is essential for efficient shoulder mechanics. The scapula, or shoulder blade, serves as the anchor for numerous muscles involved in arm elevation and rotation. Dysfunction in scapular motion can contribute directly to impingement by altering the angle at which the rotator cuff tendons move under the acromion. Strengthening the muscles that control scapular movement—particularly the serratus anterior, lower trapezius, and middle trapezius—can restore proper motion patterns and reduce stress on the rotator cuff.
Exercises like scapular clocks, wall slides, and prone Y raises target these key stabilizers. In scapular clocks, the shoulder blade is moved deliberately in different directions (as if tracing a clock face), promoting neuromuscular control and awareness. Wall slides incorporate both scapular and thoracic mobility while encouraging external rotation, which helps open the subacromial space. Meanwhile, prone Y raises on a stability ball or mat activate the lower trapezius and reinforce scapular depression—a key movement for preventing impingement. When performed consistently, these exercises lay a critical foundation for shoulder health and resilience.

Rotator Cuff Strengthening for Long-Term Stability
The rotator cuff consists of four muscles—supraspinatus, infraspinatus, teres minor, and subscapularis—that work together to stabilize the humeral head within the shoulder socket. Weakness or imbalance in these muscles is a primary factor in shoulder impingement syndrome. Strengthening the rotator cuff through low-load, high-control movements improves joint stability and reduces the likelihood of further irritation.
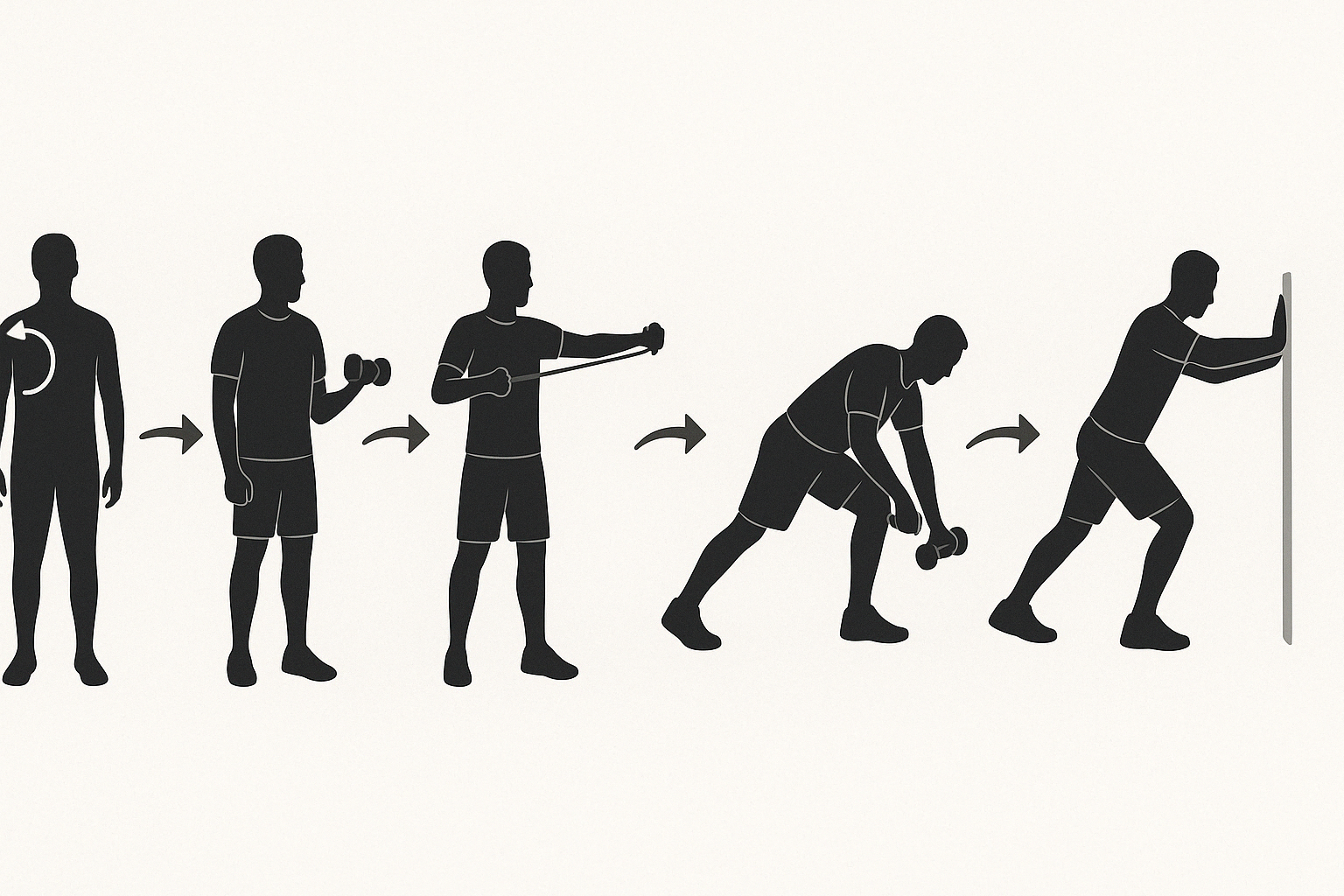
Isometric external rotation exercises, sidelying external rotations, and resistance band internal rotations are particularly effective for strengthening the rotator cuff. These movements should be performed with slow, deliberate control to avoid compensatory patterns that can stress adjacent tissues. Isometric holds, where the joint remains static against resistance, are especially useful in the early stages of rehabilitation when dynamic motion may still provoke discomfort. As strength improves, dynamic resistance exercises can be introduced to further enhance function and resilience.
Manual Therapy: Hands-On Techniques That Complement Exercise
While exercise forms the cornerstone of long-term recovery, manual therapy techniques performed by physical therapists, chiropractors, or massage therapists can accelerate healing and provide symptomatic relief. Soft tissue mobilization, joint mobilizations, and myofascial release target restrictions that may limit mobility or contribute to altered movement patterns.
