In the growing landscape of neurodegenerative conditions, few diagnoses provoke as much emotional gravity as dementia. Affecting over 55 million people globally, dementia not only disrupts memory and reasoning but also slowly unravels personality, independence, and emotional regulation. As families grapple with the complexities of care, one of the most pressing questions inevitably emerges: What is the best medication for dementia? Despite ongoing advances in neuroscience, there is no definitive cure. However, a variety of dementia treatments have shown promise in slowing progression, managing symptoms, and enhancing quality of life. Understanding the pharmacological landscape—including the most widely used memory drugs, new therapies on the horizon, and how medications are selected for each stage—is essential for navigating this condition with hope, clarity, and scientific grounding.
At the heart of this inquiry is not merely a search for symptom control, but a deeper desire to preserve identity, autonomy, and emotional well-being in the face of cognitive decline. In this article, we’ll explore the most effective and evidence-backed dementia medications available today. We’ll examine how drugs for dementia are chosen, how they interact with the brain, and what the scientific literature says about their efficacy. Additionally, we’ll uncover how clinicians combine therapies—such as using Exelon with Namenda to help with anxiety—and how these regimens vary depending on the dementia subtype and stage. The goal is to offer an authoritative yet accessible guide to those seeking answers about the best treatments for memory impairment.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding the Nature of Dementia and the Role of Medication
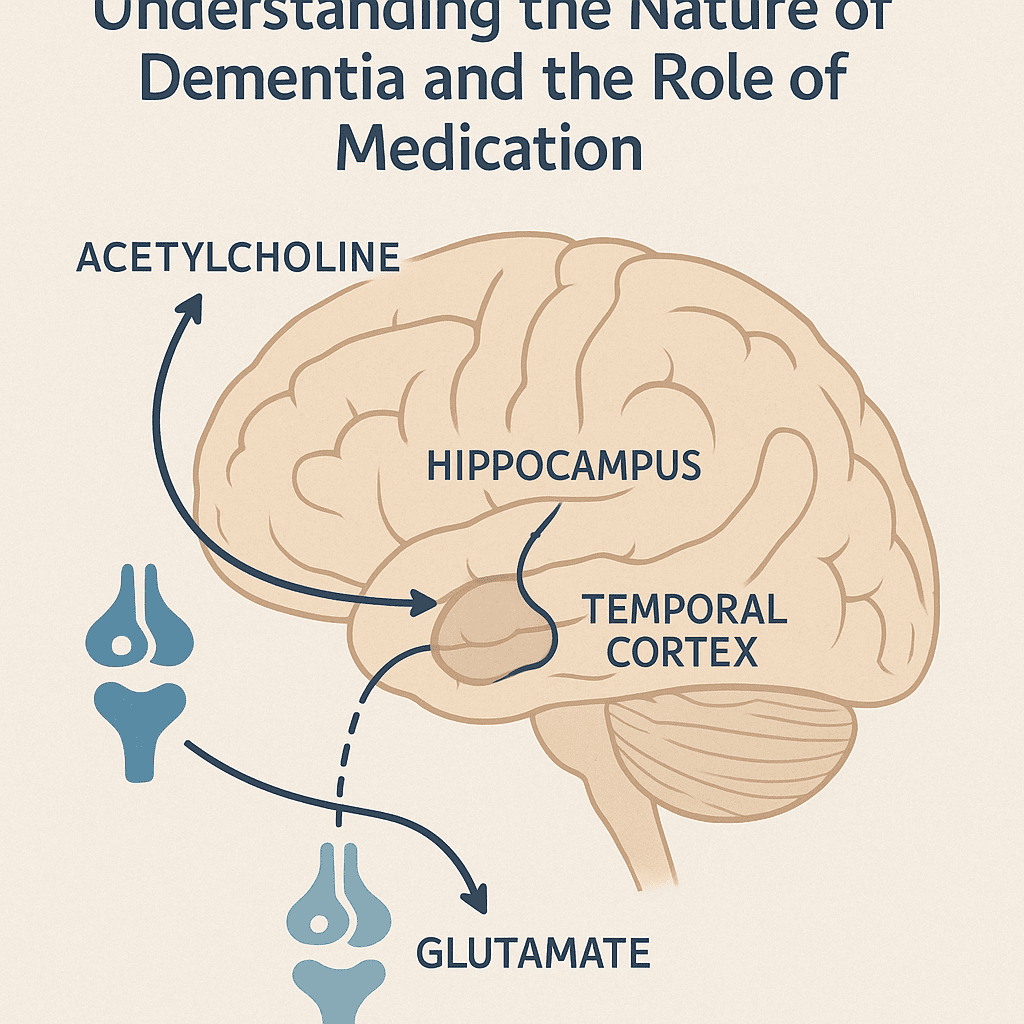
