Dementia is a complex and progressive neurological condition that impacts not only the individual diagnosed but also those who care for them. Often, the burden of care falls on family members who must navigate the emotional, physical, and logistical challenges of caregiving, usually with little to no formal training or support. These individuals, known as dementia caregivers, are the unsung heroes of an increasingly prevalent public health crisis. As the global population ages, the number of people living with dementia is expected to rise dramatically, making the role of caregivers more vital than ever. This article explores the multifaceted challenges dementia caregivers face, the essential support structures needed to sustain them, and the expert-backed strategies to ensure their well-being is prioritized alongside that of the individuals they care for.
You may also like: How to Prevent Dementia and Alzheimer’s Disease Naturally: Expert-Backed Strategies to Reduce Your Risk Through Lifestyle and Diet
Understanding the Realities of Dementia Caregiving
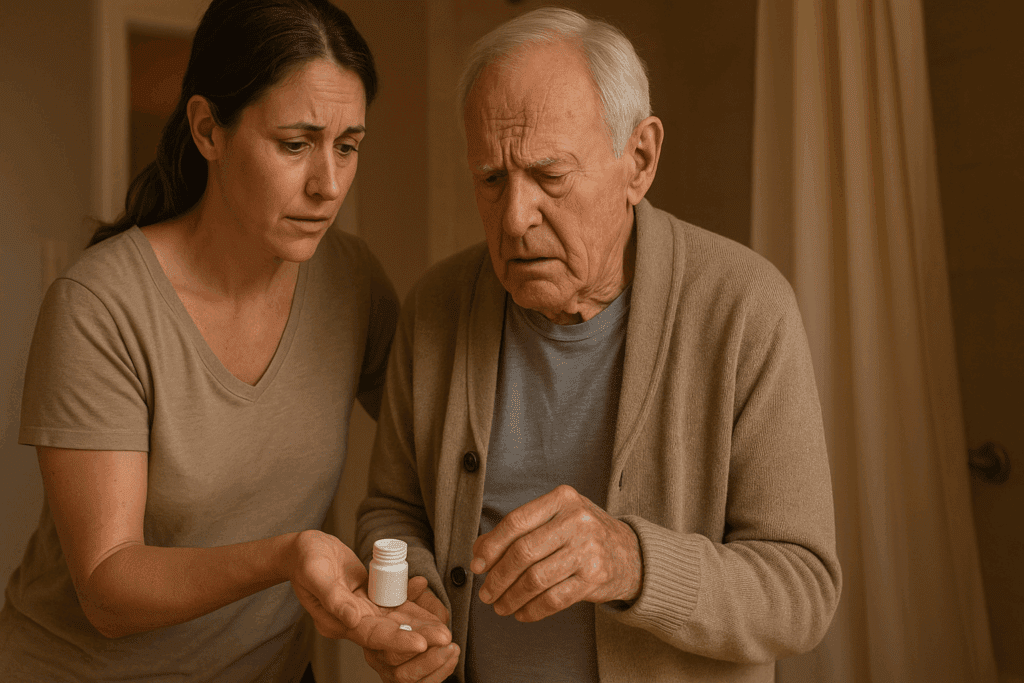
For many dementia caregivers, the role begins subtly and intensifies over time. It may start with helping a loved one remember appointments or manage medications, but as the disease progresses, the demands grow exponentially. Caregivers often become responsible for daily tasks such as bathing, dressing, feeding, and managing behavioral changes, many of which are emotionally taxing and physically exhausting. One of the most significant challenges dementia caregivers face is the emotional toll of witnessing a loved one lose their cognitive abilities. This psychological burden can lead to feelings of grief, frustration, and helplessness.
Furthermore, dementia caregivers frequently experience social isolation. The demands of caregiving can limit opportunities for social engagement, professional advancement, and self-care. A lack of understanding from friends and even healthcare professionals can exacerbate this isolation, leaving caregivers to navigate complex emotional terrain alone. Research consistently shows that caregivers for individuals with dementia are at heightened risk for depression, anxiety, and chronic health issues, underscoring the urgent need for meaningful dementia caregiver support systems.