For instance, manual release of the pectoralis minor can facilitate better scapular retraction and upward rotation, essential for impingement relief. Likewise, thoracic spine joint mobilizations can improve segmental motion and enhance postural alignment. These interventions often create a window of opportunity where movement becomes more accessible and less painful, allowing the individual to perform rehabilitation exercises more effectively. When used judiciously and in conjunction with active strategies, manual therapy can be a powerful adjunct to a comprehensive treatment plan.
Sleep Quality and Recovery Potential
Sleep plays a vital role in tissue repair, hormonal regulation, and pain modulation. Poor sleep quality has been directly associated with increased sensitivity to pain and slower recovery from musculoskeletal injuries. Many individuals with shoulder impingement report difficulty finding a comfortable sleep position, which further exacerbates the issue. Lying on the affected shoulder can compress irritated structures, while certain positions may place tension on the neck and upper back, indirectly affecting the shoulder joint.
Optimizing sleep hygiene—by maintaining a consistent sleep schedule, avoiding screens before bed, and creating an ergonomic sleep environment—can contribute significantly to healing. Side sleepers may benefit from placing a pillow between the arm and torso to support the shoulder in a more neutral position. Even modest improvements in sleep duration and quality can have profound effects on recovery timelines and the perception of pain.
Technology and Digital Tools in Shoulder Rehabilitation
Modern technology has introduced innovative tools to enhance shoulder rehabilitation, particularly for remote or self-directed care. Wearable motion sensors, app-guided exercise programs, and virtual physical therapy platforms allow individuals to track their progress, receive real-time feedback, and stay consistent with their recovery plan. These digital solutions are especially valuable in improving adherence and ensuring proper form during unsupervised exercise sessions.
Telehealth consultations also make it easier for patients to access expert guidance, particularly those in rural or underserved areas. As shoulder impingement recovery often spans weeks to months, digital tools can support continuity of care and facilitate more frequent communication between patients and clinicians. While technology cannot replace the expertise of in-person assessments, it can significantly enhance accessibility and engagement in the rehabilitation process.

Restoring Range of Motion with Controlled Mobility Work
Loss of mobility is a hallmark of shoulder impingement and can contribute to a cycle of pain and dysfunction. Limited range of motion restricts the ability to perform daily tasks and increases reliance on compensatory movements, which may further aggravate the shoulder. Incorporating mobility work into a rehabilitation plan helps restore natural movement and supports joint lubrication, which is critical for healing.