Before examining specific dementia medications, it’s important to recognize the biological underpinnings of this condition. Dementia is not a single disease, but an umbrella term encompassing several disorders, the most common of which is Alzheimer’s disease. Other forms include vascular dementia, Lewy body dementia, and frontotemporal dementia, each with its own distinct neuropathology. Despite their differences, these conditions often share overlapping symptoms: memory loss, confusion, mood changes, and difficulty with language or problem-solving. Because dementia arises from progressive neuronal damage, the goal of pharmacological intervention is not to reverse this damage, but to modify symptoms, support cognition, and in some cases, slow progression.
Is dementia treatable? While it cannot currently be cured, many medications for memory impairment can offer meaningful improvements, especially when initiated early. That said, the effectiveness of any memory medication is often highly individualized. Factors such as the type of dementia, coexisting medical conditions, and patient-specific symptoms play critical roles in determining the optimal therapeutic path. The phrase “what helps dementia” can have different meanings depending on whether the priority is to enhance memory, stabilize mood, reduce anxiety, or manage sleep disturbances. Thus, while no pill offers a panacea, certain dementia pills have become mainstays in clinical treatment due to their proven benefits and tolerability.
Cholinesterase Inhibitors: The Foundation of Early Dementia Treatment
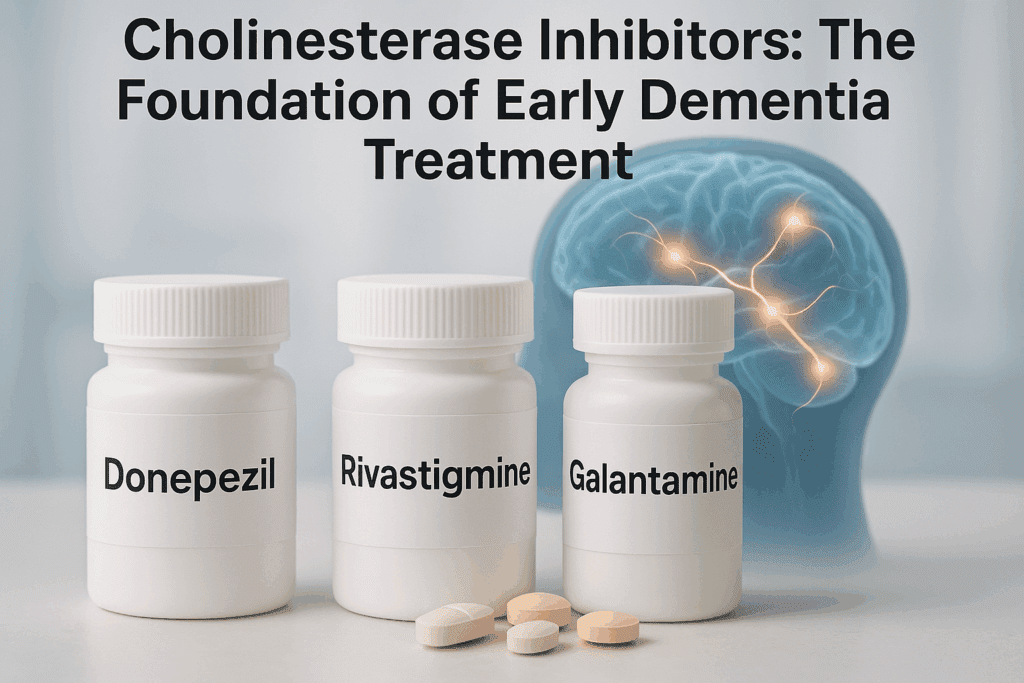
Among the earliest and most widely prescribed dementia medications are cholinesterase inhibitors—a class of drugs that include donepezil (Aricept), rivastigmine (Exelon), and galantamine (Razadyne). These medications work by boosting levels of acetylcholine, a neurotransmitter critical for memory, attention, and learning. As dementia progresses, acetylcholine levels diminish, which correlates with worsening symptoms. By preventing the breakdown of this chemical messenger, cholinesterase inhibitors can enhance neural communication and support cognitive function in the early to moderate stages of dementia.
