Caring for a loved one with Alzheimer’s or another form of dementia can be deeply rewarding, but it often comes with unique and complex challenges. Among the most distressing behaviors for caregivers is agitation, which may manifest as restlessness, aggression, irritability, or repetitive actions such as pacing. These behaviors can escalate, particularly in the late afternoon or evening, a phenomenon known as “sundowning.” Learning how to calm an agitated dementia patient requires not only patience and compassion but also an understanding of the underlying causes of agitation in dementia. Through evidence-based approaches and insights from healthcare professionals, caregivers can adopt effective techniques to create a more peaceful, supportive environment.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding Agitation in Dementia: Causes and Clinical Perspectives
Agitation in dementia is not a random or inexplicable occurrence. Instead, it often signals discomfort, unmet needs, or confusion. Clinical studies have shown that environmental changes, physical pain, sleep disturbances, and communication barriers are among the most common triggers. The person experiencing dementia may be unable to articulate their distress, resulting in behaviors that are misconstrued as aggressive or disruptive. It is crucial to reframe agitation as a form of communication, particularly when verbal expression becomes limited.
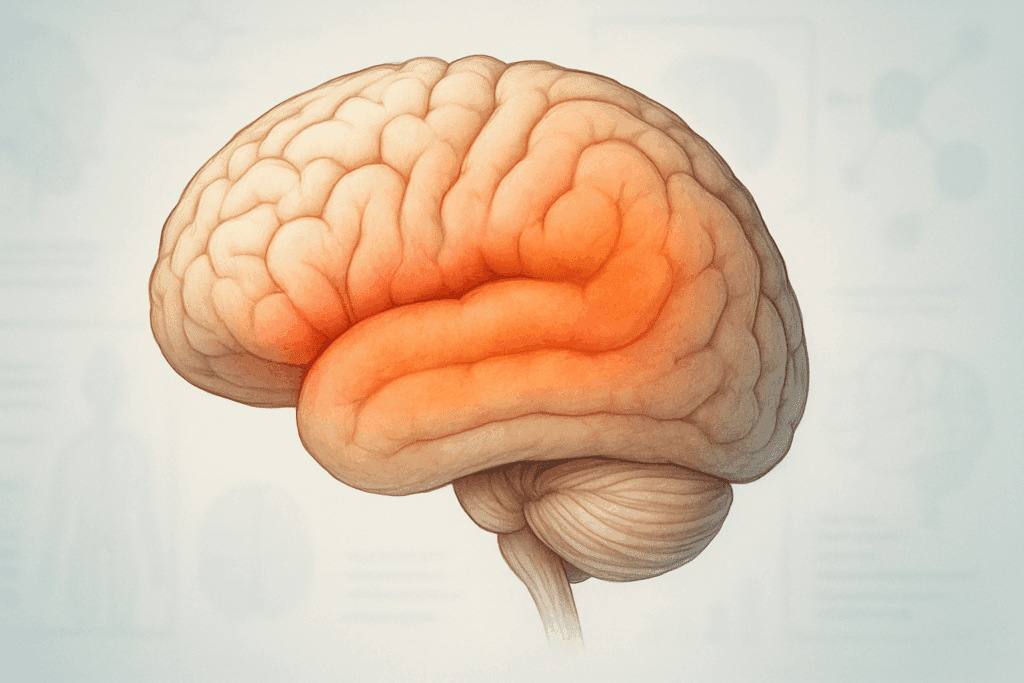
From a neurological standpoint, agitation in elderly individuals with dementia can be linked to changes in brain function, particularly in the frontal and temporal lobes, which govern emotional regulation and impulse control. These alterations can make individuals more prone to frustration and less able to manage stimuli. The decline in memory and reasoning skills compounds the issue, as disorientation and confusion lead to a heightened sense of vulnerability and fear. Therefore, managing agitation requires not just addressing the behavior but understanding its root causes.
Healthcare professionals emphasize a personalized approach. What triggers agitation in one dementia patient may have no effect on another. Observing patterns and recognizing environmental or interpersonal triggers can provide invaluable clues. Whether it’s a change in routine, an unfamiliar face, or something as subtle as background noise, these factors can have a profound impact on a person with cognitive impairment. Recognizing these influences is a cornerstone of developing an effective intervention strategy.

