Arthritis, in its many forms, can transform simple daily tasks into painful challenges. Whether it is osteoarthritis resulting from cartilage breakdown or the autoimmune attacks seen in rheumatoid arthritis, the consequences are often marked by stiffness, inflammation, and a growing sense of physical limitation. Amid various treatment strategies, stretching has emerged as both a complementary therapy and a proactive wellness practice. But does stretching help arthritis in a meaningful, medically supported way? When explored through the lens of physical therapy, rheumatology, and modern exercise science, the answer is more nuanced—and more promising—than many realize.
You may also like : Best Stretches for Sore Legs and Tight Thigh Muscles: How to Relieve Upper Leg Pain Safely and Naturally
Understanding Arthritis and Its Impact on Joint Mobility
To appreciate how stretching can support arthritis relief, it’s crucial to understand the nature of the condition. Arthritis is not a single disease but an umbrella term for more than 100 types of joint disorders, all of which share the common characteristic of joint inflammation. The two most prevalent forms—osteoarthritis and rheumatoid arthritis—differ in cause but share overlapping symptoms such as pain, stiffness, and restricted mobility.
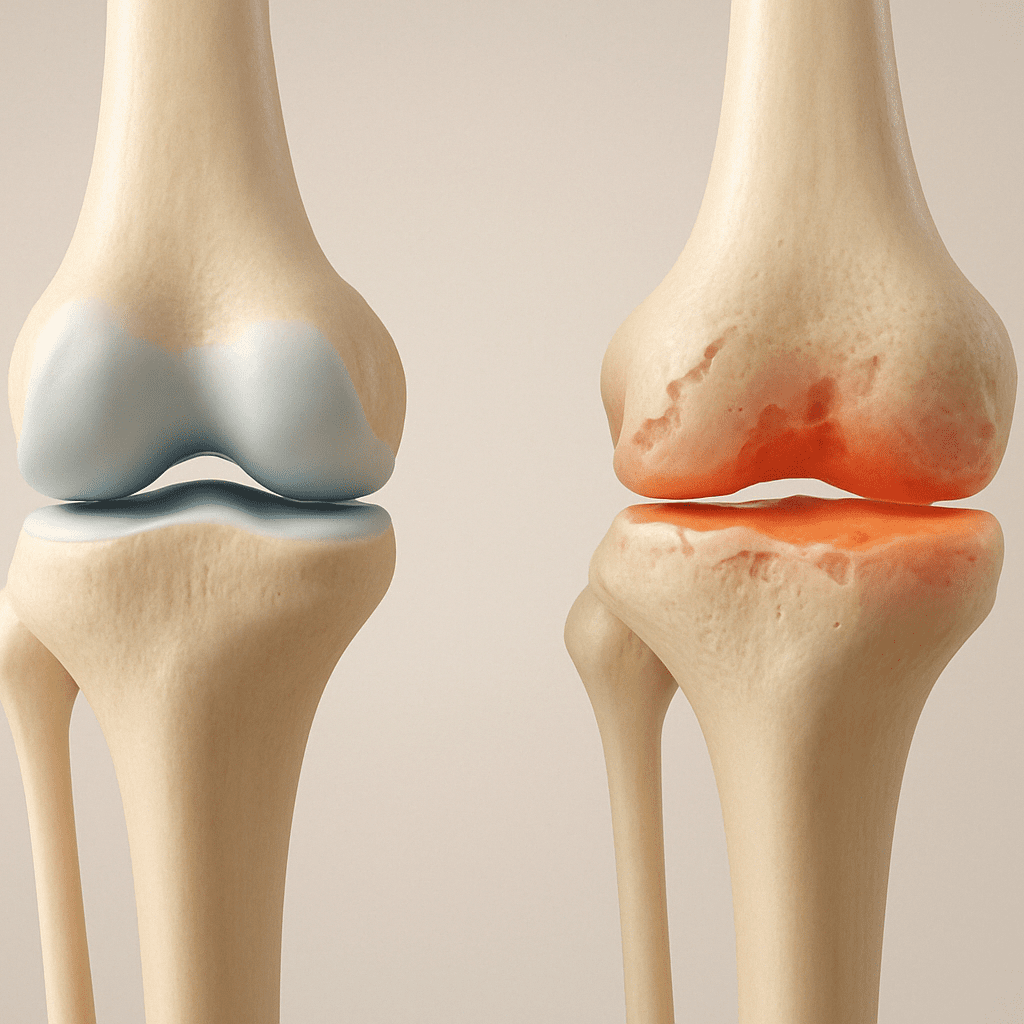
In osteoarthritis, years of wear and tear erode the protective cartilage between bones, leading to bone-on-bone contact. This degeneration triggers pain and inflammation, often in weight-bearing joints like the knees, hips, and lower spine. Rheumatoid arthritis, by contrast, is an autoimmune condition in which the immune system mistakenly attacks joint tissues, causing swelling, pain, and eventual joint deformity. Both forms of arthritis can progressively limit a person’s ability to move, making joint stretching exercises both a preventive and rehabilitative strategy.