The Role of Family Dynamics and Emotional Labor
Caregiving rarely occurs in a vacuum. Family dynamics heavily influence how responsibilities are distributed and perceived. In many cases, one family member—often a spouse or adult child—assumes the primary caregiving role. This can create tension among siblings or other relatives, especially if there are disagreements about care decisions or financial responsibilities. The emotional labor involved in being the primary caregiver is immense. In addition to managing the physical aspects of care, these individuals often serve as advocates, decision-makers, and emotional anchors for the entire family.
This emotional labor is frequently undervalued or invisible. Unlike tasks with clear outcomes, such as managing medications or scheduling appointments, emotional labor involves navigating feelings—both one’s own and those of the person with dementia. It includes calming anxiety, managing behavioral outbursts, and maintaining a sense of normalcy in the face of decline. Alzheimer caregiver roles, in particular, are often burdened with the added challenge of handling aggressive or unpredictable behavior, which can increase stress and strain familial relationships. Recognizing and addressing this emotional component is a critical part of providing comprehensive help for dementia caregivers.
Navigating Healthcare Systems and Legal Complexities
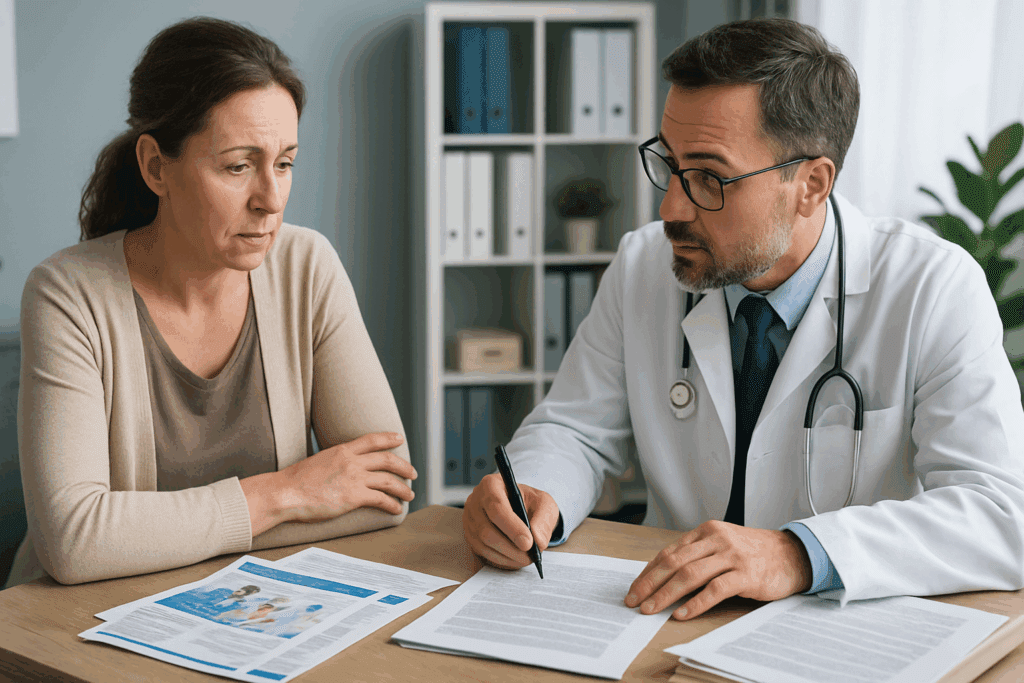
One of the most daunting aspects of being a dementia caregiver is interacting with healthcare systems and navigating the legal landscape. Caregivers must often coordinate multiple appointments, ensure that medications are correctly administered, and advocate for the best possible care—tasks that require not only time but a sophisticated understanding of healthcare terminology and bureaucracy. Without proper support, caregivers may feel overwhelmed, especially when encountering medical professionals who do not specialize in dementia care.
Legal considerations further complicate the caregiver’s role. From establishing powers of attorney to making decisions about long-term care and guardianship, Alzheimer caregiver responsibilities extend into realms that can be both intimidating and confusing. Without proper guidance, caregivers may find themselves making critical decisions under duress, often with limited information or conflicting advice. Therefore, it is essential that dementia caregiver support include legal and financial planning resources to reduce uncertainty and empower caregivers to make informed choices.