Donepezil, in particular, is often considered one of the best drugs for dementia during the initial phase of Alzheimer’s disease. It is usually well tolerated, with side effects like nausea and dizziness occurring in a minority of patients. Rivastigmine, available in both oral and transdermal patch forms, is another go-to option. Interestingly, combining Exelon with Namenda to help with anxiety and cognitive decline is a strategy sometimes employed when dual symptom management is required. This multi-modal approach can be particularly beneficial for individuals who experience both cognitive and emotional symptoms.
Although cholinesterase inhibitors do not halt disease progression, they can provide months to years of improved function and stability. For many families, these gains—however incremental—translate into more meaningful interactions, delayed institutionalization, and preserved dignity. For this reason, these medications remain among the most commonly used dementia therapies worldwide.
NMDA Receptor Antagonists: Enhancing Cognitive Function in Moderate to Severe Stages
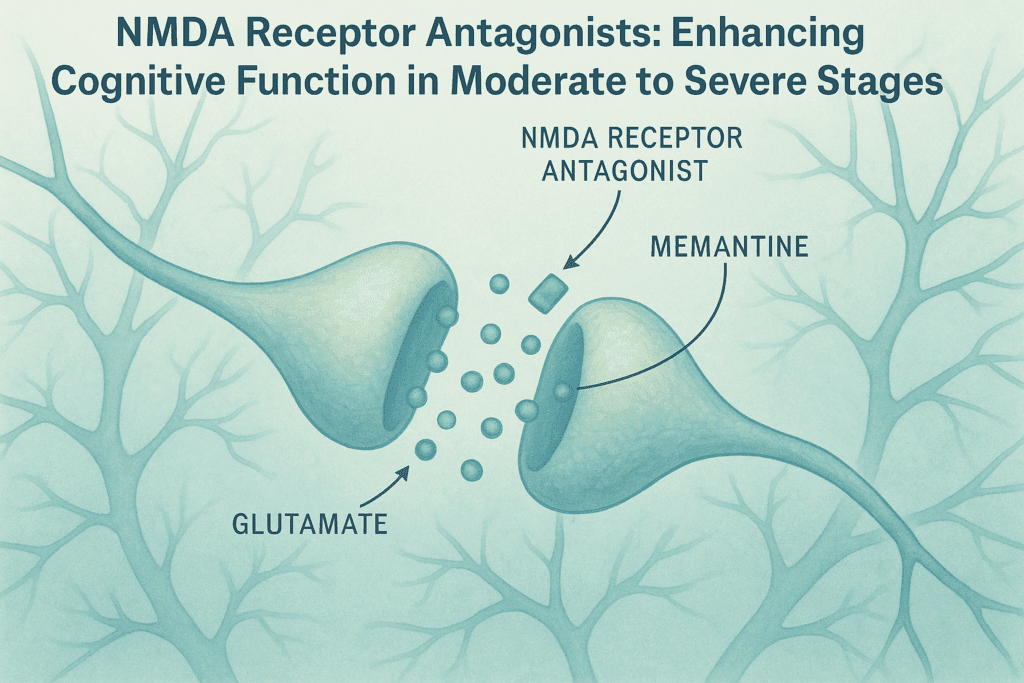
As dementia advances, especially into moderate or severe stages, another class of medications becomes more relevant: NMDA receptor antagonists. The most prominent drug in this group is memantine (Namenda), which regulates glutamate activity in the brain. Glutamate is essential for learning and memory, but excessive amounts can lead to excitotoxicity—a process in which neurons are damaged due to overstimulation. By modulating glutamate’s effects, memantine helps protect neurons while also enhancing cognition and behavioral regulation.