Fascial Health and Its Role in Arthritis Flexibility
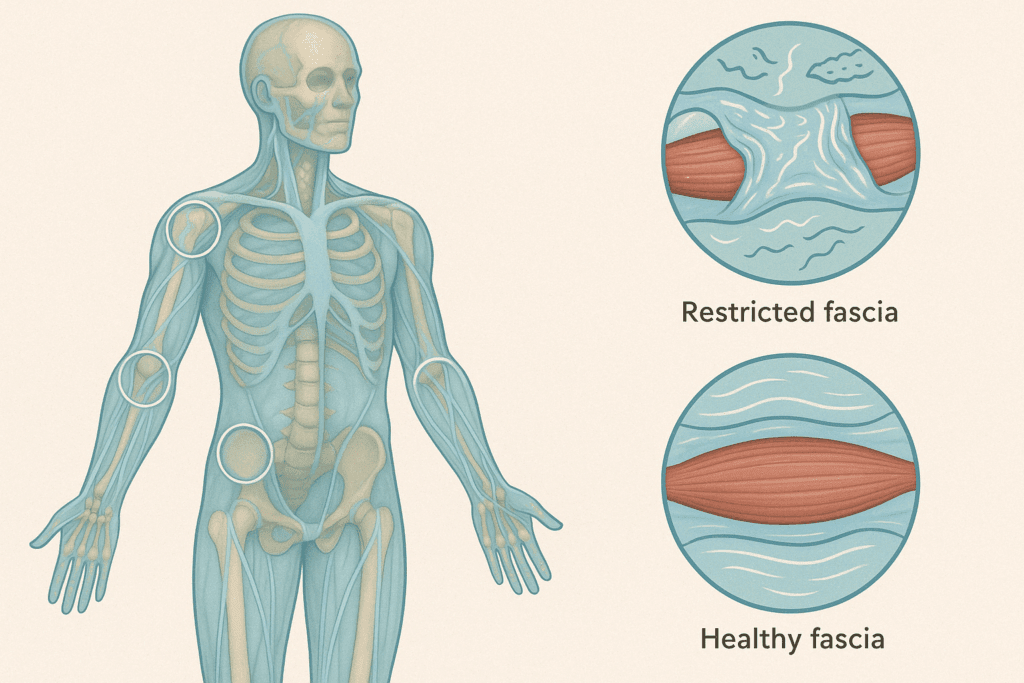
One of the lesser-known but increasingly important aspects of joint flexibility is the role of the fascia—a connective tissue network that envelops muscles, organs, and joints. Fascia is vital for maintaining structural integrity, facilitating movement, and transmitting force across the musculoskeletal system. In people with arthritis, fascial adhesions and restrictions can exacerbate stiffness and limit mobility.
Recent studies have shown that targeted fascial stretching, such as myofascial release techniques, may provide additional relief beyond standard static stretching. These approaches aim to hydrate and decompress the fascia, enhancing tissue glide and joint mobility. Foam rolling, fascial massage, and slow, full-body dynamic movements—such as those found in somatic movement therapy—can complement traditional arthritis stretching routines, particularly in cases where standard joint stretches do not fully address movement limitations.