Emotional and Psychological Impacts on Caregivers
The emotional strain of caregiving cannot be overstated. Prolonged exposure to stress without adequate coping mechanisms can lead to what is commonly referred to as caregiver burnout. Symptoms may include chronic fatigue, irritability, insomnia, and even physical health problems such as high blood pressure and weakened immunity. The emotional weight of this role is intensified by ambiguous loss—a psychological term used to describe the grief experienced when a loved one is physically present but psychologically absent.
Many dementia caregivers report feeling as though they are mourning a person who is still alive. This form of grief is difficult to articulate and often misunderstood by those outside the caregiving sphere. When left unaddressed, it can contribute to a profound sense of loneliness and despair. Building emotional resilience through therapy, support groups, and mindfulness practices can help caregivers manage these complex feelings. It is critical that help for dementia caregivers include access to mental health services tailored specifically to the unique challenges they face.

Community-Based Support and Peer Networks
Isolation is one of the most insidious challenges dementia caregivers face, making community-based support systems indispensable. Peer support networks, whether online or in person, provide a space where caregivers can share experiences, offer advice, and receive emotional validation from those who truly understand their situation. These networks often serve as a lifeline, offering practical solutions and emotional sustenance in equal measure.
Organizations such as the Alzheimer’s Association offer extensive resources, including local support groups, educational workshops, and respite care programs. These community-based services are especially valuable for first-time caregivers who may feel lost or unprepared. Access to peer networks can also help caregivers reframe their experiences, moving from a place of isolation to one of shared strength. Establishing strong connections within the community is a cornerstone of sustainable dementia caregiver support.
The Importance of Respite Care and Self-Care
Respite care—temporary relief provided by professional caregivers or volunteers—plays a crucial role in maintaining caregiver health. It allows dementia caregivers to take breaks, attend to personal needs, or simply rest, knowing their loved one is in capable hands. Without these intervals, caregivers may find themselves spiraling into exhaustion, ultimately compromising the quality of care they provide.
However, many caregivers struggle with guilt when taking time for themselves, perceiving it as a betrayal or failure of duty. Changing this mindset is essential. Just as flight attendants instruct passengers to secure their own oxygen masks before helping others, caregivers must recognize that their well-being is foundational to their effectiveness. Incorporating self-care practices—whether it’s a walk in nature, a coffee with a friend, or time spent pursuing a hobby—can rejuvenate the spirit and prevent burnout. Structured support systems should explicitly promote and facilitate these opportunities as part of comprehensive help for dementia caregivers.

Training and Education as Empowerment Tools
Knowledge is power, particularly when confronting a disease as multifaceted as dementia. Many caregivers are thrust into their roles with little preparation, forced to learn on the job through trial and error. This can be frustrating and potentially dangerous, as improper techniques or misunderstanding symptoms can lead to unintended harm. Structured education and training programs can provide a solid foundation, enhancing caregivers’ competence and confidence.
Effective training covers a range of topics, including communication strategies, behavioral management, nutrition, and mobility assistance. For Alzheimer caregiver roles specifically, specialized knowledge about the stages of the disease and symptom progression is critical. Training not only equips caregivers with practical skills but also demystifies the condition, reducing fear and anxiety. Furthermore, educational programs that offer certification or continuing education credits can serve as valuable credentials, particularly for those seeking to formalize their caregiving roles or transition into professional caregiving careers.
The Financial Toll of Dementia Caregiving
While the emotional and physical demands of caregiving are well-documented, the financial burden is often underappreciated. Dementia caregivers frequently incur out-of-pocket expenses for medical supplies, home modifications, transportation, and additional professional care. In some cases, caregivers must reduce work hours or leave the workforce entirely, leading to lost income and diminished retirement savings.
These financial strains can have long-term consequences, particularly for those caring for loved ones over many years. Policies that offer tax credits, stipends, or direct compensation for family caregivers can help alleviate some of this pressure. Additionally, helping caregivers navigate insurance policies, government programs, and nonprofit assistance can empower them to make informed financial decisions. As part of a holistic approach, dementia caregiver support must include financial planning and resource allocation tailored to individual needs.