So, what stage of dementia is memantine used for? Typically, memantine is prescribed for individuals with moderate to severe Alzheimer’s or other advanced dementias. It is often added to an existing cholinesterase inhibitor, creating a dual-therapy approach that targets two distinct neurotransmitter systems. This combination—such as Exelon with Namenda to help with anxiety and memory impairment—has been shown in clinical trials to improve daily functioning and reduce behavioral disturbances.
Memantine is also favored for its tolerability. Unlike some dementia pills that can cause gastrointestinal upset or bradycardia, memantine has a relatively benign side effect profile, with dizziness and headache being the most commonly reported issues. For patients experiencing confusion, irritability, or wandering behaviors, this medication may offer not only cognitive support but also behavioral stabilization.
Emerging Therapies: What Is the Best Drug to Improve Memory?
With ongoing advances in neuropharmacology, researchers continue to investigate novel compounds aimed at halting or reversing neurodegeneration. Among the latest memory drugs under scrutiny are monoclonal antibodies targeting amyloid plaques and tau tangles—hallmarks of Alzheimer’s pathology. Aducanumab and lecanemab, both approved by the FDA with some controversy, aim to remove these protein deposits from the brain. While their clinical efficacy is still debated, these medications represent a significant shift toward disease-modifying dementia treatments rather than symptomatic management alone.
Still, when asking what is the best drug to improve memory, it’s essential to weigh both clinical data and real-world outcomes. Medications like aducanumab may reduce biomarkers of disease, but their impact on daily functioning and memory remains modest for many. Meanwhile, established medications for memory impairment—like donepezil and memantine—continue to provide the most consistent improvements in patient-reported quality of life. As such, while novel memory drugs are promising, they are currently best viewed as adjuncts rather than replacements for existing standards of care.
Other experimental approaches include serotonin modulators, anti-inflammatory compounds, and even repurposed diabetes drugs like metformin, which have shown early promise in small studies. While these agents are not yet classified as mainstream memory loss medication, they highlight the growing recognition that dementia may have metabolic, vascular, and inflammatory underpinnings—offering a wider lens through which to approach treatment.
Personalizing Dementia Therapies: What Is the Best Prescription Medicine for Memory Loss?
Determining the best prescription medicine for memory loss depends on a constellation of factors: the specific dementia subtype, the progression stage, coexisting psychiatric symptoms, and the patient’s tolerance to side effects. For example, in cases of Lewy body dementia, traditional memory medications may worsen hallucinations or exacerbate motor symptoms, necessitating careful titration and alternative strategies. In vascular dementia, where blood flow to the brain is compromised, dementia treatments often include both cognitive enhancers and cardiovascular drugs to manage underlying risk factors.
Patients with comorbid anxiety or depression may benefit from the strategic use of SSRIs in combination with memory drugs. This is where combinations like Exelon with Namenda to help with anxiety can become particularly useful, creating a more comprehensive therapeutic effect. Additionally, behavioral symptoms such as aggression, paranoia, or agitation—common in later stages—may require adjunct medications, though the use of antipsychotics in dementia is approached with extreme caution due to increased risk of stroke and mortality.