Why Stretching Matters for Arthritic Joints
Stretching plays a pivotal role in maintaining and improving joint function, especially in arthritic individuals. Regular, targeted stretching can increase synovial fluid circulation, the body’s natural joint lubricant, thereby reducing stiffness and improving range of motion. Unlike high-impact activities that can exacerbate joint pain, arthritis stretching is typically low-intensity and controlled, making it safe for most individuals when performed correctly.
Additionally, stretching can help correct compensatory movement patterns. When one joint becomes stiff or painful, the body naturally adapts, often transferring the load to neighboring joints or muscle groups. Over time, this compensation can result in secondary issues such as muscle imbalances or altered gait mechanics. A well-rounded stretching routine that targets tight or overused muscles can restore more balanced movement and reduce the cumulative strain on vulnerable joints.
Scientific Evidence Behind Stretching for Arthritis Relief
Scientific support for stretching as part of arthritis management has grown steadily over the past two decades. Clinical studies have shown that stretching exercises for arthritis can lead to measurable improvements in pain levels, flexibility, and overall joint function. For example, a randomized controlled trial published in the Journal of Rheumatology found that patients with knee osteoarthritis who followed a structured stretching and strengthening program experienced significantly reduced stiffness and pain compared to a control group.
Further evidence from the Arthritis Foundation and the American College of Rheumatology supports incorporating stretching into daily routines. These organizations recommend stretching as part of a broader physical activity plan tailored to an individual’s condition and limitations. Moreover, emerging research suggests that even short daily sessions of osteoarthritis stretching or rheumatoid arthritis stretching can have cumulative benefits, including reduced reliance on pain medications and improved quality of life.

The Role of Temperature, Hydration, and Biomechanics in Effective Stretching
Environmental and internal conditions can dramatically affect the efficacy of arthritis stretching. For instance, temperature plays a significant role in tissue extensibility. Muscles and tendons stretch more easily when warm, which is why heat therapy—through warm compresses, baths, or heated yoga environments—is often recommended before stretching. Conversely, cold weather may exacerbate stiffness and increase the risk of strain.
Hydration is another critical but underappreciated factor. The fascia, synovial fluid, and even cartilage rely on water for optimal function. Dehydrated tissues are more prone to stiffness and injury. Therefore, maintaining adequate fluid intake supports the body’s ability to stretch and move efficiently.
Biomechanical analysis can also guide personalized stretching programs. Through gait analysis, posture assessment, and motion capture, therapists can identify compensatory movement patterns and joint-loading asymmetries. These insights allow for the creation of bespoke stretching routines that address specific weaknesses or imbalances—making stretching more precise and effective for long-term arthritis management.
Addressing the Unique Needs of Different Demographics
While arthritis can affect people of all ages, genders, and backgrounds, stretching strategies must be adapted to the unique needs of different demographic groups. For instance, older adults may have additional considerations such as balance issues, muscle atrophy, or coexisting conditions like osteoporosis. For this population, stretching should focus on slow, supported movements that reduce fall risk while enhancing joint lubrication and stability.
In younger populations with juvenile idiopathic arthritis (JIA), stretching serves both a rehabilitative and developmental role. Children and adolescents need playful, engaging methods that build body awareness and prevent long-term joint damage. Pediatric physical therapists often integrate stretches into games, sports, or creative movement to keep participation high.
Cultural perceptions of movement and healing also influence stretching practices. In some cultures, community-based movement practices like circle dancing or prayer-based postures provide natural forms of joint mobilization. Recognizing and incorporating these cultural elements can improve compliance and make stretching feel more meaningful and relevant to individuals with arthritis.