Pendulum swings, wall-assisted flexion, and cross-body stretches are gentle yet effective ways to regain shoulder motion. Pendulum swings, performed by leaning forward and allowing the arm to dangle and move passively, use gravity to facilitate motion without muscular strain. Wall-assisted flexion allows the shoulder to move through its range of motion in a supported, pain-free manner. Cross-body stretches target the posterior capsule and posterior deltoid, which often become tight in individuals with impingement. Together, these movements help reestablish normal mechanics and prepare the shoulder for more dynamic activity.
Incorporating Eccentric Training for Tendon Remodeling
Recent research into tendon rehabilitation has highlighted the importance of eccentric training—where the muscle lengthens under tension—for promoting tendon healing and remodeling. Eccentric exercises stimulate collagen synthesis and help align tendon fibers, making them more resilient to future strain. For individuals recovering from shoulder impingement syndrome, eccentric loading of the rotator cuff and associated musculature can enhance tissue quality and reduce pain.
A practical example of eccentric training is the eccentric external rotation, where the shoulder is externally rotated against resistance and then returned slowly to the starting position. This deliberate lowering phase recruits muscle fibers differently than concentric movement, placing a therapeutic load on healing tissues. Eccentric training should be introduced gradually and performed with strict control to prevent re-injury. When integrated appropriately, it offers a valuable complement to traditional strengthening and mobility work.

Advanced Neuromuscular Re-education for Long-Term Success
As the shoulder begins to recover, rehabilitation should transition from isolated exercises to more integrative, functional movements that mimic real-world demands. Neuromuscular re-education involves retraining the brain and body to coordinate movement efficiently, reducing reliance on compensatory patterns that may have developed during the painful phase. This process enhances proprioception, or the body’s sense of joint position, which is often impaired in individuals with chronic shoulder impingement.
Closed kinetic chain exercises such as quadruped weight shifts, wall push-ups with scapular protraction, and modified planks encourage the shoulder to bear weight in a controlled manner, improving joint awareness and dynamic stability. These movements also integrate core activation and scapular control, which are essential for healthy upper limb function. As patients progress, sport- or task-specific drills can be added to further refine movement patterns and ensure lasting improvements in mobility and pain relief.
Progression and Personalization: Tailoring the Program to the Individual
Not all exercises for impinged shoulder recovery are appropriate for every individual at every stage of healing. A successful rehabilitation plan must be personalized based on the severity of symptoms, the presence of structural abnormalities, and the individual’s baseline mobility and strength. While some people may benefit from early resistance training, others may need to focus on gentle mobility work before advancing to more demanding exercises.
Progression should follow a logical sequence, beginning with pain-free mobility exercises and isometric activation, followed by dynamic resistance, eccentric loading, and eventually functional integration. Regular reassessment with a qualified physical therapist ensures that the program remains aligned with the patient’s progress and goals. This personalized approach helps optimize outcomes while minimizing the risk of reinjury.
When to Seek Professional Guidance
Although home-based exercise programs can be highly effective, certain signs indicate the need for professional evaluation. Persistent or worsening pain despite adherence to a rehabilitation routine, significant weakness or loss of function, or suspicion of underlying structural pathology such as a rotator cuff tear or labral injury should prompt consultation with a healthcare provider. Imaging studies, such as MRI or ultrasound, may be warranted in these cases to clarify the diagnosis and guide further treatment.
Working with a licensed physical therapist provides access to expert evaluation, manual therapy techniques, and supervised exercise progression. These professionals can help identify subtle movement dysfunctions, address underlying postural or muscular imbalances, and ensure that exercises are performed safely and effectively. Collaboration between the patient and clinician enhances accountability and supports long-term recovery.
Preventing Recurrence: Maintaining Shoulder Health Over Time
Recovery from shoulder impingement syndrome does not end with the resolution of symptoms. Maintaining the gains achieved through rehabilitation requires ongoing attention to posture, movement quality, and strength balance. Incorporating regular mobility and stability exercises into a general fitness routine can help preserve shoulder health and prevent recurrence.