Thus, answering the question “what is the best prescription medicine for memory loss” necessitates a nuanced approach. It is rarely a matter of choosing a single agent. Rather, it involves building a medication regimen that addresses the unique cognitive, emotional, and behavioral profile of each individual.
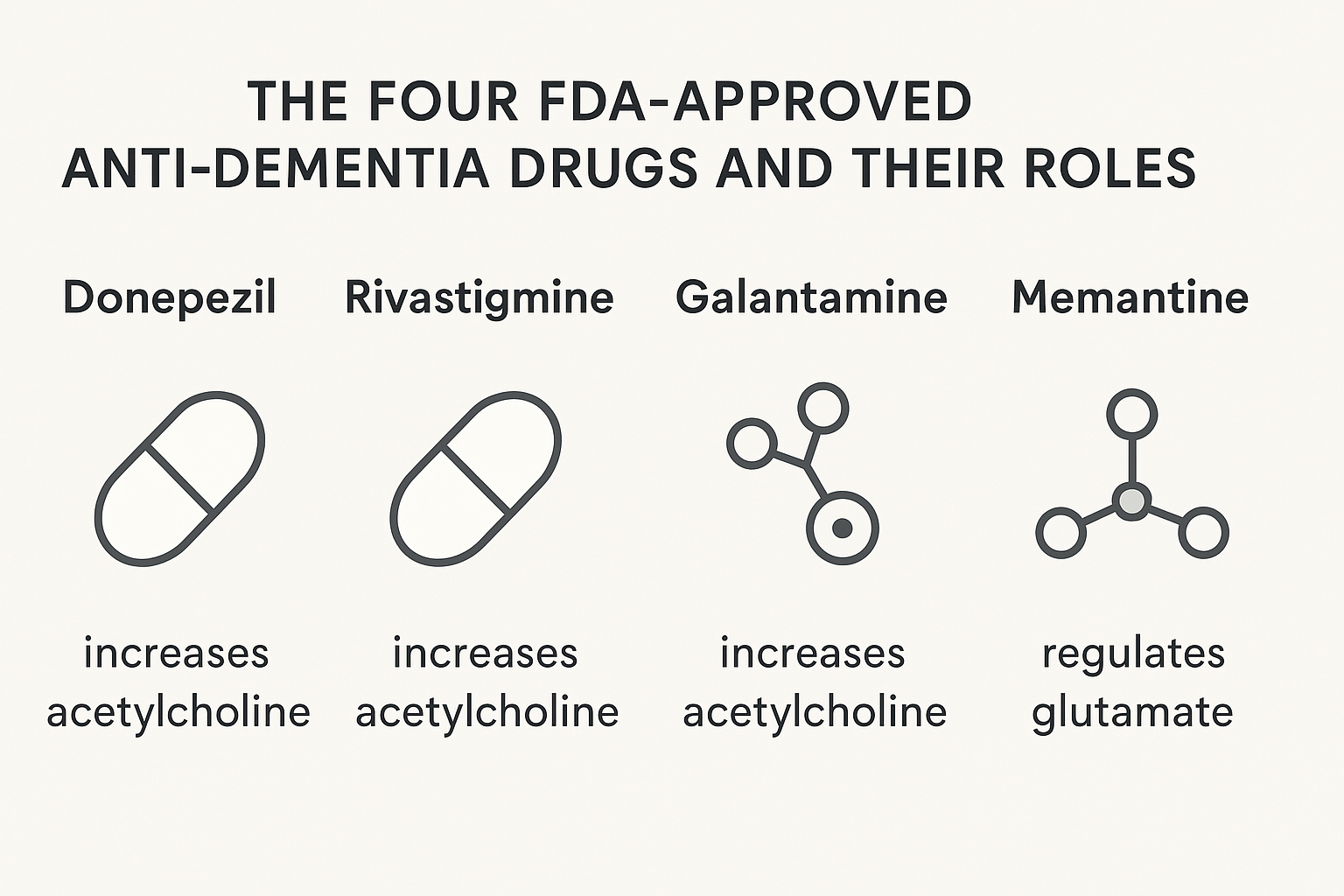
The Four FDA-Approved Anti-Dementia Drugs and Their Roles
As of today, four primary FDA-approved medications constitute the foundation of pharmacologic dementia therapies: donepezil, rivastigmine, galantamine, and memantine. These 4 anti dementia drugs form the pharmacological backbone of dementia care in the United States. Each has a well-documented safety and efficacy profile, and each offers distinct advantages depending on the patient’s needs and disease stage.