Creating a Calming Environment: Sensory and Emotional Cues
One of the most powerful tools in managing agitation is the environment itself. Because individuals with dementia are often hypersensitive to sensory stimuli, a chaotic or overstimulating space can contribute significantly to their distress. Creating a calming environment involves both physical and emotional dimensions. On the physical side, soft lighting, minimal clutter, and muted colors can reduce cognitive overload. Soundscapes with gentle music or nature sounds can have a soothing effect, while excessive noise from televisions or multiple conversations should be minimized.
Emotional ambiance is equally important. Individuals with dementia are remarkably perceptive of tone, facial expressions, and body language. Caregivers should strive to convey a sense of calm and reassurance through slow movements, gentle touch, and a soothing tone of voice. Eye contact and relaxed facial expressions signal safety and trust. Research supports the notion that when caregivers maintain a composed demeanor, the patient often mirrors that emotional state.
It is also vital to consider the role of personal items in fostering comfort. Familiar objects, photographs, or even a favorite blanket can provide a grounding sense of identity and security. These items serve as emotional anchors that help reduce the disorientation that often fuels agitation. This approach is especially effective during episodes of pacing and Alzheimer’s-related restlessness, offering tactile and visual cues that promote a sense of belonging and calm.

Communication Techniques to De-Escalate Agitation
Knowing how to calm an agitated dementia patient also requires mastery of specialized communication techniques. Because verbal comprehension may be impaired, caregivers must adapt their speech to be clear, concise, and reassuring. Short sentences, simple words, and a slow, steady cadence are more likely to be understood and accepted. Avoiding open-ended questions can help prevent confusion; instead, offer choices between two simple options.
Non-verbal communication becomes increasingly important. Touch, gestures, and eye contact can be more effective than words in conveying empathy and reassurance. Physical closeness should be approached with sensitivity—some individuals may find it comforting, while others may interpret it as intrusive. Always approach from the front, announce your presence, and allow the person time to process and respond.
Redirection is another effective technique for managing agitation in elderly individuals with dementia. If the person becomes fixated on a distressing thought or begins to pace repetitively, gently shifting their focus to a different activity—such as looking at photos, folding towels, or listening to music—can provide relief. Timing and tone are crucial; the goal is to redirect without invalidating their experience or appearing dismissive. A calm, validating statement followed by a new suggestion can help achieve this balance.

Understanding Pacing and Alzheimer’s: When Movement Signals a Need
Pacing is a common manifestation of agitation in dementia and is often misunderstood as simply a nervous habit. In reality, pacing in Alzheimer’s and other forms of dementia can be a meaningful behavior that expresses unmet needs, such as discomfort, boredom, or a desire for physical activity. While it can be concerning for caregivers, especially if safety becomes an issue, it is important to recognize pacing as a form of communication rather than a symptom to suppress.
Some individuals may pace to relieve physical restlessness, particularly if they are confined for extended periods. Others may be searching for something familiar, whether a person, a place, or a memory. In some cases, pacing reflects anxiety triggered by environmental stimuli or internal confusion. Rather than attempting to halt the behavior, caregivers can create safe walking paths within the home, providing a controlled environment that allows for expression without risk.
Intervening appropriately requires discernment. If pacing escalates into agitation or appears to be driven by distress, redirecting the individual to a more calming activity may be beneficial. On the other hand, if the pacing appears to be benign and self-soothing, it may be best to simply observe and ensure the environment is safe. In either case, understanding the emotional context behind the behavior can guide an appropriate and empathetic response.

How to Calm Dementia Patients at Night: Managing Sundowning and Sleep Disruptions
Nighttime can be particularly challenging for individuals with dementia and their caregivers. The phenomenon known as “sundowning” refers to increased agitation, confusion, and restlessness that often occur in the late afternoon or evening. This pattern can severely disrupt sleep and increase caregiver stress, making it critical to understand how to calm dementia patients at night.