The Mechanisms Behind Stretching and Pain Reduction
Understanding how stretching eases arthritis pain involves both physiological and neurological mechanisms. On a mechanical level, stretching gently elongates the muscles and tendons surrounding stiff joints, helping to maintain or increase range of motion. This prevents the shortening of soft tissues—a common problem in people who avoid movement due to discomfort. As flexibility improves, joints are less likely to become impinged or inflamed during everyday tasks.
On a neurological level, stretching activates sensory receptors known as muscle spindles and Golgi tendon organs. These receptors help regulate muscle tone and tension, promoting relaxation and reducing the perception of pain. Furthermore, consistent stretching may modulate central pain processing, helping to “reset” the nervous system’s response to chronic discomfort. These effects, though subtle, can accumulate over time and lead to tangible improvements in joint health.
The Best Types of Stretching for Arthritis Relief
Not all stretching is equally beneficial for arthritic joints. Static stretching, in which a stretch is held for a period of 15 to 60 seconds, is often the safest and most effective method for people with arthritis. These stretches should be performed slowly and never to the point of pain. Dynamic stretching, which involves controlled movements that gradually increase range of motion, may be suitable for some individuals during warm-ups, but should be approached with caution if joints are inflamed.
Proprioceptive neuromuscular facilitation (PNF), a more advanced form of stretching that combines contraction and relaxation phases, can also be beneficial when supervised by a trained physical therapist. Importantly, all joint stretching exercises should be tailored to the individual’s diagnosis, joint involvement, and physical capacity. Working with a professional—such as a physiotherapist or certified arthritis exercise specialist—can ensure that each movement enhances rather than harms joint function.

Stretching Exercises for Arthritis: What to Include
Creating a daily or weekly stretching routine for arthritis begins with identifying key muscle groups associated with commonly affected joints. For osteoarthritis in the knees, stretches that target the quadriceps, hamstrings, calves, and hip flexors can help stabilize and offload the joint. For those with rheumatoid arthritis in the hands or wrists, gentle finger and wrist stretches can preserve dexterity and reduce morning stiffness.
Neck and shoulder stretches are especially helpful for individuals with cervical spine involvement, while lower back stretches—such as the cat-cow pose from yoga—can alleviate spinal stiffness. Across all these areas, slow and consistent practice is more valuable than forceful stretching. The emphasis should always be on gentle elongation, deep breathing, and mindful awareness of bodily feedback. By approaching stretching as a form of body dialogue rather than a mechanical task, individuals can avoid injury and better understand their own limits.

Stretching and Sleep: A Vital Relationship for Arthritis Relief
Quality sleep is essential for tissue repair, immune function, and pain modulation. Unfortunately, many people with arthritis experience sleep disruptions due to discomfort, nocturnal joint pain, or associated mood disorders. Emerging evidence suggests that stretching—especially when performed in the evening—can improve sleep quality and reduce nocturnal symptoms.
Gentle bedtime stretches help transition the nervous system into a parasympathetic state conducive to sleep. They may also release muscular tension that builds up from daytime compensatory movements. Specific poses such as child’s pose, reclined spinal twists, or supine leg stretches are known to soothe the nervous system while gently mobilizing key joints.
When incorporated into a wind-down routine, arthritis stretching becomes part of a holistic strategy for improving sleep and reducing next-day pain and fatigue. This nighttime ritual may also strengthen habit formation, making stretching a natural and sustainable part of daily life.
Incorporating Stretching into a Holistic Arthritis Management Plan
Stretching alone is not a cure for arthritis, but it is a powerful adjunct therapy when integrated into a broader lifestyle approach. Combining joint stretching exercises with strength training, low-impact cardio (such as swimming or cycling), and anti-inflammatory nutrition can lead to synergistic benefits. For instance, improving leg strength through resistance exercises can reduce the load on arthritic knees, while stretching helps maintain mobility and prevents stiffness post-exercise.
Other lifestyle modifications—including weight management, smoking cessation, and stress reduction—also enhance the body’s capacity to respond to arthritis stretching. Chronic stress, for example, can elevate inflammatory markers in the body, undermining the benefits of physical interventions. Practices such as deep breathing, meditation, or gentle yoga can complement stretching routines and reinforce a sense of bodily connection, resilience, and control.