Lifestyle modifications, such as ergonomic adjustments at workstations, proper lifting mechanics, and periodic stretching breaks during prolonged activity, also play a crucial role. For athletes and active individuals, preseason conditioning and sport-specific training can prepare the shoulder for high-demand tasks and reduce injury risk. The best exercises for shoulder impingement syndrome are those that not only resolve symptoms but also create a foundation for sustainable function and resilience.
Integrating Holistic Wellness for Optimal Results
Beyond physical rehabilitation, a holistic approach to shoulder recovery can further enhance outcomes. Nutritional support, including adequate protein intake and anti-inflammatory nutrients such as omega-3 fatty acids, may aid in tissue healing and reduce chronic inflammation. Stress management techniques like meditation and deep breathing can lower systemic tension that contributes to muscular tightness and postural imbalance.
Sleep quality, often overlooked, plays a significant role in musculoskeletal health. During deep sleep, the body undergoes repair processes that are essential for recovery. Ensuring sufficient rest and addressing sleep disturbances can accelerate the healing process. These integrative strategies, when combined with the best exercises for shoulder impingement syndrome, create a comprehensive plan for regaining comfort and mobility.
Frequently Asked Questions: Shoulder Impingement Syndrome – Beyond the Basics
1. Are there effective alternatives to traditional physical therapy for shoulder impingement syndrome?
Yes, there are several complementary approaches that can enhance or even substitute for traditional physical therapy in certain cases. For instance, neuromuscular electrical stimulation (NMES) can be used to retrain weakened shoulder muscles when active movement is painful. Similarly, aquatic therapy offers a low-impact environment where mobility can be restored with minimal stress on the joint. Some patients benefit from modalities like dry needling or cupping therapy to address deep fascial restrictions contributing to poor shoulder mechanics. These strategies are not replacements for the best exercises for shoulder impingement syndrome, but when integrated strategically, they can support faster and more comfortable recovery.
2. Can lifestyle factors influence the effectiveness of exercises for impinged shoulder recovery?
Absolutely. Diet, hydration, and sleep quality all play critical roles in tissue healing, inflammation control, and muscular recovery. In particular, poor posture associated with sedentary habits—such as long hours spent at a computer—can reduce the effectiveness of even the best exercises for shoulder impingement syndrome. Addressing ergonomic setup and taking frequent movement breaks during the day helps support joint alignment and ensures that exercise gains are not undermined by daily habits. Moreover, stress management techniques like breathwork and mindfulness may reduce protective muscle tension around the shoulder, creating a more responsive healing environment.
3. How can shoulder impingement syndrome affect mental health, and what can be done about it?
Chronic pain conditions like shoulder impingement syndrome can significantly impact mood, sleep, and emotional well-being. Frustration from limited mobility, disrupted sleep due to nighttime pain, and anxiety about reinjury are common. To mitigate these effects, cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) have been used effectively alongside exercises for impinged shoulder rehabilitation. These tools can help individuals shift their focus from fear-based avoidance to positive movement patterns, which is vital for long-term recovery. Addressing the emotional toll of injury is just as important as strengthening the rotator cuff.
4. Are there specific training mistakes that often lead to shoulder impingement in athletes?
Yes, one common mistake is failing to balance pushing and pulling exercises in a training routine. Overemphasis on bench presses, overhead lifts, or shoulder presses without adequate scapular retraction and posterior chain work can promote anterior shoulder tightness and dysfunction. Additionally, insufficient warm-up and mobility prep before intense upper-body workouts can increase the risk of developing symptoms. Athletes are encouraged to incorporate the best exercises for shoulder impingement syndrome as prehabilitation tools, not just as part of rehab after symptoms appear. Regular scapular stabilization and rotator cuff conditioning can significantly reduce the likelihood of developing chronic shoulder issues.
5. What role do breathing patterns play in shoulder rehabilitation?
Although often overlooked, dysfunctional breathing patterns can worsen shoulder impingement syndrome. When individuals breathe shallowly using accessory neck and shoulder muscles, it creates chronic tension around the shoulder girdle. Diaphragmatic breathing retrains the core and stabilizes the thoracic spine, indirectly enhancing scapular mobility and upper-body posture. Integrating breath-focused movements with the best exercises for shoulder impingement syndrome can improve coordination and reduce unnecessary strain. This holistic approach enhances not only recovery but also overall nervous system regulation.