Donepezil is often the first-line treatment due to its once-daily dosing and broad use across all stages of Alzheimer’s. Rivastigmine offers flexibility with its transdermal patch, which is particularly helpful for patients with swallowing difficulties or gastrointestinal sensitivity. Galantamine, with its dual mechanism of enhancing acetylcholine and modulating nicotinic receptors, may provide an edge in certain cognitive domains. Memantine, meanwhile, is the go-to option for moderate to severe dementia, frequently used in tandem with the other agents.
While these drugs are not curative, they remain the most evidence-supported options currently available. When families ask, “is there a cure for dementia?” the honest answer is no—but that doesn’t mean there is no hope. Medications can significantly delay progression, reduce caregiver burden, and improve patient engagement in meaningful daily activities.
Beyond Pills: How to Treat Dementia Holistically
While pharmacological interventions are central to dementia care, effective treatment often requires a broader lens. The best approach for how to treat dementia involves a multimodal strategy: combining memory loss drugs with lifestyle modification, cognitive rehabilitation, physical exercise, and social engagement. Music therapy, reminiscence therapy, and environmental modifications are just a few examples of non-pharmacologic interventions that can enhance outcomes when paired with dementia pills.
Nutrition also plays a crucial role. Diets rich in antioxidants, omega-3 fatty acids, and anti-inflammatory foods have shown promise in slowing cognitive decline. Addressing sleep disturbances, sensory deficits (like hearing or vision loss), and pain management are also vital components of care, particularly in reducing behaviors such as agitation and withdrawal. For patients who experience physical symptoms such as discomfort or migraines, knowing how to treat dementia headaches becomes another critical layer of intervention.
Thus, while dementia medications are a cornerstone, they are most effective when integrated into a holistic care plan tailored to the patient’s medical, emotional, and social context.
Evaluating Risk vs. Benefit: Is There Medication for Dementia That Is Always Effective?
One of the challenges of dementia pharmacotherapy is the variability in patient response. Some individuals experience notable improvements in memory, mood, or behavior within weeks of starting a new medication. Others may see only modest benefits or even adverse reactions. This inconsistency often leads to difficult decisions around continuing, adjusting, or discontinuing drugs for dementia.
When patients and caregivers ask, “is there medicine for dementia that works for everyone?” the answer, unfortunately, is no. Human brains are incredibly complex, and dementia is not a uniform disease. What helps dementia in one person may have little effect in another. Still, medications for memory impairment remain a critical tool, especially when used judiciously and monitored regularly by experienced clinicians.
Clinicians often employ a trial-and-error approach—starting with a single agent, assessing response, and adjusting based on symptomatology. Meds for memory loss are not magic bullets, but they can be powerful allies in maintaining quality of life when prescribed thoughtfully and used in tandem with non-drug interventions.