Interdisciplinary Models of Care: Stretching Within Team-Based Arthritis Treatment
Best practices in modern arthritis care involve interdisciplinary collaboration. Rheumatologists, orthopedic specialists, physiotherapists, occupational therapists, dietitians, and mental health professionals all bring valuable insights into the management of chronic joint disease. Within these models, stretching is increasingly recognized as a core element of non-pharmacological intervention.
Multidisciplinary arthritis clinics may offer movement screenings and customized exercise plans, with stretching as a foundational component. Collaborative care models can also integrate psychological support, helping patients overcome fear of movement—a common barrier to adopting stretching routines. When stretching is prescribed and supported across the continuum of care, patients are more likely to adhere and benefit.
This collaborative model also facilitates innovation. By pooling expertise, care teams can experiment with novel combinations of treatments—such as pairing acupuncture with fascial stretching or integrating mindfulness training into stretching programs. These synergies can produce outcomes greater than the sum of their parts, further enhancing arthritis flexibility and function.
Can Stretching Help Arthritis in the Long Run?
One of the most compelling questions for people managing arthritis is whether the benefits of stretching are sustainable. Research and clinical experience both suggest that consistent stretching over weeks and months yields progressively greater improvements in mobility, pain levels, and functional independence. However, sporadic or overly aggressive stretching can do more harm than good.
Long-term success depends not just on frequency but also on form, patience, and personal adaptation. As arthritis evolves—sometimes with periods of flare and remission—stretching routines may need to be adjusted. Consulting regularly with healthcare providers, tracking one’s symptoms, and listening to bodily cues are essential strategies for making stretching a lasting and effective part of arthritis care. In many cases, those who maintain a stretching practice report reduced need for analgesic medications, greater ease in everyday tasks, and an improved overall sense of wellbeing.
Stretching Safety Tips for Arthritis Sufferers
Safety is paramount when introducing new physical routines, particularly for individuals with joint vulnerabilities. Always begin stretching after a gentle warm-up to increase blood flow and reduce muscle tension. Never force a stretch beyond mild discomfort, and avoid ballistic (bouncing) movements, which can strain already compromised tissues.
If a joint is swollen, inflamed, or particularly painful, it’s best to wait until symptoms subside or seek professional guidance. Applying heat before stretching or cold afterward may also help manage pain and inflammation. Hydration is another often-overlooked factor that influences tissue elasticity and joint function—drinking adequate water supports the body’s natural healing and mobility mechanisms. With these precautions in place, arthritis stretching becomes a safe and empowering practice rather than a risk.
The Psychological Benefits of Stretching for Arthritis
While the physical benefits of stretching are well-documented, its psychological effects are equally profound. Chronic pain often leads to anxiety, depression, and a feeling of helplessness. Stretching offers a counter-narrative—a way for individuals to reconnect with their bodies, reclaim agency, and experience moments of relief and mindfulness.
Many people report that the ritual of stretching becomes a meditative practice, anchoring them in the present and reducing pain catastrophizing. This mind-body connection is particularly valuable in rheumatoid arthritis, where flares can be unpredictable and emotionally draining. By establishing a daily habit of self-care through stretching, individuals cultivate resilience and a sense of empowerment that transcends physical symptom management.

Integrating Professional Support and Customized Programs
While some arthritis-friendly stretches can be learned from online resources or classes, a customized program developed by a physical therapist or occupational therapist provides tailored benefits. Such programs account for specific joint involvement, disease stage, comorbidities, and personal preferences. They may also include assistive devices, such as stretch bands or foam rollers, to enhance effectiveness and comfort.
Rehabilitation clinics often provide group stretching sessions that combine physical therapy with social support, creating a sense of community and shared progress. Moreover, programs that integrate stretching with other modalities—such as aquatic therapy or Tai Chi—offer diverse avenues for improving flexibility while minimizing joint strain. These comprehensive approaches underscore that stretching is not an isolated fix, but part of a larger, integrative healing ecosystem.