Establishing a consistent bedtime routine is one of the most effective strategies for managing nocturnal agitation. A predictable schedule helps reduce anxiety and signals to the body that it is time to wind down. Gentle, calming activities such as listening to soft music, reading aloud, or offering a warm beverage (caffeine-free) can help facilitate this transition. Bright lights should be dimmed, and any overstimulating stimuli should be removed from the environment.
Addressing the physiological causes of nighttime agitation is equally important. Pain, hunger, urinary urgency, or side effects from medications can all disrupt sleep and increase confusion. Ensuring that basic needs are met before bedtime can prevent unnecessary awakenings. Some caregivers find that placing a nightlight in the room can help reduce disorientation if the patient wakes during the night.
Melatonin and other non-pharmacological sleep aids have been explored as gentle interventions for sleep disturbances in dementia. However, any supplement or medication should be discussed with a healthcare provider. Behavioral interventions are often preferred as first-line strategies. By combining a structured routine with emotional support, caregivers can significantly reduce nighttime agitation in elderly patients with dementia.
Effective Interventions for Agitation in Elderly Treatment Plans
Medical and non-medical strategies both play critical roles in treating agitation in elderly individuals with dementia. A comprehensive approach often begins with identifying and addressing any underlying physical or psychological issues. Infections, dehydration, constipation, and unrecognized pain are all common contributors to behavioral disturbances. Routine health assessments are vital for early detection and intervention.
Non-pharmacological interventions remain the cornerstone of agitation management. Activities that provide sensory stimulation, cognitive engagement, or opportunities for expression can be highly beneficial. Art therapy, music therapy, and pet therapy have demonstrated positive effects on mood and behavior. These approaches help fulfill emotional and psychological needs that might otherwise be expressed through agitation.
When behavioral approaches are insufficient, healthcare providers may consider pharmacological treatment. However, the use of antipsychotic medications or sedatives must be approached with caution due to the risk of serious side effects, including increased risk of stroke or mortality in elderly patients with dementia. These medications should only be used when the individual poses a risk to themselves or others and should be monitored closely by medical professionals.
Caregiver training is another essential component of treatment. Equipping caregivers with tools to recognize early warning signs, de-escalate tension, and implement calming strategies can dramatically improve outcomes. Emotional support for caregivers, including counseling and respite care, helps sustain their ability to provide effective and compassionate care over the long term.

Supporting the Emotional Well-Being of Caregivers and Patients Alike
Agitation in dementia not only affects the individual but also has profound emotional and physical effects on caregivers. The constant vigilance, emotional strain, and disrupted sleep can lead to burnout, anxiety, and depression. Acknowledging the challenges of caregiving and prioritizing caregiver well-being is essential for the sustainability of care.
Support groups, both in-person and online, offer a valuable outlet for sharing experiences and learning from others in similar situations. These groups can reduce the sense of isolation that many caregivers feel and provide practical strategies for coping. Counseling or therapy can also help caregivers process complex emotions, especially when confronting feelings of guilt, frustration, or grief.
Practicing self-care is not a luxury but a necessity. Caregivers should carve out regular time for rest, hobbies, social interaction, and medical checkups. Engaging in mindfulness practices, such as deep breathing, meditation, or yoga, can provide mental clarity and reduce stress. When caregivers are well-supported, their capacity to respond calmly and effectively to agitation in dementia patients improves significantly.
Building a Supportive, Dementia-Friendly Environment for Long-Term Care
The journey of dementia caregiving is not a sprint but a marathon. Creating a supportive, dementia-friendly environment involves ongoing adjustments as the disease progresses. Flexibility, observation, and a willingness to learn are indispensable traits for caregivers. Over time, recognizing patterns of behavior, identifying triggers, and refining intervention strategies become second nature.
Technology can also play a supportive role. Motion sensors, GPS trackers, and remote monitoring devices can help ensure safety while preserving a sense of independence for the patient. Adaptive clothing, accessible home layouts, and visual cues (such as signs or color-coded labels) can further enhance comfort and orientation.