Frequently Asked Questions (FAQ): Understanding Dementia Medications and Treatments
1. How are dementia medications personalized to individual patient needs?
Dementia medications are increasingly prescribed with precision, accounting for each patient’s unique symptom profile, stage of progression, and coexisting health conditions. For instance, while some individuals may respond well to standard memory medication like donepezil, others with significant behavioral symptoms may require an integrated approach combining dementia pills with antidepressants or antipsychotics. When managing emotional symptoms, physicians often turn to a regimen such as Exelon with Namenda to help with anxiety, providing cognitive support while targeting mood. Additionally, patients with comorbidities like heart disease or diabetes may face restrictions on certain memory loss drugs due to interactions. As a result, dementia therapies are rarely one-size-fits-all; they must be carefully curated, regularly reviewed, and adapted to reflect changing clinical realities.
2. Are there non-cognitive benefits to using dementia treatments long-term?
Yes, beyond cognitive stabilization, many dementia treatments contribute to improved emotional regulation, sleep quality, and social engagement. Medications for memory impairment have been associated with reduced caregiver burden and enhanced patient participation in daily routines, which can significantly elevate quality of life. For example, certain dementia therapies may mitigate irritability and agitation, common behavioral symptoms in mid-to-late stages. In such cases, the use of memory drugs isn’t solely to enhance recall but also to foster a more predictable and comforting environment. Long-term use of meds for memory loss can thus influence relational dynamics within families, easing tensions and reducing emotional distress.
3. What new dementia drugs are currently under investigation?
Current research into memory drugs is exploring groundbreaking avenues beyond conventional acetylcholinesterase inhibitors and NMDA antagonists. Monoclonal antibodies targeting amyloid-beta and tau proteins—such as lecanemab and donanemab—aim to modify disease progression by addressing core pathologies. These agents may eventually reshape how clinicians approach dementia treatments, especially if early intervention proves to slow decline. While these experimental drugs for dementia show promise, questions remain about accessibility, long-term efficacy, and adverse effects. Other areas of interest include neuroinflammatory modulators and metabolic therapies, such as intranasal insulin or GLP-1 receptor agonists, reflecting the evolving view that dementia involves more than memory loss alone.
4. How do lifestyle and behavioral interventions complement dementia medications?
Even the best prescription medicine for memory loss is most effective when paired with a structured and supportive environment. Lifestyle strategies such as cognitive stimulation therapy, aerobic exercise, and music therapy have been shown to synergize with medications for memory impairment. Moreover, patients who receive both pharmacological and non-pharmacological support often experience delayed institutionalization and improved mood. Integrating routine physical activity can even enhance the pharmacokinetics of certain dementia medications, improving their bioavailability. Thus, when determining how to treat dementia comprehensively, a dual-pronged strategy that includes both meds for dementia and psychosocial enrichment often yields the best results.
5. Are dementia medications safe for older adults with multiple health conditions?
While most dementia medications are generally well tolerated, older adults with polypharmacy concerns must be closely monitored. For example, drugs for dementia can sometimes exacerbate cardiovascular issues, trigger gastrointestinal upset, or interfere with sleep. Adjusting dosage and monitoring for interactions is crucial, particularly when memory loss medication is combined with blood pressure or anticoagulant therapies. In these populations, clinicians often favor treatments like the Exelon patch to reduce systemic side effects. This highlights the importance of personalized dementia treatments that are mindful of the broader medical context in which memory drugs are being administered.
6. Can dementia medications improve executive functioning or just memory?
Although memory is the primary target, many dementia medications also offer benefits for executive functioning, including attention, planning, and problem-solving. For instance, patients on NMDA antagonists like memantine often show improvements in judgment and task initiation. This expanded impact is particularly useful for those navigating daily tasks independently or semi-independently. Understanding what helps dementia from an executive perspective is crucial for caregivers and clinicians alike, as it affects everything from medication adherence to safety awareness. As research progresses, the search for what is the best drug to improve memory is increasingly becoming a question about how to enhance overall cognitive architecture.