Recognizing Cultural and Socioeconomic Factors in Caregiving
Culture plays a pivotal role in shaping caregiving practices and expectations. In some communities, caregiving is viewed as a sacred duty, while in others it may be seen as a shared responsibility among extended family members. Socioeconomic factors further influence the availability of resources, with low-income caregivers often facing additional barriers such as limited access to healthcare, transportation, and professional respite services.
To be effective, support systems must be culturally competent and sensitive to these diverse realities. This includes providing multilingual resources, engaging community leaders, and acknowledging varying attitudes toward mental health and elder care. Help for dementia caregivers must be inclusive, addressing not only the universal challenges of caregiving but also the unique burdens shaped by cultural and economic contexts. Only then can support initiatives truly serve all who need them.
Advocating for Policy Change and Systemic Reform
Individual efforts, while essential, are not sufficient to address the broader challenges faced by dementia caregivers. Systemic reform is necessary to create an environment where caregivers are recognized, respected, and adequately supported. Advocacy plays a critical role in driving these changes. Caregivers, healthcare professionals, and concerned citizens must work together to push for policies that expand access to resources, improve caregiver training, and ensure fair compensation.
Legislation such as the RAISE Family Caregivers Act represents a step in the right direction, mandating the development of national strategies to support caregivers. However, much work remains. Comprehensive dementia caregiver support requires integrated efforts across healthcare, legal, financial, and community domains. By raising awareness and advocating for change, society can begin to shift from a reactive to a proactive stance, ensuring that caregivers receive the recognition and support they so clearly deserve.
Looking Ahead: Innovations and Opportunities in Dementia Caregiving
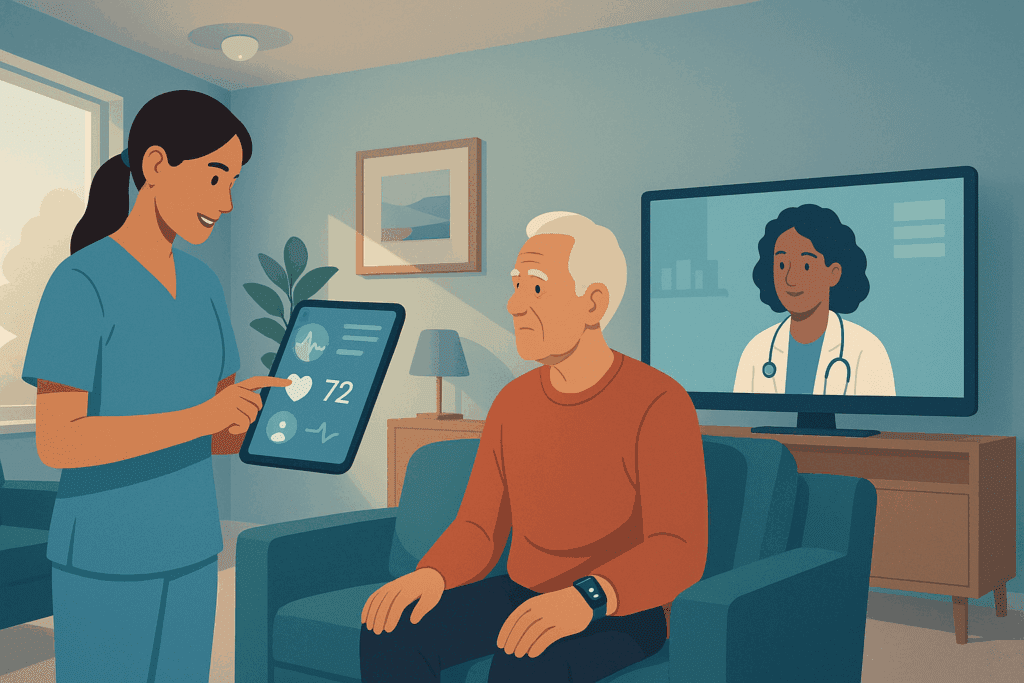
As technology and research continue to advance, new opportunities are emerging to support dementia caregivers more effectively. Innovations such as smart home monitoring systems, wearable health trackers, and telehealth platforms can ease the burden of care and enhance safety for individuals with dementia. These tools can provide real-time updates, reduce emergency incidents, and allow caregivers to monitor their loved ones from a distance.