Frequently Asked Questions (FAQ): Stretching and Arthritis
1. Can arthritis stretching improve long-term joint stability, or is it only effective for short-term relief?
Arthritis stretching does more than provide short-term relief—it plays a crucial role in preserving long-term joint stability. When practiced consistently and thoughtfully, joint stretching exercises help strengthen surrounding muscle groups and enhance neuromuscular control. This stabilization effect is particularly beneficial for joints that are vulnerable to deformation over time, such as those affected by rheumatoid arthritis. Regular movement improves joint alignment and balance, making daily activities easier and reducing compensatory strain on adjacent muscles and joints. In the long run, integrating stretching exercises for arthritis into your daily wellness plan can serve as a proactive safeguard against progressive joint instability.
2. How do arthritis stretching routines differ between osteoarthritis and rheumatoid arthritis patients?
While both conditions benefit from stretching, osteoarthritis stretching typically focuses more on increasing joint lubrication and reducing mechanical stiffness, especially in weight-bearing joints. In contrast, rheumatoid arthritis stretching routines are tailored to accommodate inflammation, joint tenderness, and systemic fatigue. This means the approach to joint stretches must be gentler and often includes longer warm-up periods or mindfulness-based movements to minimize triggering a flare-up. Flexibility programs for rheumatoid arthritis patients might also emphasize hand and wrist mobility, which are frequently impacted. The key is individualization—what works for one form of arthritis may need significant adjustments for another.
3. Does stretching help arthritis in the hands and fingers, or is it only effective for larger joints?
Absolutely, arthritis stretching can be particularly useful for smaller joints like those in the hands and fingers. Joint stretches tailored to the fingers can improve grip strength, preserve fine motor skills, and alleviate morning stiffness—an especially common complaint among those with rheumatoid arthritis. Techniques such as tendon gliding and passive range-of-motion exercises help maintain functionality and reduce discomfort in these delicate areas. When incorporated into a comprehensive care routine that includes joint protection techniques and ergonomic tools, these stretching exercises for arthritis in the hands can significantly improve quality of life. Importantly, hand-based stretches should be approached with as much care and consistency as those for larger joints.
4. Are there any advanced or technology-assisted tools that enhance arthritis stretching effectiveness?
Yes, technological advances have made arthritis stretching more accessible and effective. Devices like smart resistance bands, motion-tracking wearables, and interactive stretching apps offer biofeedback, helping users refine their form and track progress. Some digital platforms now incorporate adaptive algorithms that adjust routines based on real-time pain or flexibility feedback. These tools can be especially valuable for those with limited mobility who may not always be able to attend in-person therapy sessions. By combining innovation with evidence-based routines, these solutions make joint stretching exercises more precise and personalized, which is especially helpful for individuals navigating the variable nature of arthritis symptoms.
5. Is stretching good for arthritis during flare-ups, or should it be avoided until symptoms subside?
Whether stretching is appropriate during flare-ups depends on the type and severity of the arthritis symptoms. Gentle movements, such as slow passive joint stretches or breath-synchronized stretches from restorative yoga, may actually help reduce inflammation and promote circulation. However, aggressive or high-intensity arthritis stretching should be avoided during flare-ups to prevent aggravating already sensitive tissues. Listening to the body is key—if a stretch causes sharp or prolonged pain, it’s best to pause or modify the approach. In many cases, using heat before stretching or incorporating stress-reducing practices like guided breathing can make stretching more tolerable and beneficial, even during mild flare-ups.
6. Can stretching help arthritis by reducing the need for medication over time?
For some individuals, consistent arthritis stretching may reduce their reliance on certain medications—particularly non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants. By improving joint flexibility and reducing muscular tension, stretching addresses one of the root contributors to arthritis discomfort: mechanical stiffness. In clinical settings, stretching exercises for arthritis are often included as part of broader physical therapy programs that aim to enhance function and minimize pharmacological side effects. While stretching alone may not eliminate the need for medication, it can serve as a complementary tool that empowers individuals to manage pain more naturally. Patients should always consult their healthcare provider before adjusting any medication regimen, but the potential for reduced dependency through movement is well-supported.