7. What factors influence the discontinuation of memory loss drugs?
Discontinuation decisions are multifactorial and involve a nuanced assessment of benefits versus risks. Some patients may develop side effects like bradycardia or nausea, prompting a reassessment of their medication regimen. In others, a plateau in effectiveness may suggest that continuing certain dementia pills offers limited value. Additionally, advanced-stage dementia patients may experience diminished absorption or responsiveness, which impacts how to treat dementia in its later phases. Clinicians and families often collaborate to reevaluate whether ongoing use of dementia therapies aligns with the goals of care, focusing on comfort, dignity, and quality of life.
8. How does the combination of Exelon with Namenda to help with anxiety work mechanistically?
The pairing of Exelon with Namenda to help with anxiety operates through dual neurotransmitter pathways. Exelon increases acetylcholine levels, which supports cognition and emotional regulation, while Namenda modulates glutamate to reduce overstimulation of neurons. This combination has been particularly useful for patients exhibiting both memory loss and anxiety-driven agitation. By targeting these neurochemical imbalances simultaneously, this regimen can stabilize mood without the need for sedatives, which often carry higher risks in elderly populations. It reflects a growing trend toward multi-modal dementia medications that address not just memory loss, but also the affective symptoms that often accompany it.
9. Is there any cure for dementia, or do treatments only manage symptoms?
Currently, there is no definitive cure for dementia, but that doesn’t equate to a lack of progress. While memory loss drugs cannot reverse damage, they can stabilize cognition, delay progression, and reduce behavioral symptoms. Promising disease-modifying therapies are in development, and early intervention is showing greater potential than ever before. Understanding whether or not is there a cure for dementia often depends on how we define the term; if the goal is total reversal, the answer remains no. However, if the goal is to preserve function, improve quality of life, and slow decline, then today’s dementia treatments offer more hope than ever.
10. How do clinicians approach treating physical symptoms like headaches in dementia patients?
Addressing physical symptoms such as headaches in individuals with dementia requires both medical precision and a deep understanding of behavioral cues. Since patients may struggle to verbalize discomfort, changes in behavior—like withdrawal, aggression, or pacing—can signal pain. In such cases, determining how to treat dementia headaches involves ruling out environmental triggers, reviewing medication side effects, and sometimes using low-dose analgesics. It’s also important to distinguish between vascular headaches and tension-type headaches, particularly in those with vascular dementia. This facet of care underscores that dementia medications must be part of a broader, compassionate approach that considers all aspects of the patient’s well-being.
Final Reflections: What Is the Best Treatment for Dementia in Today’s Medical Landscape?
So, what is the best treatment for dementia in 2025? While the perfect cure remains elusive, our understanding of how to treat this condition has evolved significantly. The combination of cholinesterase inhibitors and NMDA antagonists—along with personalized strategies that incorporate medications like Exelon with Namenda to help with anxiety—can offer meaningful improvements. Among the 4 anti dementia drugs currently approved, none stand alone as a silver bullet, yet together they provide a therapeutic framework that has helped millions retain function and dignity.
When considering what are the 3 most commonly prescribed drugs for dementia, the answer usually includes donepezil, rivastigmine, and memantine. These agents continue to anchor most treatment protocols, supported by a growing awareness of the need to personalize care. Whether the goal is to address behavioral symptoms, improve cognition, or simply make daily life more manageable, there are now more tools than ever to support patients and caregivers alike.
Even in the absence of a cure, the answer to the question “can dementia be cured” is not without hope. Science is advancing, therapies are becoming more targeted, and clinical trials offer glimpses of what the future may hold. Until then, the thoughtful application of memory medication—guided by evidence and empathy—remains one of our most powerful means of addressing this formidable condition. For those wondering what is the best medication for dementia, the most accurate answer is this: it depends, but there is always something we can do to help. And that itself is a powerful step toward healing.
Further Reading:
The Latest Advances in the Diagnosis and Treatment of Dementia
Alzheimer’s: Medicines help manage symptoms and slow decline