Equally important is the growing field of dementia-friendly community design. From public transportation systems to retail environments, creating inclusive spaces can reduce caregiver stress and promote independence for those with dementia. In the realm of education, virtual reality simulations and gamified training platforms are helping caregivers build empathy and hone their skills in engaging, effective ways. As these innovations become more accessible, they hold the potential to transform the caregiving experience and broaden the scope of dementia caregiver support.
A New Paradigm: Centering the Needs of Dementia Caregivers
Ultimately, the health and sustainability of our caregiving systems depend on acknowledging and addressing the needs of those who provide care. Dementia caregivers are a critical component of the healthcare ecosystem, yet they often go unrecognized and unsupported. To build a truly compassionate and functional society, we must center their experiences in policy, practice, and public discourse. From expanded mental health services to practical training, from financial assistance to culturally attuned resources, help for dementia caregivers must be as multifaceted as the challenges they face.
Caring for someone with dementia is a profound act of love and commitment—but it should not come at the expense of the caregiver’s own health and well-being. By elevating the voices of dementia caregivers and embracing expert-informed strategies, we can build a support system that honors their sacrifice and fortifies their resilience. In doing so, we not only improve the lives of caregivers but also enhance the quality of care for those living with dementia. It is time to shift the narrative from silent suffering to shared support, recognizing that in supporting the supporters, we strengthen the entire fabric of our communities.
Frequently Asked Questions: Expert Answers for Dementia Caregivers
1. What are some overlooked sources of stress for dementia caregivers that might go unrecognized?
While physical exhaustion and emotional grief are commonly acknowledged, one overlooked source of stress for dementia caregivers is decision fatigue. Constantly making both large and small decisions—ranging from daily routines to long-term care planning—can deplete cognitive resources and lead to burnout. Another source is hypervigilance, where caregivers feel they must remain alert at all times to ensure the safety of their loved one, even during rest. Additionally, subtle social stigma surrounding dementia may isolate caregivers, causing them to withdraw from friendships and support networks. These chronic stressors highlight the importance of targeted dementia caregiver support that addresses not only physical demands but also invisible psychological burdens.
2. How can dementia caregivers maintain their personal identity while managing caregiving responsibilities?
Maintaining a sense of personal identity is one of the most difficult yet essential challenges for dementia caregivers. One effective strategy is setting boundaries by carving out protected time each week for personal hobbies, relationships, or self-reflection. Creating a caregiving journal or blog can also help individuals process experiences while reaffirming their own voice. Joining caregiver support groups that encourage storytelling fosters self-expression beyond the caregiving role. Ultimately, successful help for dementia caregivers must go beyond logistical aid to support emotional self-preservation and identity resilience.
3. Are there specific technologies that can reduce the daily workload of an Alzheimer caregiver?
Yes, the digital health landscape has expanded rapidly, offering a range of technologies to support Alzheimer caregivers. Smart home systems with motion sensors and automated reminders can reduce the need for constant supervision. Wearable devices that monitor vital signs and alert caregivers to irregularities provide peace of mind and enable early intervention. Specialized dementia care apps also help track behaviors, manage medication schedules, and communicate with healthcare professionals. These tools, when integrated into a dementia caregiver support plan, can meaningfully reduce stress and enhance care quality.
4. What are the long-term psychological effects of caregiving that may appear even after the caregiving role ends?
Long after the caregiving journey ends, many former dementia caregivers continue to experience emotional reverberations. Prolonged grief is common, especially when the death of a loved one comes after years of cognitive decline and ambiguous loss. Some may develop symptoms resembling post-traumatic stress disorder (PTSD), including flashbacks or emotional numbness. Others struggle with reintegration into social life or finding a renewed sense of purpose. This underscores the need for post-caregiving services as a critical extension of dementia caregiver support, ensuring caregivers receive help even beyond their active role.
5. How can employers better support workers who are also dementia caregivers?
Employers can play a pivotal role in reducing the dual burden faced by working dementia caregivers. Flex-time policies, remote work options, and extended family leave are all tangible accommodations that can ease logistical strain. Providing Employee Assistance Programs (EAPs) with counseling and caregiving resources adds an emotional and practical layer of support. Employers should also foster open dialogue and educate management on the unique stressors faced by employees in Alzheimer caregiver roles. By institutionalizing flexibility and empathy, workplace cultures can offer critical help for dementia caregivers who are juggling professional and personal responsibilities.