Community-based resources such as adult day programs, memory cafes, and respite care services offer structured environments that can reduce agitation and promote engagement. These services not only benefit the person with dementia but also provide critical relief for caregivers, allowing them to recharge and avoid exhaustion.
Healthcare professionals, social workers, and dementia care specialists can assist families in developing customized care plans. Regular consultations and check-ins ensure that interventions remain appropriate and effective. A collaborative approach that includes medical, emotional, and practical support creates the strongest foundation for managing agitation and promoting quality of life.
Frequently Asked Questions: How to Calm an Agitated Dementia Patient
1. What role does hydration play in managing agitation in dementia?
Hydration is often overlooked as a factor in behavioral changes, but it can significantly influence agitation in dementia. Dehydration may lead to confusion, fatigue, and irritability, exacerbating cognitive symptoms and making patients more prone to episodes of restlessness or aggression. Especially in elderly individuals, the sensation of thirst diminishes, making them less likely to self-regulate fluid intake. For caregivers learning how to calm agitated dementia patients, offering small sips of water or electrolyte-rich fluids throughout the day may help prevent behavioral escalation. This subtle but proactive measure complements other agitation in elderly treatment strategies by addressing an easily modifiable physical cause.
2. Can specific scents help reduce agitation and pacing in Alzheimer’s patients?
Aromatherapy is emerging as a promising tool in managing agitation in dementia, particularly when it comes to pacing and Alzheimer’s-related restlessness. Calming scents like lavender, bergamot, and chamomile may promote relaxation through olfactory stimulation, engaging the limbic system and triggering emotional responses associated with calmness. Using diffusers or scented lotions during peak times of anxiety can subtly influence mood without direct confrontation or stimulation. For those exploring how to calm dementia patients at night, introducing calming scents in the evening may also improve sleep hygiene. Although not a standalone solution, aromatherapy can be a gentle and non-invasive part of a comprehensive care plan.
3. Is it helpful to involve patients in simple decision-making during agitation?
Involving individuals in minor decisions can be an effective de-escalation tactic during episodes of agitation in elderly patients. Even when cognitive function is compromised, having a sense of control over one’s environment can reduce frustration. Questions like “Would you like tea or juice?” or “Shall we sit here or by the window?” promote autonomy without overwhelming the person with complex choices. This technique works especially well when trying to redirect pacing and Alzheimer’s-driven behaviors into more structured, peaceful alternatives. When caregivers incorporate this practice into their approach to how to calm agitated dementia patients, it often results in more cooperative and less confrontational interactions.
4. How can seasonal changes impact agitation in elderly individuals with dementia?
Seasonal changes, particularly the shift to shorter days and longer nights, can exacerbate agitation in elderly populations. Disruption in circadian rhythms may increase confusion and contribute to behaviors like pacing and agitation in dementia patients. This phenomenon is closely related to sundowning, where symptoms intensify during the late afternoon or evening. To counteract this, caregivers might consider using full-spectrum light therapy to simulate natural daylight, which can support a more stable sleep-wake cycle. Understanding how environmental changes influence behavior is essential for anyone aiming to refine their strategy for how to calm dementia patients at night and throughout the year.
5. What impact does caregiver emotional state have on dementia-related agitation?
A caregiver’s emotional tone and demeanor profoundly affect agitation in elderly patients with dementia. People with dementia often respond to nonverbal cues even more than to spoken language, meaning they are highly attuned to tension, stress, or frustration in others. If a caregiver approaches in a rushed or anxious manner, the patient may mirror those emotions, escalating the situation. Conversely, a calm, measured tone and slow, deliberate movements can serve as powerful tools when determining how to calm agitated dementia patients. Training in mindfulness and stress-reduction techniques is increasingly being incorporated into agitation in elderly treatment protocols to enhance caregiver resilience and emotional regulation.