7. What role does hydration play in maximizing the benefits of arthritis stretching?
Hydration is often overlooked, yet it significantly impacts the effectiveness of joint stretching exercises. Adequately hydrated tissues are more pliable, which allows for smoother, safer stretching with reduced risk of strain. For people with arthritis, especially those engaging in osteoarthritis stretching routines, hydration supports synovial fluid production—the natural lubricant of the joints. Moreover, well-hydrated fascia, tendons, and muscles respond more positively to elongation, reducing post-stretch soreness. Incorporating hydration into your stretching plan isn’t just about drinking more water—it’s about optimizing your body’s responsiveness to movement and maintaining joint health at a cellular level.
8. How can joint stretching exercises support emotional well-being in people with arthritis?
Stretching can have a profound effect on mental health, offering emotional relief in addition to physical benefits. For individuals coping with chronic conditions like rheumatoid arthritis, stretching fosters a sense of agency and reduces feelings of helplessness. Regular stretching practices—especially those incorporating breathwork or meditative elements—can calm the nervous system and lower stress-related inflammation. This psychophysiological link means that stretching exercises for arthritis may indirectly influence mood, energy levels, and sleep quality. Over time, this holistic benefit becomes a crucial pillar in managing both the physical and emotional dimensions of arthritis.
9. Are joint stretches beneficial for individuals with both arthritis and other mobility-limiting conditions like fibromyalgia or neuropathy?
Joint stretching exercises can be adapted for people managing arthritis alongside coexisting conditions like fibromyalgia or peripheral neuropathy. These individuals often experience widespread pain or nerve-related discomfort, which requires a particularly gentle and intuitive approach. Stretching that emphasizes myofascial release, slow rhythmic motion, or breath-coordinated techniques can help ease tension without triggering additional pain. Moreover, many of the same routines used in arthritis stretching can be cross-applied—with modifications—to support tissue health and nervous system regulation. Multimorbidity doesn’t have to be a barrier; in fact, stretching can serve as a unifying practice that addresses overlapping symptoms across conditions.
10. What are the future directions or innovations in arthritis stretching therapies?
The future of arthritis stretching lies in personalized, tech-integrated, and interdisciplinary approaches. Researchers are exploring how neuromuscular retraining and virtual reality-assisted movement can reshape the brain’s response to chronic pain, potentially revolutionizing how we view stretching. On the clinical side, new forms of dynamic osteoarthritis stretching are being developed that integrate resistance and proprioceptive training. Additionally, AI-guided platforms that monitor biomechanical feedback are becoming more sophisticated, enabling highly customized routines based on individual joint profiles. As more data accumulates from wearable tech and real-time motion analytics, stretching exercises for arthritis will likely evolve into precision therapies tailored not just to the disease, but to each person’s unique experience with it.
Conclusion: Embracing Joint Stretches as a Lifelong Ally Against Arthritis
So, is stretching good for arthritis? The evidence points to a clear and confident yes—when performed safely, consistently, and in accordance with individual needs. Joint stretching exercises help reduce stiffness, improve mobility, and counteract the physical limitations imposed by osteoarthritis and rheumatoid arthritis alike. They offer not only mechanical benefits to the joints but also psychological solace and a sense of regained control.
While stretching exercises for arthritis are not a cure, they form a cornerstone of holistic arthritis care. They blend seamlessly with strength training, healthy lifestyle practices, and medical treatment plans. Whether you’re newly diagnosed or have lived with arthritis for years, incorporating arthritis stretching into your daily routine can transform how you move, feel, and live.
Ultimately, the question should not just be “Can stretching help arthritis?” but rather, “How can I make stretching a sustainable, meaningful part of my arthritis journey?” With the right mindset, guidance, and consistency, stretching becomes more than a physical routine—it becomes a powerful act of self-care and resilience in the face of chronic joint disease.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Yin Yoga for Arthritis: 10 poses to ease your pain