6. Can wearable technology help track recovery from shoulder impingement syndrome?
Wearable motion sensors and digital rehab platforms are increasingly being used in musculoskeletal care. These tools provide real-time feedback on posture, range of motion, and exercise accuracy, helping patients stay accountable and make precise adjustments. For people doing exercises for impinged shoulder recovery at home, smart devices can guide them to ensure optimal movement quality. In some cases, motion analysis software can detect compensatory movements that the user may not even be aware of. These innovations make self-guided recovery more effective and reduce the need for constant in-person supervision.
7. How does shoulder impingement differ in older adults compared to younger populations?
In older adults, shoulder impingement syndrome often coincides with degenerative changes like osteoarthritis or partial-thickness rotator cuff tears. This population may present with more stiffness and less muscular resilience, requiring a slower, more cautious exercise progression. However, they still benefit significantly from performing the best exercises for shoulder impingement syndrome, especially when movements are modified for joint protection. In contrast, younger individuals tend to develop impingement from overuse or poor biomechanics during sports or work. Their programs can often progress more aggressively, emphasizing eccentric strength and proprioceptive retraining.
8. Are there long-term maintenance strategies once symptoms have resolved?
Yes, post-rehabilitation maintenance is essential to prevent recurrence. Even after pain subsides, continuing a modified version of the best exercises for shoulder impingement syndrome helps preserve mobility and scapular coordination. Incorporating these movements into a general fitness program at least two to three times per week can keep the shoulder healthy. Additionally, monitoring posture during daily tasks and avoiding prolonged static positions—especially overhead—further reduces reinjury risk. Long-term shoulder wellness also involves periodic check-ins with a physical therapist or movement specialist to catch early signs of dysfunction.
9. Is there a difference between anterior and posterior shoulder impingement when selecting exercises?
Yes, anterior impingement typically involves compression between the acromion and the rotator cuff during forward or overhead movements, whereas posterior impingement often affects athletes during the cocking phase of throwing motions. The selection of exercises for impinged shoulder conditions must reflect this distinction. Anterior impingement responds well to external rotation, scapular stabilization, and postural correction. Posterior impingement may require more attention to internal rotator flexibility and eccentric strengthening in extreme ranges of motion. While both conditions can benefit from the best exercises for shoulder impingement syndrome, tailoring the program to the type of impingement ensures optimal results.
10. What are emerging trends in shoulder impingement rehabilitation?
One emerging trend is the use of virtual reality (VR) environments to gamify rehabilitation and improve adherence. VR programs offer immersive experiences that promote active engagement and proprioceptive training. Another innovation is the integration of AI-assisted motion analysis, which can individualize the progression of exercises for impinged shoulder recovery based on movement efficiency data. Additionally, regenerative medicine techniques—such as platelet-rich plasma (PRP) injections—are being explored as adjuncts to exercise-based therapy. Despite these advances, evidence continues to support that the best exercises for shoulder impingement syndrome remain the most reliable foundation for recovery when guided by skilled clinical oversight.
Conclusion: Embracing Movement to Overcome Shoulder Impingement
Shoulder impingement syndrome can be a frustrating and limiting condition, but it is not insurmountable. Through a structured, evidence-based exercise regimen, individuals can regain mobility, reduce pain, and restore function without the need for invasive procedures. The best exercises for shoulder impingement syndrome emphasize mobility, stability, and strength, progressing from foundational movements to advanced functional integration. By addressing underlying postural issues, improving rotator cuff and scapular control, and embracing a personalized approach to recovery, long-term relief is not only possible—it is sustainable.
Whether you’re an athlete returning to sport, a professional seeking relief from desk-related strain, or someone navigating age-related shoulder stiffness, there are effective exercises for impinged shoulder relief tailored to your needs. With consistency, guidance, and a commitment to movement, recovery is within reach. Embrace the journey, trust your body’s capacity to heal, and stay engaged with strategies that support both immediate relief and lifelong shoulder health.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Shoulder Impingement Exercises: Gentle Moves to Ease Pain and Get Relief