6. Are dietary patterns associated with increased or decreased episodes of agitation?
Yes, dietary habits may influence the frequency and severity of agitation in dementia. Sudden spikes and crashes in blood sugar can lead to mood swings, irritability, and fatigue, potentially triggering episodes of agitation in elderly individuals. Meals rich in protein, fiber, and healthy fats help stabilize blood glucose and promote sustained energy throughout the day. Additionally, reducing processed foods, excess sugar, and stimulants like caffeine can minimize behavioral volatility. Implementing consistent meal schedules may also reduce confusion and anxiety, reinforcing how strategic dietary choices can support efforts to calm dementia patients at night and during the day.
7. Can music therapy reduce pacing behaviors in Alzheimer’s disease?
Music therapy has shown considerable promise in alleviating pacing and Alzheimer’s-related agitation. Familiar music often evokes positive memories and emotions, fostering a sense of connection and reducing feelings of isolation. Rhythmic music, in particular, can provide structure and predictability, which may reduce compulsive pacing and other repetitive behaviors. Incorporating music into daily routines, especially during known agitation periods, offers a low-risk and highly personalized intervention. For caregivers learning how to calm agitated dementia patients, music therapy presents an evidence-supported option that blends emotional resonance with therapeutic structure.
8. What should caregivers avoid when trying to manage agitation in dementia?
When responding to agitation in dementia, certain well-meaning actions can inadvertently escalate the situation. These include arguing, correcting the patient’s memory, or using complex reasoning to explain why something is happening. Additionally, excessive stimulation—such as bright lights, loud voices, or crowded spaces—can worsen behaviors associated with agitation in elderly individuals. Caregivers should also avoid physical restraint unless absolutely necessary for safety, as it often increases fear and resistance. Instead, a compassionate, patient approach with minimal confrontation aligns better with long-term strategies for how to calm agitated dementia patients.
9. Is nighttime agitation a sign of sleep disorder in dementia patients?
While nighttime agitation can stem from sundowning, it may also signal an underlying sleep disorder such as sleep apnea, restless leg syndrome, or REM sleep behavior disorder. These conditions are more common in elderly populations and often coexist with dementia. If behavioral strategies fail to reduce nighttime agitation, a sleep study might be warranted to rule out medical causes. Recognizing the difference between behavioral agitation and sleep pathology is critical for caregivers trying to determine how to calm dementia patients at night. Proper diagnosis can lead to tailored treatments that significantly improve quality of life for both the patient and caregiver.
10. What are emerging innovations in agitation in elderly treatment?
Recent advances in agitation in elderly treatment include wearable biosensors that monitor physiological stress markers, enabling real-time detection of agitation before it escalates. Artificial intelligence tools are also being developed to analyze patterns in behavior and environment to predict when agitation is likely to occur. Additionally, virtual reality interventions are being explored as immersive experiences to reduce anxiety and pacing behaviors in Alzheimer’s care. These technologies complement traditional methods by offering proactive, personalized care. For those exploring new frontiers in how to calm agitated dementia patients, these innovations hold promise for transforming both diagnosis and treatment strategies in the near future.
Embracing Compassionate Strategies for Calming Agitation in Dementia
Learning how to calm an agitated dementia patient is not a matter of mastering a single technique, but of cultivating a compassionate, flexible, and informed approach to care. Understanding the multifaceted causes of agitation in dementia—from neurological changes to environmental stressors—allows caregivers to respond with empathy and effectiveness. Whether dealing with pacing and Alzheimer’s behaviors, managing nighttime restlessness, or exploring options for agitation in elderly treatment, the key lies in recognizing behaviors as meaningful expressions of need.
Rather than reacting with frustration or alarm, caregivers can create an atmosphere of safety and trust through consistency, clear communication, and environmental comfort. Empowering caregivers with knowledge and support strengthens their ability to respond with confidence, reducing both distress for the patient and emotional strain for themselves. The path of dementia caregiving is undeniably demanding, but it is also an opportunity to offer profound dignity, love, and respect during one of life’s most vulnerable chapters. By embracing a holistic, patient-centered approach, we can help ensure that those living with dementia receive care that honors their humanity and soothes their unrest.
Further Reading:
How to Calm Agitated Dementia Patient
Calming the Agitated Patient: Providing Strategies to Support Clinicians
Agitation in Dementia: Causes, Symptoms, and Management Guide