6. In what ways can friends and extended family provide meaningful support to primary dementia caregivers?
Rather than vague offers to “help if needed,” extended family and friends can offer specific, consistent support to dementia caregivers. This might include taking on grocery shopping, providing scheduled companionship visits, or managing administrative tasks like bills or insurance paperwork. Emotional validation is equally important—simply listening without judgment can alleviate feelings of isolation. Thoughtful gestures such as delivering meals or offering respite hours reinforce a caregiver’s sense of community. For dementia caregiver support to be effective at the grassroots level, it must be built on reliability, empathy, and actionable involvement.
7. How do cultural beliefs shape expectations for dementia caregivers across different communities?
Cultural norms profoundly influence the expectations placed on dementia caregivers. In many collectivist cultures, caregiving is considered a family obligation, and seeking external support might be viewed as neglectful or dishonorable. In contrast, Western societies may emphasize autonomy, potentially leading to quicker institutionalization but also earlier intervention from medical professionals. These cultural paradigms affect everything from how Alzheimer caregiver duties are distributed to which services are considered acceptable. Recognizing and respecting these differences is essential when designing inclusive help for dementia caregivers that truly meets people where they are.
8. What are the implications of caregiver burnout on public health systems?
Caregiver burnout doesn’t just affect individuals—it has ripple effects throughout the public health system. When dementia caregivers experience health breakdowns, they may require hospitalization or mental health services, increasing healthcare costs. Furthermore, declining caregiver effectiveness can lead to earlier institutionalization of dementia patients, which places a greater burden on long-term care facilities. Addressing this cascade effect requires robust dementia caregiver support policies that include preventive mental health care, caregiver education, and systemic acknowledgment of caregiver labor as a public health asset.
9. Are there emerging trends in caregiver training that go beyond traditional methods?
Yes, the future of dementia caregiver education is rapidly evolving with the integration of experiential and tech-driven models. Virtual reality simulations now allow caregivers to experience the world through the lens of someone with dementia, enhancing empathy and practical response skills. Interactive e-learning modules with real-time feedback provide flexible, self-paced training ideal for busy Alzheimer caregivers. Additionally, peer-led workshops and mentorship programs offer personalized insights that formal instruction may miss. As part of innovative help for dementia caregivers, these next-generation training tools are poised to dramatically improve both confidence and competence.
10. How can policymakers better align services to reflect the evolving needs of dementia caregivers?
Policymakers must recognize that the needs of dementia caregivers are not static but evolve over time. Early in the caregiving journey, informational support and diagnosis navigation are essential. As the disease progresses, policies should ensure access to affordable respite care, legal resources, and comprehensive Alzheimer caregiver education. Toward the end stages and beyond, grief counseling and reintegration services become critical. A dynamic, stage-based approach to dementia caregiver support ensures that services remain relevant and impactful throughout the full trajectory of the caregiving experience.
Conclusion: Why Investing in Dementia Caregiver Support Strengthens the Future of Health and Wellness
The road walked by dementia caregivers is often one of quiet sacrifice and unwavering devotion. Yet, in their silence, they sustain a vital pillar of our healthcare system. By understanding the layered burdens they carry—from emotional strain and financial hardship to social isolation and legal complexities—we unlock the ability to design better, more effective support structures. Dementia caregiver support must evolve from being a peripheral concern to a central focus within health and wellness strategies.
Empowering dementia caregivers with education, mental health resources, and respite services not only protects their well-being but also elevates the standard of care for individuals living with dementia. Alzheimer caregivers, in particular, require nuanced guidance, ongoing training, and psychological reinforcement to manage the relentless progression of the disease they confront daily. Community and policy-level changes, inclusive of cultural and socioeconomic realities, are essential to ensure no caregiver feels left behind.
The future of dementia care will depend not just on medical innovation, but on how well we care for those doing the caring. With every resource, reform, and recognition extended to caregivers, we strengthen the moral and medical fabric of society. Help for dementia caregivers is not just a matter of compassion—it is a public health imperative. By centering their needs today, we invest in a healthier, more resilient tomorrow for everyone touched by dementia.


